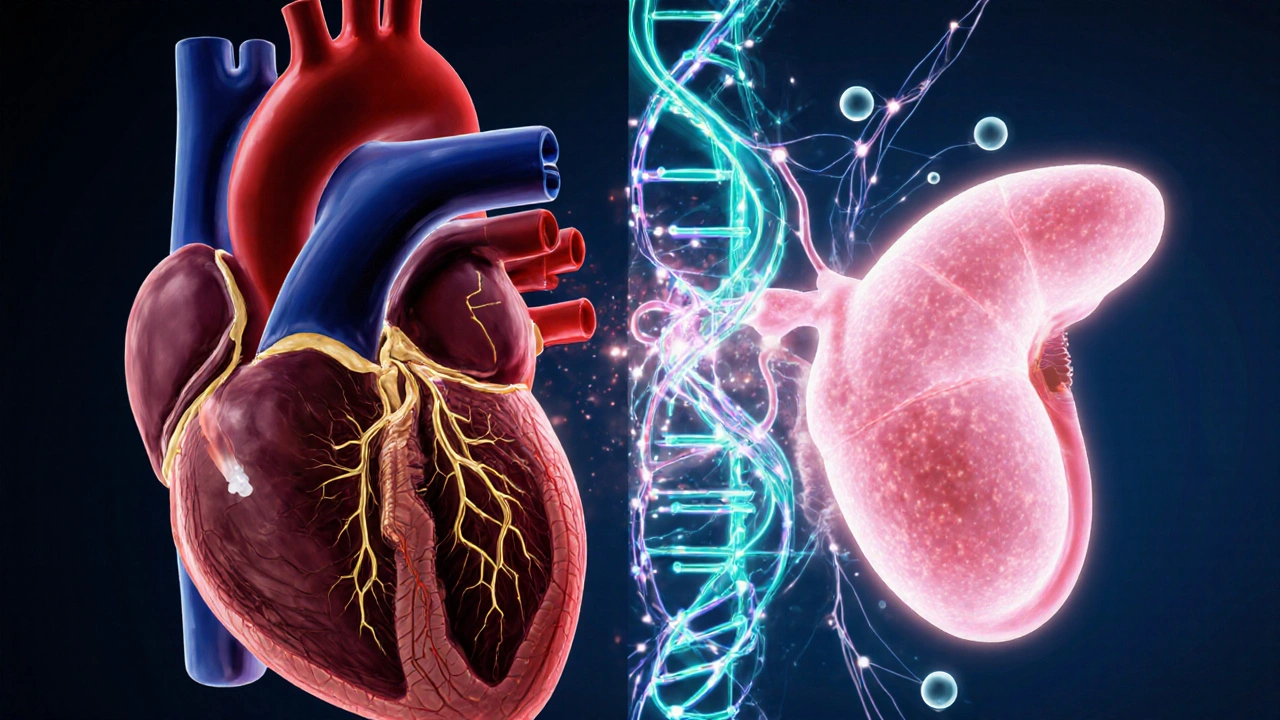
Hypertrophic Subaortic Stenosis is a form of hypertrophic cardiomyopathy where thickened heart muscle blocks blood flow out of the left ventricle. It often presents with a left‑ventricular outflow tract (LVOT) gradient, chest pain, shortness of breath, or fainting episodes. Though traditionally viewed as a purely structural heart disease, growing evidence shows a clear connection with diabetes, especially type 2, that reshapes how clinicians assess risk and treat patients.
Why the Connection Matters
Patients who carry both conditions face a two‑fold increase in cardiovascular events. Diabetes accelerates myocardial fibrosis, worsens LVOT obstruction, and heightens the risk of atrial fibrillation and sudden cardiac death. Recognising this overlap helps cardiologists and endocrinologists tailor screening, medication, and lifestyle plans.
Shared Pathophysiology
Several biological threads weave hypertrophic subaortic stenosis (HSS) and diabetes together:
- Insulin resistance a hallmark of type 2 diabetes promotes maladaptive cardiac remodeling through chronic activation of the renin‑angiotensin‑aldosterone system.
- Elevated glycated hemoglobin (HbA1c) reflects long‑term glucose exposure correlates with increased myocardial collagen deposition, thickening the interventricular septum.
- Genetic mutations such as MYH7 encode β‑myosin heavy chain, a common driver of HSS are more prevalent in families with metabolic syndrome, suggesting a shared hereditary substrate.
These mechanisms converge on myocardial fibrosis, impaired relaxation, and heightened sympathetic tone-exactly the milieu that fuels LVOT obstruction.
Clinical Impact: What Changes for the Patient?
When diabetes co‑exists with HSS, clinicians notice several predictable shifts:
- Earlier onset of symptoms. Diabetic patients often report exertional dyspnea in their 40s, a decade earlier than non‑diabetic HSS peers.
- Higher prevalence of atrial fibrillation. Studies from 2023 show a 30% increase in AF incidence among diabetic HSS cohorts.
- Elevated risk of sudden cardiac death (SCD). The combined presence of diabetes and a maximal LVOT gradient >50mmHg raises 5‑year SCD risk to roughly 6% versus 3% in isolated HSS.
These data push the threshold for implantable cardioverter‑defibrillator (ICD) consideration lower in diabetics, especially when HbA1c exceeds 8%.
Diagnostic Nuances
Imaging remains the cornerstone, but diabetes adds layers of complexity.
- Echocardiography provides real‑time assessment of septal thickness and LVOT gradient may underestimate obstruction in patients with diabetic microvascular disease because of reduced tissue Doppler signal quality.
- Cardiac MRI offers high‑resolution tissue characterization, detecting fibrosis via late gadolinium enhancement is especially valuable for diabetic HSS patients; a fibrosis burden >15% strongly predicts adverse outcomes.
- Laboratory monitoring should include fasting glucose, HbA1c, and lipid profile every 3‑6months to gauge metabolic control.
Management Strategies: Aligning Cardiac and Metabolic Care
Therapeutic goals split into two tracks: relieving LVOT obstruction and optimising glycaemic control.
| Aspect | Non‑Diabetic HSS | Diabetic HSS |
|---|---|---|
| First‑line drug | Beta‑blocker (e.g., propranolol) | Beta‑blocker + Metformin (if eGFR≥45ml/min) |
| Second‑line drug | Disopyramide or calcium‑channel blocker | Calcium‑channel blocker (avoid non‑dihydropyridines that can worsen glucose) |
| Invasive option | Septal myectomy or alcohol septal ablation | Same, but ensure tight glucose control pre‑procedure to reduce wound infection |
| Risk mitigation | ICD if LVOT>50mmHg + syncope | ICD threshold lowered if HbA1c>8% or fibrosis>15% |
| Lifestyle focus | Low‑intensity aerobic exercise | Combined aerobic + resistance training to improve insulin sensitivity |
Key medication interactions deserve attention. Beta‑blockers reduce heart rate and contractility can mask hypoglycaemic symptoms, so diabetic patients must monitor glucose more frequently. Conversely, Metformin improves insulin sensitivity without causing hypoglycaemia is generally safe and may even attenuate myocardial hypertrophy.
Emerging Research and Future Directions
Recent trials (2024-2025) explore sodium‑glucose cotransporter‑2 (SGLT2) inhibitors as adjuncts in HSS. Preliminary data suggest a modest reduction in LVOT gradient and fibrosis scores, possibly through anti‑inflammatory pathways. Gene‑editing approaches targeting MYBPC3 mutations linked to HSS are still experimental, but they open a window to treat the root cause rather than just symptoms.
On the metabolic side, continuous glucose monitoring (CGM) combined with wearable ECG patches is being evaluated for early detection of arrhythmias in diabetic HSS patients. Early alerts could prompt timely ICD placement or medication adjustment.
Practical Checklist for Clinicians
- Screen all HSS patients for diabetes (fasting glucose, HbA1c).
- Perform cardiac MRI when LVOT gradient >30mmHg and diabetes is present.
- Use beta‑blockers cautiously; educate patients about blunted hypoglycaemia warning signs.
- Consider metformin as part of the baseline regimen unless contraindicated.
- Re‑evaluate ICD candidacy if HbA1c >8% or fibrosis >15%.
- Prescribe combined aerobic‑resistance exercise; aim for 150min/week moderate activity.
- Monitor for atrial fibrillation with periodic Holter or wearable ECG, especially if glycaemic control is poor.
Related Topics Worth Exploring
Understanding the HSS-diabetes link naturally leads to other areas:
- Metabolic syndrome and its impact on other forms of cardiomyopathy.
- Autonomic neuropathy in diabetes and its effect on heart rate variability.
- Role of lifestyle medicine in reducing LVOT gradients without surgery.
- Genetic counselling for families with MYH7 or MYBPC3 mutations.

Frequently Asked Questions
Does having diabetes increase the severity of hypertrophic subaortic stenosis?
Yes. Diabetes accelerates myocardial fibrosis and can raise the left‑ventricular outflow tract gradient, leading to earlier symptom onset and higher risk of arrhythmias.
Should I get a cardiac MRI if I have both conditions?
A cardiac MRI is strongly recommended when LVOT gradients exceed 30mmHg and diabetes is present, because it detects fibrosis that echocardiography can miss.
Can standard beta‑blockers be used safely with diabetes?
They can be used, but patients need to check blood sugar more often since beta‑blockers may mask hypoglycaemic symptoms. Pairing with metformin often balances heart‑rate control and glucose management.
Is an ICD more likely for diabetic HSS patients?
Guidelines suggest a lower threshold for ICD implantation when HbA1c is above 8% or when cardiac MRI shows fibrosis over 15% because both factors elevate sudden cardiac death risk.
Do SGLT2 inhibitors help with the heart issues in HSS?
Early trials indicate SGLT2 inhibitors may modestly reduce LVOT gradients and improve myocardial energetics, but they are not yet standard of care for HSS. Consultation with both cardiology and endocrinology is advised.
What type of exercise is safe for someone with HSS and diabetes?
Low‑ to moderate‑intensity aerobic activity (e.g., brisk walking, cycling) combined with resistance training 2‑3 times a week improves insulin sensitivity without provoking high LVOT gradients. Always get clearance from a cardiologist first.




September 27, 2025 AT 00:52
Great info, thanks for sharing! 😊