Understanding the Role of Lincomycin in COPD Treatment
If you've battled the dragon called Chronic Obstructive Pulmonary Disease (COPD) or know someone who has, you're likely familiar with a good friend of ours: Lincomycin. The world of pharmaceuticals may be more tangled than a teenager’s room after a weekend with friends, but that's exactly where I come in. You see, Lincomycin, this mysterious friend of ours, has made a striking comeback in COPD management. And today, we’ll shine a light on it, brighter than your 450 lumens camping flashlight.
Breaking down COPD and Lincomycin: the Dynamic Duo
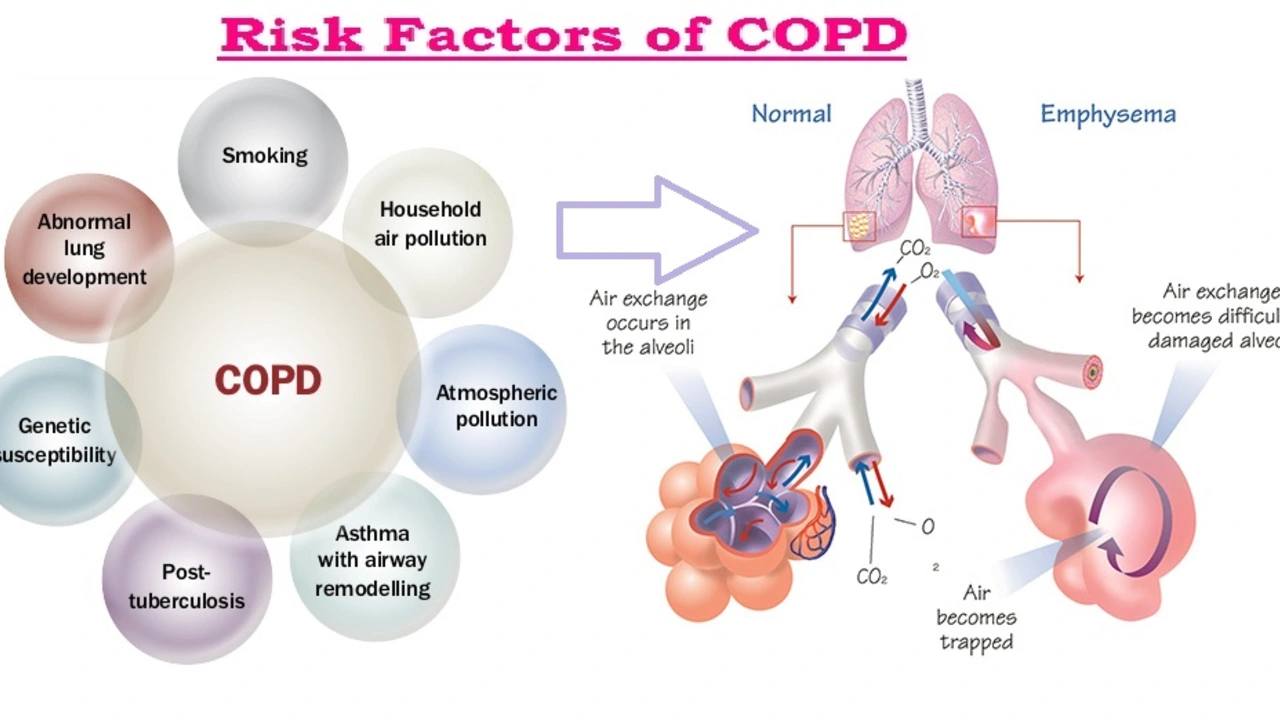
First off, let's poke around COPD. With more baggage than most reality TV stars, COPD isn't just a condition, it's a collection. Chronic bronchitis, severe emphysema, you name it. But Lincomycin, our superhero, has shown some promising effects in treating this ailment. Now, it's no One Direction, because there is a direction we need to head in when we opt for Lincomycin treatment: up! Up on the ladder of hope, health, and huffing-less!
Unfurling the Magic Carpet of Lincomycin’s Mechanism
"How does it work?" you ask, leaning over the edge of your seat. Let me share a story. Just like Game of Thrones, our bodies are full of different kingdoms (read: cells). When harmful intruders, our body's very own White Walkers (read: bacteria), start making trouble, our white blood cells are the Night's Watch, fighting them off. Lincomycin, ladies and gents, enhances their effort by inhibiting the growth of the troublemakers. It's much like recruiting Jon Snow into your team, but only much, much more effective!
Navigating the Course – Dosage and Administration
What's that? You want more specifics? Well, aren't you in luck! The recommended dosage for Lincomycin, a Spartacus that bellows - 'I am here to fight for you,' typically lies between 500 mg to 2 grams daily, depending on the severity of the condition. Administration is usually intramuscular or intravenous, but like a kangaroo with a hidden pouch, this medicine could also be taken orally.
Sidekick Woes: Side Effects and Precautions
Superheroes often come with their own baggage; even our friendly neighborhood Lincomycin isn't spared. Think nausea, vomiting, diarrhea. Some people experience skin rashes or changes in white blood cells. On the brighter side, a study also found that people taking Lincomycin don't turn into Spock or grow an extra thumb, so we got that going on for us. Be sure to consult a healthcare professional because - and I say this in the most caring and professional way possible - you definitely don't want to try this at home!
Livin’ La Vida Lincomycin: Stories from the Frontline
You know what? I wasn't always this muscular bodybuilder-turned-writer who loves analogies as much as a koala loves eucalyptus leaves. I had my own tussle with COPD. When I was first introduced to Lincomycin, I thought it was spelled "Link Comic Sin," like a chain of hilariously sinful comics of the world, but soon after I realized you shouldn't judge a drug by its pronunciation. It has since proven to be a valuable tool in my fight against COPD, a real Thor's hammer to my respiratory woes.
Looking Into the Future: Ongoing Research and Developments
As they say, the universe isn't done surprising us. Lincomycin, despite its brewing comeback, is still a hot topic in the labs. Studies suggest that it may play an even bigger role in respiratory infections. We may soon see a day when Lincomycin tops the charts again, beating The Beatles to their own game in the pharmaceutical world.
So there you have it, my dear COPD warriors and curious comrades! That's your crash course on Lincomycin for COPD management. So the next time you find yourself in a heated discussion about antibiotics and COPD, you can confidently chime in, 'Aha! But have you heard of Lincomycin?' Cheers to being better informed and to healthier lungs!




November 8, 2023 AT 20:06
Oh sure, because every antibiotic magically cures COPD, right?