Understanding Tacrolimus and Its Use in Transplant Medicine
Tacrolimus, also known as FK506, is a potent immunosuppressive drug that is commonly used in transplant medicine to prevent organ rejection. In this section, we will explore the basic pharmacology of Tacrolimus, its mechanism of action, and why it is an essential medication in pediatric transplant patients. Understanding the role of Tacrolimus in pediatric transplant patients is crucial for healthcare providers, as it is a cornerstone in the management of these patients.
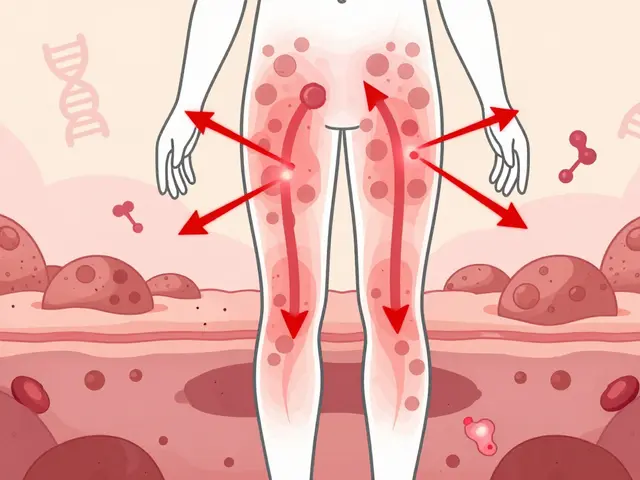
Tacrolimus is a macrolide compound derived from the bacterium Streptomyces tsukubaensis. It works by inhibiting the enzyme calcineurin, which is necessary for the activation of T-cells, a type of white blood cell that plays a significant role in the immune system. By inhibiting T-cell activation, Tacrolimus effectively suppresses the immune response, reducing the risk of organ rejection in transplant patients.
The Importance of Immunosuppression in Pediatric Transplant Patients
Organ transplantation is a life-saving procedure for many children with end-stage organ failure. However, the body's natural immune response can pose a threat to the transplanted organ, as it may recognize the new organ as foreign and attack it, leading to organ rejection. This is where immunosuppressive medications like Tacrolimus come into play.
Immunosuppressive therapy is an essential part of post-transplant care, as it helps to prevent acute and chronic organ rejection. This is especially important in pediatric transplant patients, as they often have a more robust immune response than adults. By suppressing the immune system, Tacrolimus allows the transplanted organ to function without being attacked by the recipient's immune cells.
Monitoring Tacrolimus Levels in Pediatric Patients
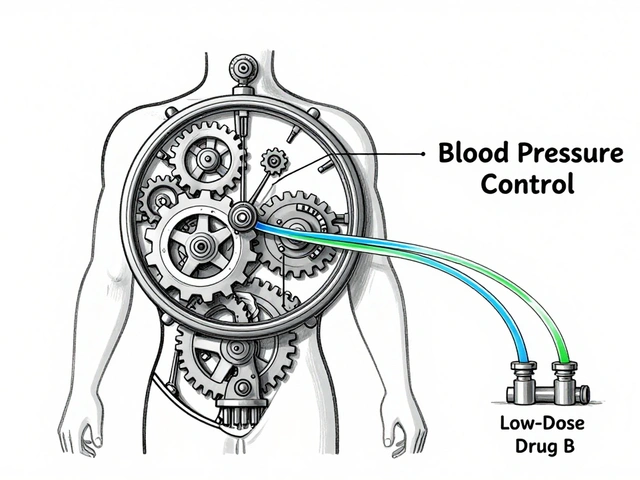
One of the challenges in using Tacrolimus in pediatric transplant patients is maintaining the appropriate drug levels in the bloodstream. The therapeutic window for Tacrolimus is narrow, meaning that there is a fine balance between providing enough immunosuppression to prevent organ rejection and avoiding the potential side effects of the drug.
Monitoring Tacrolimus levels in pediatric patients involves regular blood tests to ensure that the drug concentration remains within the target range. This can be challenging in children, as factors such as age, weight, and organ type can all influence the appropriate dosage. Close collaboration between healthcare providers, patients, and their families is essential for successful Tacrolimus therapy in pediatric transplant patients.
Managing Side Effects of Tacrolimus in Pediatric Patients
While Tacrolimus is a critical component of immunosuppressive therapy in pediatric transplant patients, it is not without potential side effects. Some common side effects of Tacrolimus include hypertension, nephrotoxicity, neurotoxicity, and an increased risk of infection due to the suppression of the immune system.
Managing side effects in pediatric patients requires close monitoring by healthcare providers, as well as ongoing communication with patients and their families. In some cases, adjustments to the Tacrolimus dosage or the addition of other medications may be necessary to minimize side effects while maintaining adequate immunosuppression.
Long-Term Management of Pediatric Transplant Patients on Tacrolimus
Given that many pediatric transplant patients will require lifelong immunosuppressive therapy, long-term management of these patients on Tacrolimus is essential. This includes regular follow-up appointments with healthcare providers, ongoing monitoring of Tacrolimus levels, and management of any side effects that may arise.
Additionally, educating patients and their families about the importance of medication adherence and the potential consequences of non-adherence is crucial. Non-adherence to immunosuppressive therapy can lead to organ rejection and graft loss, so ensuring that pediatric transplant patients and their families understand the importance of taking Tacrolimus as prescribed is vital to the long-term success of the transplant.
Improving Outcomes for Pediatric Transplant Patients with Tacrolimus
In conclusion, Tacrolimus plays a critical role in the management of pediatric transplant patients. By providing effective immunosuppression and reducing the risk of organ rejection, Tacrolimus has significantly improved the outcomes for these patients. However, the successful use of Tacrolimus in pediatric transplant patients requires careful monitoring, management of side effects, and a strong emphasis on medication adherence.
Through ongoing research and collaboration, healthcare providers continue to refine the use of Tacrolimus in pediatric transplant patients, working towards the ultimate goal of improving the quality of life and long-term outcomes for these children.




May 27, 2023 AT 14:56
Honestly, the whole hype around tacrolimus in kids is overrated, and most of the so‑called "experts" are just pushing pharma money. I read the article and it feels like a copy‑paste from a textbook with zero real world insight. The narrow therapeutic window that they babble about is a nightmare for any parent trying to keep a schedule, especially when the dosage has to be tweaked every few weeks. There’s hardly any mention of the daily struggle families face with blood draws-no one talks about kids screaming in the clinic while the nurse tries to draw blood from a trembling arm. And let’s not forget the side effects: hypertension, nephrotoxicity, neuro‑toxicity-yeah, great, just what a child needs besides a new organ. You’d think after all the research, there’d be some alternative, but nope, we’re stuck with a drug that’s as fickle as a cat. The article also breezes past adherence issues, assuming every family has the resources to monitor levels constantly. In reality, many families live in rural areas with limited access to labs, making regular monitoring a logistical nightmare. The author mentions collaboration between providers and families, but in practice, communication breaks down the moment the transplant team leaves the hospital. Also, the piece glosses over the psychological toll on children who have to swallow pills that taste like metal. I’ve seen kids develop aversions to all medication because of this. And the financial burden? Not addressed at all-immunosuppressants are pricey, and insurance doesn’t always cover the full cost. Finally, there’s no discussion about long‑term outcomes beyond survival; what about quality of life, growth, or cognitive development? All in all, this article feels like a polished brochure, not a gritty reality check for families dealing with pediatric transplants.