When you’re nursing, every pill you take feels like a gamble. You’re not just thinking about yourself anymore-you’re thinking about your baby. So when allergies hit or a headache won’t quit, you ask: antihistamines and pain relievers while nursing-are they safe? The answer isn’t a simple yes or no. It depends on which one you pick, how much you take, and how often. The good news? Many common medications are perfectly fine. The bad news? Some can sneak into breast milk and cause real problems for your baby.
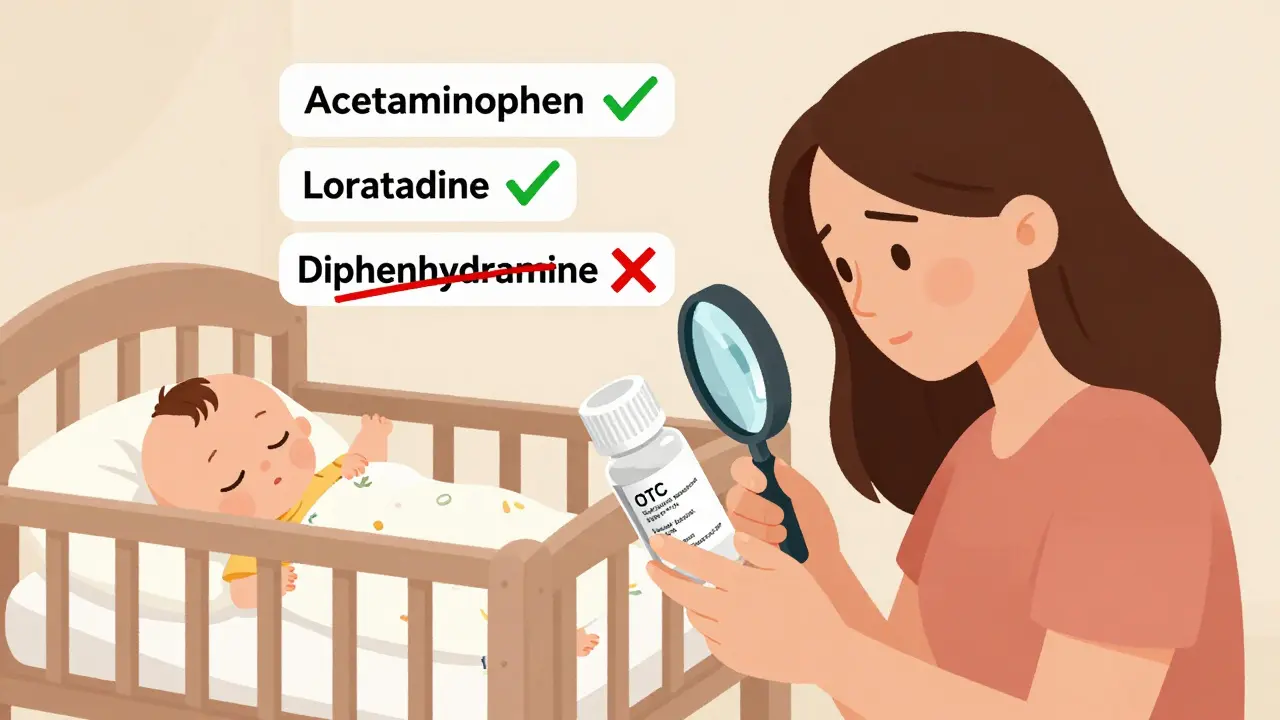
Not All Antihistamines Are Created Equal
There are two big groups of antihistamines: the old-school ones and the newer ones. The old ones-like diphenhydramine (Benadryl), chlorpheniramine, and promethazine-are sedating. They make you drowsy. And they can make your baby drowsy too. In fact, there are documented cases where babies of moms taking these regularly became overly sleepy, missed feeds, and didn’t gain weight properly. That’s not just inconvenient-it’s dangerous.Why? These drugs cross the blood-brain barrier easily. They’re small, fat-soluble molecules that slip into breast milk in higher amounts. One study showed that a baby could get up to 1% of the mother’s dose from diphenhydramine. That’s enough to slow down a newborn’s breathing or make them too sleepy to nurse well.
The newer antihistamines-loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-are different. They’re designed to stay out of the brain. They’re larger, bind tightly to proteins in your blood, and barely make it into breast milk. Loratadine transfers at just 0.04% of the maternal dose. Fexofenadine? Only 0.02%. That’s practically nothing. Multiple studies and clinical guidelines, including those from the American Academy of Family Physicians and the Mayo Clinic, list these as safe for breastfeeding. No reports of drowsiness, poor feeding, or developmental issues in babies.
So if you’re choosing between Benadryl and Claritin? Go with Claritin. Always.
Pain Relievers: The Clear Winners
For pain, fever, or inflammation, you have two top-tier options: acetaminophen and ibuprofen. Both are considered among the safest medications you can take while nursing.Acetaminophen (Tylenol) shows up in breast milk at about 1-2% of your dose. That’s so low, no studies have ever linked it to any side effects in babies. It’s the go-to for postpartum pain, headaches, and even mild fevers. You can take it every 4-6 hours as needed, up to the maximum daily dose.
Ibuprofen (Advil, Motrin) is even better in some ways. It’s highly protein-bound, meaning most of it stays in your bloodstream. Only 0.6-0.8% ends up in milk. Plus, it breaks down quickly-half of it is gone from your body in just two hours. That means your baby gets even less. The American Academy of Family Physicians specifically lists ibuprofen as a preferred option for nursing mothers.
What about other painkillers? Stay away from naproxen (Aleve). It sticks around in your system for up to 17 hours. Studies show it transfers at 7% of your dose-much higher than ibuprofen. There are reports of babies developing bleeding, anemia, or vomiting after prolonged exposure. Codeine, hydrocodone, oxycodone, and tramadol? These are opioids. They can cause dangerous breathing problems in infants. Even small amounts can lead to life-threatening sedation. The FDA has issued warnings about codeine in nursing mothers. Skip them unless your doctor says otherwise-and even then, use the lowest dose for the shortest time.
What About OTC Cold and Allergy Mixes?
This is where things get tricky. Most cold and allergy medicines aren’t just one drug-they’re combinations. A bottle labeled “Allergy & Sinus Relief” might contain pseudoephedrine, diphenhydramine, and acetaminophen. All three.Pseudoephedrine (Sudafed) is a decongestant. It’s not an antihistamine, but it can reduce milk supply if taken regularly. One study showed a 24% drop in milk volume after a single 60mg dose. If you’re already struggling with supply, skip it.
Diphenhydramine? As we said-it’s risky. Even if the label says “non-drowsy,” check the ingredients. Many “daytime” formulas still sneak in sedating antihistamines. Always read the small print. Look for “loratadine,” “cetirizine,” or “fexofenadine” as the antihistamine. Avoid anything with “diphenhydramine,” “chlorpheniramine,” or “promethazine.”
And here’s a big one: many OTC pain relievers include antihistamines too. So if you’re taking Tylenol Cold + Flu, you’re not just getting acetaminophen-you’re getting diphenhydramine. That’s a problem.
What If You Have to Use a Riskier Medication?
Sometimes, you don’t have a choice. Maybe your allergies are so bad that only Benadryl helps. Or you had surgery and need a stronger painkiller. That doesn’t mean you have to stop nursing.Here’s what to do:
- Take the medication right after nursing, not before. That gives your body time to clear most of it before the next feed.
- Use the lowest effective dose. Don’t double up. Don’t take it more often than directed.
- Watch your baby closely for 24-48 hours. Signs of trouble: unusual sleepiness, trouble latching, weak suck, fewer wet diapers, or fussiness.
- If you’re on something like codeine or tramadol, talk to your doctor about alternatives. If you must use it, consider pumping and dumping for 12-24 hours after the dose.
And never, ever take something without checking with your doctor or a lactation consultant-even if it’s “just an OTC pill.”
What About Topical or Nasal Treatments?
Good news: if you can avoid swallowing the drug, you reduce the risk even more. Nasal sprays like fluticasone (Flonase) or azelastine (Astelin) are mostly absorbed locally. Very little enters your bloodstream, so even less goes into milk. Same with eye drops or skin creams. These are usually safe, even if they contain antihistamines or steroids.Just avoid applying creams to your breasts right before nursing. Wash them off if you do.

When to Call Your Doctor
You don’t need to panic every time you take a pill. But if your baby shows any of these signs after you start a new medication, call your pediatrician or lactation consultant:- Sleeping more than usual or hard to wake for feeds
- Not having at least 6 wet diapers a day
- Poor feeding or refusing the breast
- Unusual fussiness, jitteriness, or vomiting
- Slow weight gain or weight loss
These aren’t common with safe medications-but they can happen with the wrong ones.
Bottom Line: What’s Safe to Take
Here’s what you can confidently use while nursing:- Antihistamines: Loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra)
- Pain relievers: Acetaminophen (Tylenol), ibuprofen (Advil, Motrin)
- Topical/nasal: Fluticasone spray, azelastine spray, hydrocortisone cream (avoid breasts)
Here’s what to avoid:
- Antihistamines: Diphenhydramine (Benadryl), chlorpheniramine, promethazine
- Pain relievers: Naproxen (Aleve), codeine, tramadol, oxycodone, hydrocodone
- Combination cold meds: Unless you’ve checked every ingredient and confirmed it’s safe
Remember: your body is designed to feed your baby. Most medications don’t interfere with that. But some do-and you deserve to know which ones. Always check with a pharmacist or lactation specialist before starting anything new. And if you’re unsure, wait for a safer option. Your baby’s health is worth the extra step.
Can I take Benadryl while breastfeeding?
It’s not recommended. Benadryl contains diphenhydramine, a first-generation antihistamine that can make your baby drowsy, interfere with feeding, and even affect milk supply. If you must use it, take the lowest dose possible right after a feeding and monitor your baby closely for sleepiness or poor feeding. Safer alternatives like loratadine or cetirizine are available and preferred.
Is Tylenol safe for breastfeeding moms?
Yes, acetaminophen (Tylenol) is considered one of the safest pain relievers for breastfeeding mothers. Only 1-2% of your dose enters breast milk, and no adverse effects have been reported in nursing infants. It’s commonly used for headaches, fever, and postpartum pain without issue.
Can ibuprofen reduce my milk supply?
No, ibuprofen does not reduce milk supply. In fact, it’s one of the few pain relievers proven safe and effective for nursing mothers. It transfers into breast milk at very low levels (0.6-0.8% of your dose) and clears quickly from your body. It’s often recommended over naproxen, which has a higher risk of side effects in babies.
Are allergy shots safe while breastfeeding?
Yes, allergy shots (immunotherapy) are safe during breastfeeding. They don’t enter breast milk and don’t affect your baby. If you were already receiving them before pregnancy or breastfeeding, you can continue without interruption. If you’re starting them now, discuss timing with your allergist, but there’s no need to delay treatment.
What if I need a prescription painkiller after delivery?
Talk to your doctor about alternatives to opioids. Acetaminophen and ibuprofen are often enough for postpartum pain. If you need something stronger, ask for the lowest effective dose of a short-acting opioid like oxycodone, and avoid codeine or tramadol entirely. Take it right after nursing, and watch your baby for signs of sedation-like excessive sleepiness or trouble latching. Never take more than prescribed.
Can I use nasal sprays with antihistamines while nursing?
Yes, nasal antihistamine sprays like azelastine (Astelin) are generally safe. Since they’re applied locally and not swallowed, very little enters your bloodstream-or your breast milk. They’re often preferred over oral antihistamines because they target symptoms without systemic effects. Just avoid spraying near your breasts or nipples.





January 13, 2026 AT 17:24
Just wanted to say this post saved my sanity. I was about to grab Benadryl for my allergies last week until I saw this. Went with Zyrtec instead-no drowsiness for me, and my baby slept like a angel. Seriously, thank you for laying it all out so clearly.