When you stand up from a chair, your body should automatically adjust your blood pressure to keep you from feeling dizzy or fainting. But for people with autonomic neuropathy, that automatic response breaks down. Blood pressure plummets, the heart races, and sometimes you just collapse. At the same time, food sits in the stomach for hours, bloating and vomiting become daily struggles, and bowel movements turn erratic-sometimes constipated, sometimes explosive. This isn’t just "feeling off." It’s a neurological disorder quietly wrecking internal systems most people never think about.
What Exactly Is Autonomic Neuropathy?
Autonomic neuropathy damages the nerves that control your body’s automatic functions-things like heart rate, digestion, blood pressure, sweating, and bladder control. These nerves don’t respond to your will. They work in the background, like a silent engine. When they’re damaged, your body loses its ability to regulate itself.
Diabetes is the main cause, responsible for 85-90% of cases. High blood sugar over years slowly eats away at these tiny nerves and the blood vessels that feed them. But it’s not just diabetes. Autoimmune diseases, certain chemotherapy drugs like vincristine, viral infections like Guillain-Barré, and neurodegenerative conditions such as Parkinson’s can also trigger it. The National Institute of Diabetes and Digestive and Kidney Diseases estimates that 60-70% of people with diabetes have some level of autonomic nerve damage-but only about 20% show clear symptoms. That means many cases go unnoticed until something serious happens.
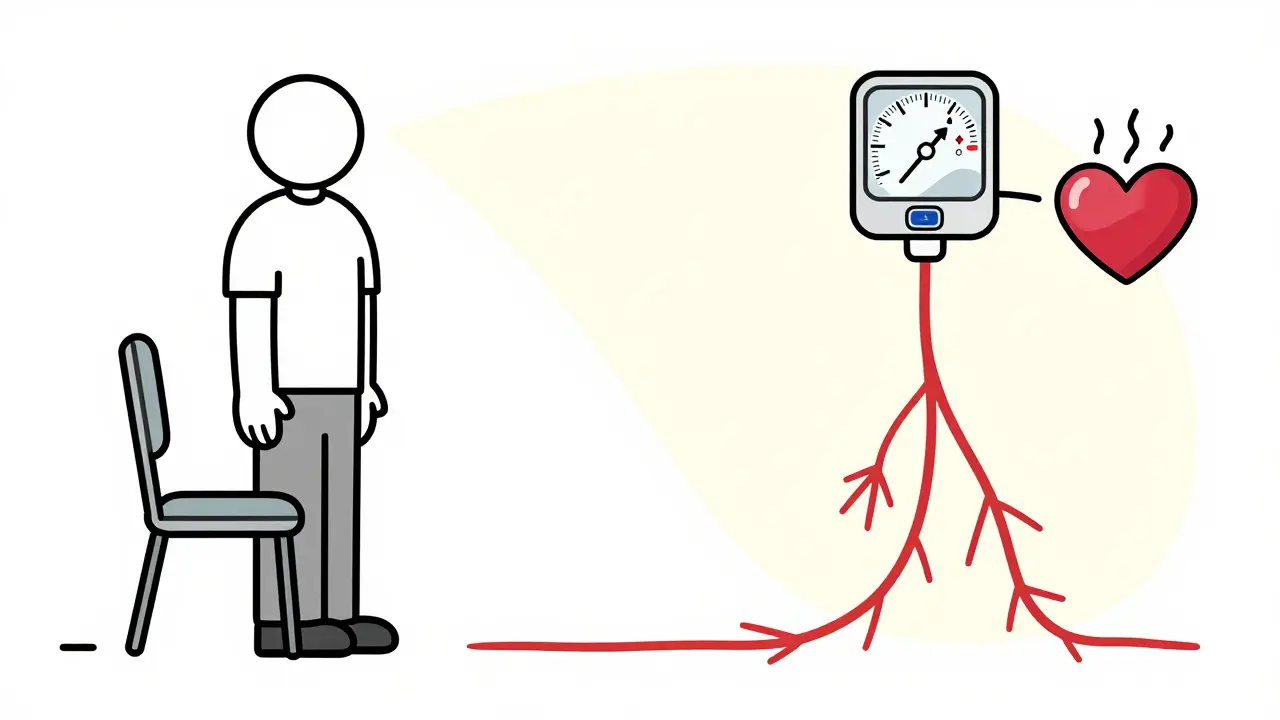
Why Your Blood Pressure Drops When You Stand Up
Standing up should trigger a reflex: your blood vessels tighten, your heart beats a little faster, and your blood pressure stays steady. In autonomic neuropathy, that reflex fails. The sympathetic nervous system-the part that says "hold the line"-stops working properly.
This is called orthostatic hypotension. It’s defined as a drop in systolic blood pressure of at least 20 mmHg or diastolic of 10 mmHg within three minutes of standing. In severe cases, systolic pressure can plunge 35 mmHg or more. A 2021 study of 450 patients found 68% experienced systolic pressure below 90 mmHg when standing. That’s dangerously low.
People describe it as sudden lightheadedness, tunnel vision, or feeling like they’re going to black out. Some faint. Others just feel drained, with brain fog that lasts for minutes after standing. One patient on Reddit described it: "My BP dropped from 120/80 to 85/55 in 30 seconds. I’d collapse if I didn’t sit right back down."
Not everyone gets low blood pressure. Some develop POTS-Postural Orthostatic Tachycardia Syndrome. Instead of blood pressure dropping, their heart rate spikes. A rise of 30 beats per minute or more within 10 minutes of standing, without a significant BP drop, is the hallmark. POTS affects 1-3 million Americans, mostly women aged 15-50. It’s controversial whether POTS is a separate condition or part of the autonomic neuropathy spectrum. Some experts say yes; others say it’s just one variation of the same problem.
How Your Digestive System Gets Caught in the Crossfire
Autonomic nerves control every step of digestion-from swallowing to stomach emptying to bowel movement timing. When they’re damaged, your gut becomes unpredictable.
Gastroparesis is the most common GI issue. It means your stomach doesn’t empty properly. The standard test is a gastric emptying scan. If more than 10% of food remains in the stomach after four hours, it’s diagnosed. Around 30% of diabetic autonomic neuropathy patients have it. Symptoms? Nausea, bloating, early fullness, and vomiting-often at night. One Mayo Clinic study found 78% of these patients vomited at night, and 45% did it daily.
Constipation is even more common, affecting 60% of patients. Bowel movements drop from the normal 4-5 per week to just 1-2. But then, paradoxically, diarrhea hits. About 25% experience frequent, watery stools-often at night. Many report alternating between constipation and diarrhea. This isn’t IBS. It’s nerve damage causing chaotic muscle contractions in the intestines.
Another hidden problem: SIBO-small intestinal bacterial overgrowth. When the gut doesn’t move food along properly, bacteria overgrow and ferment undigested carbs. A 2021 study found 52% of autonomic neuropathy patients with GI symptoms had SIBO, compared to only 15% in healthy people. It causes bloating, gas, and diarrhea. Breath tests can detect it.
How Doctors Diagnose It
There’s no single blood test. Diagnosis relies on symptoms and specific tests.
For blood pressure issues, the 10-minute active stand test is standard. You lie down for 5 minutes, then stand. Blood pressure and heart rate are checked at 1, 3, 5, and 10 minutes. A drop of 20/10 mmHg confirms orthostatic hypotension.
Heart rate variability testing during deep breathing is another key tool. If your heart doesn’t speed up when you inhale and slow down when you exhale, your autonomic nerves are impaired. The Valsalva maneuver-forcing air out against a closed airway-also tests nerve reflexes. Abnormal results mean trouble.
For GI symptoms, gastric emptying scintigraphy is still the gold standard. But newer tests like the wireless motility capsule-swallowed like a pill-are gaining ground. It tracks pressure and pH as it moves through your gut, giving a full picture with 92% accuracy.
Doctors also use questionnaires like the COMPASS-31, which scores autonomic symptoms from 0 to 100. A score above 30 means significant dysfunction. It’s not perfect, but it’s reliable.
Treatment: What Actually Works
There’s no cure. But symptoms can be managed.
For low blood pressure, fludrocortisone helps by increasing blood volume. It works in 60% of patients, but 35% end up with high blood pressure when lying down-dangerous for the heart. Midodrine tightens blood vessels. It’s effective in 70% of cases, but you have to time the doses carefully to avoid nighttime hypertension. You can’t take it after 6 p.m.
For POTS with rapid heart rate, ivabradine slows the heart without lowering blood pressure. It reduces heart rate by 15-25 bpm in 65% of patients. It’s not a cure, but it gives people back hours of upright time.
For gastroparesis, metoclopramide was the go-to drug. But it carries a black box warning: long-term use can cause irreversible movement disorders. Erythromycin helps short-term, but most patients develop tolerance within weeks.
A better option now is pyridostigmine. Originally used for myasthenia gravis, it improves nerve signaling in the gut. A 2023 guideline found it improved symptoms in 55% of patients with minimal side effects. It’s becoming the first-line choice.
Non-drug approaches are just as important. Compression stockings (30-40 mmHg) reduce blood pooling in the legs and cut orthostatic symptoms by 35%. Abdominal compression garments help with bloating and improve gastric emptying. A 2022 Mayo Clinic trial showed a 40% reduction in symptoms.
Diet changes are critical. Eating six small meals a day instead of three large ones helps. Avoiding fat (under 25g per meal) and fiber (under 10g) reduces stomach delay. One patient wrote: "The low-fat, low-residue diet cut my vomiting from five times a day to once every three days. Worth every social sacrifice."

Life With Autonomic Neuropathy
People with this condition don’t just have medical problems-they lose their lives.
A 2022 survey of 850 patients found 89% avoid hot environments (showers, saunas, summer heat), 76% wear compression gear daily, and 68% increase salt intake. Social life shrinks. 62% say dietary restrictions ruin outings. 55% avoid restaurants because they can’t predict when symptoms will strike.
Diagnosis takes years. The average time from first symptom to correct diagnosis is 4.7 years. Most see three or more doctors before someone listens. Many are told it’s anxiety or "just stress."
Life expectancy drops by 8.2 years compared to diabetics without autonomic neuropathy. That’s not because of the nerve damage alone-it’s because of the cascade: falls from fainting, malnutrition from vomiting, infections from SIBO, heart attacks from unstable blood pressure.
What’s Next?
Research is moving fast. A new NIH trial is testing fecal transplants for GI symptoms. Early results show 40% improvement in quality of life scores. Blood tests measuring neurofilament light chain-a protein released when nerves are damaged-may soon allow diagnosis before symptoms appear.
The American Diabetes Association will soon recommend annual autonomic screening for anyone with diabetes for more than seven years. That could catch half a million new cases early.
And the diagnostic threshold for orthostatic hypotension? It’s changing. Starting in 2025, a systolic drop of just 15 mmHg will count as abnormal-not 20. That means earlier detection, earlier help.
Autonomic neuropathy isn’t rare. It’s hidden. But when you understand the signs-the dizzy spells when standing, the vomiting after meals, the unpredictable bowels-you start seeing it everywhere. It’s not just "getting older." It’s nerve damage. And it needs to be treated like one.
Can autonomic neuropathy be reversed?
No, the nerve damage itself cannot be reversed. But symptoms can be managed effectively with medication, lifestyle changes, and diet. Early detection and strict blood sugar control in diabetic patients can slow or stop further progression. Some patients regain partial function with aggressive treatment, but full recovery is rare.
Is orthostatic hypotension the same as low blood pressure?
No. Low blood pressure (hypotension) is a general term. Orthostatic hypotension is a specific type that happens when you stand up. It’s caused by a failure of the autonomic nervous system to adjust blood pressure quickly. You can have low blood pressure while lying down, but orthostatic hypotension only occurs with posture change.
Why do I get diarrhea and constipation at the same time?
Autonomic neuropathy disrupts the coordinated muscle contractions that move food through the intestines. In some areas, the muscles become too slow, causing constipation. In others, they spasm or contract irregularly, leading to diarrhea. This is called "paradoxical diarrhea." It’s often linked to bacterial overgrowth (SIBO), which worsens the cycle.
Can I still eat fiber if I have gastroparesis?
High-fiber foods delay stomach emptying and can worsen symptoms. The recommended limit is under 10 grams of fiber per day. Focus on cooked vegetables, peeled fruits, and refined grains. Avoid raw veggies, whole grains, nuts, and seeds. A dietitian specializing in gastroparesis can help design a safe meal plan.
How do I know if I have POTS or just autonomic neuropathy?
POTS is a subtype of autonomic neuropathy. If your blood pressure doesn’t drop much when you stand but your heart rate spikes by 30 bpm or more, you likely have POTS. It’s diagnosed with a tilt table test or active stand test. Some experts see POTS as a separate condition, but most agree it falls under the autonomic neuropathy umbrella. Treatment approaches overlap, but ivabradine and beta-blockers are more commonly used for POTS.
Are there any new treatments on the horizon?
Yes. Fecal microbiota transplants (FMT) are being tested for GI symptoms and show promising results. Blood tests measuring neurofilament light chain may soon allow diagnosis before symptoms appear. New drugs targeting nerve regeneration are in early trials. Also, wearable tech that monitors blood pressure and heart rate in real time is being developed to help patients avoid dangerous drops.





January 11, 2026 AT 19:41
I’ve had POTS for five years and this post nailed it. The heart racing without the drop in BP? That’s the nightmare. I used to think I was just anxious until a cardiologist finally did the tilt test. Now I know it’s not "all in my head." I wear compression socks 24/7 and carry electrolyte packets everywhere. It’s exhausting, but at least I’m not alone.