What Is Diabetic Neuropathy?
Diabetic neuropathy is nerve damage caused by years of high blood sugar. It’s not a single condition-it’s a group of nerve problems that happen when glucose stays too high for too long. The most common type is diabetic peripheral neuropathy, which starts in the feet and legs, then can move to the hands and arms. People often notice it first as tingling, burning, or numbness-sometimes so mild they ignore it. But left unchecked, it can lead to serious problems like foot ulcers, infections, and even amputations.
About 60 to 70% of people with diabetes develop some form of neuropathy. Of those, 16 to 26% experience painful diabetic neuropathy (PDN), where the nerve damage causes ongoing, often severe pain. This isn’t just discomfort-it’s life-limiting. Many patients say they can’t sleep, walk, or even wear socks without agony. The good news? You can slow it down, manage the pain, and sometimes even reverse early damage.
Why Blood Sugar Control Is the Foundation
If you do nothing else for your nerves, get your blood sugar under control. It’s not optional-it’s the single most effective way to stop neuropathy from getting worse. The Diabetes Control and Complications Trial (DCCT) proved this back in the 1990s: people who kept their HbA1c below 7% cut their risk of developing neuropathy by 60% compared to those with poor control.
Today, the American Diabetes Association still recommends HbA1c below 7% (53 mmol/mol) as the target. That means fasting blood sugar between 80-130 mg/dL and under 180 mg/dL after meals. Sounds simple, right? But only 14% of people with diabetes actually hit that target. Why? Because it takes daily effort: checking glucose, eating right, moving, and taking meds as prescribed.
Here’s what happens when you improve your numbers: nerves stop getting damaged. In some cases, especially if caught early, numbness and tingling can fade within a year. One Cleveland Clinic study found that 25% of patients saw noticeable improvement in sensation after sticking to tight glucose control for 12 months. That’s not magic-it’s biology. Nerves heal slowly, but they do heal when the stressor (high sugar) is removed.
Medications That Actually Work for Nerve Pain
There’s no cure-all pill, but several medications are proven to help. Only two-pregabalin (Lyrica) and duloxetine (Cymbalta)-are FDA-approved specifically for diabetic nerve pain. But that doesn’t mean others don’t work. In fact, many doctors start with older, cheaper drugs that work just as well.
Amitriptyline, a tricyclic antidepressant, is often the first choice. In clinical trials, 58-63% of patients got at least 50% pain relief. But it comes with trade-offs: drowsiness, dry mouth, weight gain, and heart rhythm risks in older adults. Many people quit because they feel too foggy.
Duloxetine is less sedating but can cause nausea and loss of appetite. In the PRECISION trial, 35% of users had half their pain gone, compared to 18% on placebo. Pregabalin helps too-30-40% of people get significant relief-but it causes dizziness, swelling in the legs, and weight gain. It’s often used when antidepressants don’t work or cause side effects.
For stubborn pain, doctors may turn to tramadol or tapentadol. These are opioid-like drugs. They work, but they’re risky. The CDC says 8-12% of long-term users develop dependence. Nausea and constipation are common. They’re not first-line-they’re last-resort.
And skip the ibuprofen or naproxen. NSAIDs don’t touch nerve pain. Worse, they can hurt your kidneys-already at higher risk in diabetes-and raise your chance of heart problems by 10-20%.
Topical Treatments: Local Relief Without Systemic Side Effects
If you hate pills or can’t tolerate them, try topical options. They deliver pain relief right where it hurts-with almost no effect on the rest of your body.
The capsaicin 8% patch (Qutenza) is a game-changer. It’s applied by a doctor in-office and works by depleting substance P, the chemical that sends pain signals. In trials, 40% of users got at least 30% pain reduction. It lasts up to 3 months per application. No drowsiness. No weight gain. Just localized relief.
Lidocaine patches (5%) are another option. You stick them on painful areas for up to 12 hours a day. They’re safe, cheap, and work well for localized burning or stabbing pain. Many patients use them on their feet at night.
These aren’t magic, but they’re safer than pills for older adults or people on multiple medications. One patient survey at the Cleveland Clinic showed that 65% of people found combining topical treatments with blood sugar control was the most effective approach.

Non-Drug Options: What Really Helps Beyond Pills
Medications don’t fix everything. The real breakthrough comes from lifestyle changes that protect nerves and reduce inflammation.
Exercise is powerful. Walking 30 minutes a day, swimming, cycling, or doing yoga improves blood flow to nerves and helps lower glucose. Many patients say their pain gets worse at first-especially if they’re numb and don’t feel their feet. But stick with it. After a few weeks, movement becomes easier and pain often decreases.
Diet matters too. Cut out processed foods, sugary drinks, and refined carbs. Eat more vegetables, whole grains, lean proteins, and healthy fats. This reduces inflammation, which worsens nerve damage. A Mediterranean-style diet has been linked to slower neuropathy progression.
Stress management is often ignored. Chronic stress raises cortisol, which spikes blood sugar. Mindfulness, deep breathing, and meditation aren’t just “nice to have”-they’re medical tools. One study showed that patients who practiced daily mindfulness had 20% lower pain scores after 8 weeks.
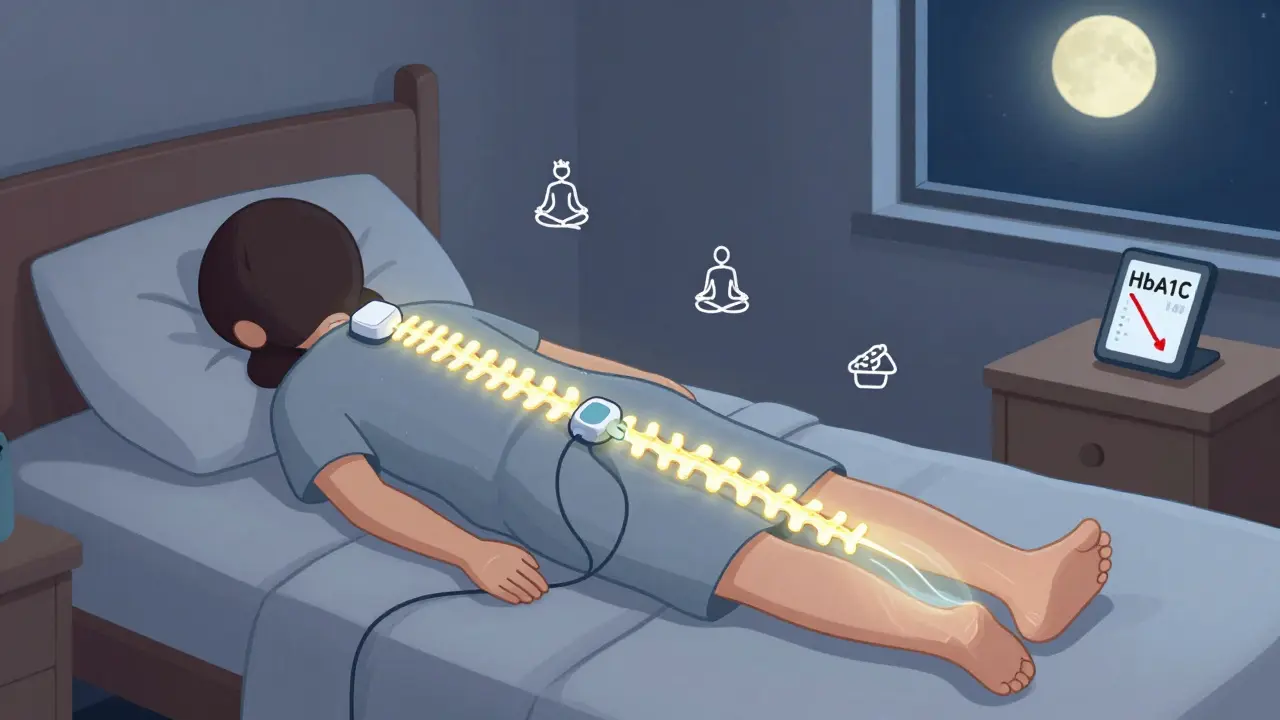
And don’t underestimate TENS units. These small devices send mild electrical pulses through the skin to block pain signals. In a clinical trial, 83% of users saw pain drop from 3.17 to 1.44 on a 5-point scale-compared to just 38% with fake (sham) devices.
Advanced Treatments: When Everything Else Fails
If pain still won’t quit after trying meds, topicals, and lifestyle changes, it’s time to consider advanced options.
Nerve blocks involve injecting numbing medicine near affected nerves. They give fast relief-often within hours-but it lasts only 2 to 6 weeks. Good for flare-ups, not long-term.
Peripheral nerve stimulation (PNS) implants a tiny device under the skin near the painful nerve. It sends gentle pulses to disrupt pain signals. Studies show 50-70% of patients get lasting relief. It’s minimally invasive and reversible.
The most exciting new option? Spinal cord stimulation. It’s been around for decades, but newer models are changing the game. A University of Maryland study found that patients didn’t just feel less pain-they started regaining sensation in numb areas. One man, who hadn’t felt his toes in 8 years, could feel his sock again after 3 months of stimulation. That’s not just pain control. That’s nerve repair.
These aren’t for everyone. They require surgery, cost thousands, and insurance often requires trying everything else first. But for those with severe, unrelenting pain, they can restore quality of life.
What Doesn’t Work-and Why
There’s a lot of misinformation out there. Let’s clear it up.
- Alcohol and smoking: Both make neuropathy worse. Alcohol is toxic to nerves. Smoking narrows blood vessels, starving nerves of oxygen.
- Supplements like B12 or alpha-lipoic acid: Some people swear by them, but large reviews show little to no benefit beyond correcting a true deficiency. Don’t waste money.
- Acupuncture: May help some with pain, but evidence is weak and inconsistent. Not a substitute for proven methods.
- Waiting it out: Neuropathy doesn’t get better on its own. Without control, it progresses.
The truth? There’s no shortcut. Progress comes from consistency-not quick fixes.
How to Know If You’re Making Progress
Improvement isn’t always dramatic. Sometimes it’s subtle:
- Less burning at night
- Being able to wear shoes without pain
- Sleeping through the night
- Walking farther without stopping
- Feeling a light touch on your foot again
Track your pain on a scale of 1 to 10 each week. Write down what you did-meds, exercise, diet, sleep. After 3 months, look back. You’ll see patterns. Maybe your pain dropped after you started walking daily. Maybe it spiked when you skipped your meds. That’s data. That’s power.
And don’t forget your HbA1c. If it’s dropping, your nerves are healing-even if you don’t feel it yet.
When to See a Specialist
See a neurologist or pain specialist if:
- Your pain is getting worse despite treatment
- You’ve lost feeling in your feet and can’t tell if you have a cut or blister
- You’re having trouble walking or balancing
- Medications cause intolerable side effects
- You’re considering nerve stimulation or other advanced treatments
You don’t have to suffer in silence. There are more tools now than ever before.
Final Thought: It’s a Marathon, Not a Sprint
Managing diabetic neuropathy isn’t about finding one magic solution. It’s about layering smart choices: tight blood sugar control, safe medications, movement, stress reduction, and sometimes advanced tech. Most people don’t get 100% relief-but most can get to a point where pain doesn’t control their life.
And here’s the most hopeful part: science is moving fast. Researchers are testing drugs that could actually reverse nerve damage-not just mask pain. In the next 5 to 10 years, we may have treatments that restore sensation, not just reduce discomfort.
Right now, your best weapon is what you can do today: lower your sugar, move your body, and refuse to accept pain as normal. Your nerves are listening. Give them a chance to heal.





January 31, 2026 AT 07:20
I've been managing diabetic neuropathy for 12 years. The capsaicin patch was a game-changer for me. No more daily pills, no brain fog. Just apply it once every few months and my feet stop screaming at night. Seriously, if you're still on gabapentin and feeling like a zombie, try this. Your neurologist might not mention it, but it's in the guidelines.