When you take two drugs at the same time, they don’t just sit quietly in your body. They talk to each other-sometimes helping, sometimes fighting. This isn’t about one drug changing how the other is absorbed or broken down. That’s pharmacokinetics. This is about what happens at the target: the receptors, the cells, the systems where the drugs actually do their job. That’s pharmacodynamic drug interaction-and it’s one of the most dangerous, and often overlooked, reasons people end up in the hospital.
How Drugs Talk at the Receptor Level
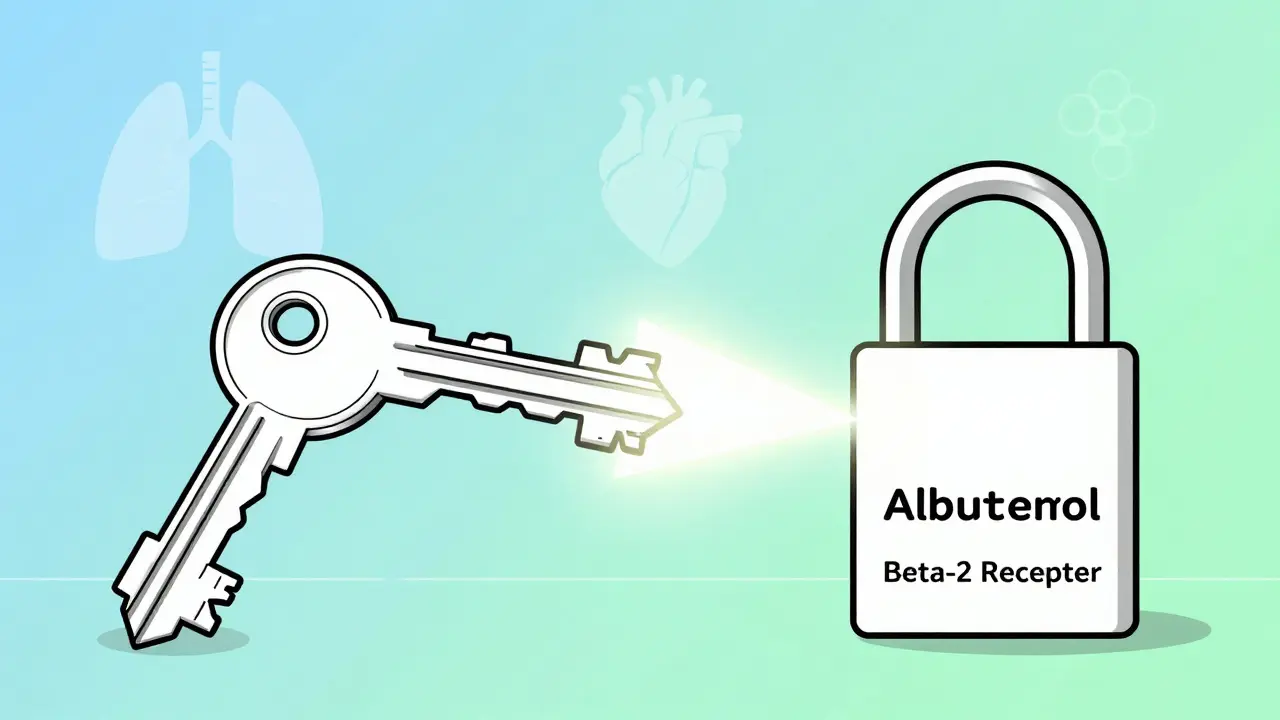
Imagine your body’s receptors as locks. Drugs are keys. When a drug like albuterol (used for asthma) fits into its lock (the beta-2 receptor), it opens the airways. But if you take propranolol-a beta-blocker used for high blood pressure or heart conditions-it’s a key that fits the same lock. It doesn’t just block albuterol. It can completely shut it out. Even if you take the right dose of albuterol, propranolol can make it useless. That’s receptor competition. And it’s not rare. It happens daily in clinics and ERs. The key here is affinity. The drug with higher affinity wins. Propranolol has a stronger grip on the beta receptor than albuterol. So even at low doses, it can override the asthma drug. This isn’t theoretical. In 2021, a patient in Melbourne was admitted with severe bronchospasm after starting propranolol for anxiety. He was on albuterol for years. No one checked the interaction. He nearly needed intubation.Additive, Synergistic, and Antagonistic Effects
Not all drug combinations are bad. Some are designed to work together. Take trimethoprim and sulfamethoxazole. They’re antibiotics that attack bacteria at two different steps in the same pathway. Together, they’re far more powerful than either alone. This synergy lets doctors use lower doses, reducing side effects. Studies show this combo cuts the needed dose of each drug by 75% compared to using one alone. Then there’s additive effects. When two drugs with the same action are combined-like two painkillers that both work on the same brain receptors-their effects simply add up. It’s predictable. But here’s the trap: if you don’t realize you’re doubling down on sedation, you can end up with dangerously low breathing rates. Antagonism is the most dangerous. It’s not just about one drug blocking another. It’s about one drug actively undoing the effect of another. NSAIDs like ibuprofen are a classic example. They’re meant to reduce pain and inflammation. But when taken with an ACE inhibitor like lisinopril (used for high blood pressure), they interfere with kidney function. How? By blocking prostaglandins that help keep blood flowing to the kidneys. A 2019 NIH study showed this drops renal blood flow by 25%. That means the blood pressure drug stops working. The patient’s pressure spikes. Their kidneys get stressed. And they don’t even know why.The Most Dangerous Combinations
Some drug pairs are like loaded guns. One wrong move, and it’s catastrophic. Take SSRIs (like sertraline) and MAOIs (like phenelzine). Both raise serotonin. Together, they can trigger serotonin syndrome-a life-threatening condition with high fever, seizures, muscle rigidity, and confusion. A 2021 meta-analysis found this combo increases serotonin syndrome risk by 24 times. And it’s not just old drugs. Newer antidepressants, even herbal supplements like St. John’s wort, can do the same thing. In 2023, a 72-year-old woman in Sydney was admitted to ICU after combining sertraline with an over-the-counter cough syrup containing dextromethorphan. She didn’t know the risk. Neither did her GP. Another deadly combo: opioids and opioid antagonists. If someone dependent on morphine or oxycodone gets naloxone (used to reverse overdoses), it doesn’t just stop the overdose. It triggers immediate, violent withdrawal. Sweating, vomiting, seizures, heart rhythm problems. It’s terrifying. And it happens more often than you think-especially in patients with chronic pain who are also being treated for addiction. Anticoagulants like warfarin or apixaban combined with antiplatelets like aspirin or clopidogrel? That’s a bleeding risk that skyrockets. A 2022 survey of Australian GPs found 38% of them had seen a patient with major bleeding from this combo. It’s not rare. It’s routine.
Why Pharmacodynamic Interactions Are Harder to Spot
Pharmacokinetic interactions-where one drug changes how another is metabolized-are easier to predict. You can measure blood levels. You can adjust doses. But pharmacodynamic interactions? You can’t measure them in a lab. You can’t see them on a blood test. They only show up when the patient feels worse, or worse-when they collapse. That’s why 68% of serious events from these interactions lead to hospitalization, compared to 42% for pharmacokinetic ones. They’re silent until they’re not. And here’s the kicker: they’re most dangerous with drugs that have a narrow therapeutic index. That means the difference between a helpful dose and a toxic one is tiny. Think digoxin, lithium, warfarin, or antiepileptics. If a drug changes how your body responds to one of these-even slightly-it can tip you over the edge. A 2019 NIH analysis found 83% of life-threatening pharmacodynamic interactions involved at least one drug with a therapeutic index below 3.0. That’s not a big margin for error.What Clinicians Are Doing About It
Technology helps-but it’s not enough. Clinical decision support systems in hospitals catch about 78% of dangerous interactions. But they miss the rest. Why? Because they’re built on simple rules. They don’t understand physiology. They don’t know that NSAIDs reduce kidney perfusion by 25%. They just flag “NSAID + ACE inhibitor” and say “possible interaction.” They don’t tell you how bad it is, or what to do instead. The real solution? Pharmacists. A 2021 review in BMJ Quality & Safety found that when pharmacists reviewed medications for elderly patients, they cut adverse events from pharmacodynamic interactions by 58%. The top two interactions they caught? NSAIDs with antihypertensives, and multiple CNS depressants (like benzodiazepines, opioids, and sleep meds) combined. In Australia, the National Health and Medical Research Council now recommends pharmacist-led medication reviews for anyone taking five or more drugs. That’s not optional anymore. It’s standard care.
What You Can Do
If you’re on more than three medications, especially if you’re over 65, you need to ask three questions:- Is there any chance these drugs are working against each other?
- Am I taking something that could make my blood pressure, breathing, or heart rhythm unstable?
- Have I been told what to watch for if something goes wrong?
The Future: Predicting Interactions Before They Happen
The field is changing. Researchers at UCSF built a machine learning model that predicts serotonin syndrome risk from polypharmacy with 89% accuracy. The European Clinical Research Infrastructure Network just launched a $4.7 million database focused solely on pharmacodynamic interactions. The FDA now requires these studies for all new CNS drugs. The goal? Move from reactive to proactive. Instead of waiting for someone to collapse, we’ll use AI and real-time data from electronic health records to warn doctors before they write the prescription. But that future won’t help you tomorrow. Right now, the best tool you have is awareness. Know that drugs don’t just act alone. They influence each other. And sometimes, that influence can kill.What’s the difference between pharmacodynamic and pharmacokinetic drug interactions?
Pharmacokinetic interactions change how your body absorbs, breaks down, or gets rid of a drug-like when grapefruit juice slows down liver enzymes that process statins. Pharmacodynamic interactions happen at the target site-like when one drug blocks a receptor another drug needs to work. One changes drug levels; the other changes how the drug works, even if the level stays the same.
Can over-the-counter drugs cause pharmacodynamic interactions?
Absolutely. NSAIDs like ibuprofen can reduce the effect of blood pressure meds. Antihistamines like diphenhydramine can add to sedation from opioids or benzodiazepines. Even St. John’s wort can trigger serotonin syndrome when mixed with antidepressants. OTC doesn’t mean safe-especially when you’re on other meds.
Why are pharmacodynamic interactions more dangerous in older adults?
Older adults often take 4-6 medications at once. Their kidneys and liver don’t clear drugs as well, so levels stay higher longer. But more importantly, their bodies are more sensitive to changes in drug effect. A small drop in blood pressure from an NSAID and ACE inhibitor combo can cause falls. A little extra sedation from sleep aids and painkillers can lead to respiratory failure. Their safety margin is thin.
Are there any beneficial pharmacodynamic interactions?
Yes. The antibiotic combo of trimethoprim and sulfamethoxazole is a classic example-they hit bacteria at two points in the same pathway, making them far more effective together. Low-dose naltrexone combined with certain antidepressants has shown promise in treatment-resistant depression by boosting endorphin activity. These aren’t accidents. They’re designed.
How can I check for drug interactions myself?
Use trusted databases like the University of Liverpool’s HIV Drug Interactions Checker (even if you don’t have HIV-it’s one of the most detailed), or Medscape’s Drug Interaction Checker. But don’t rely on apps that just say “possible interaction.” Look for ones that grade severity: avoid, use with caution, monitor. Always talk to your pharmacist. They’re trained to spot these.





January 22, 2026 AT 07:59
So let me get this straight-we’re telling people to just ‘ask their doctor’ while doctors are juggling 20 patients an hour? Yeah, no. That’s not care, that’s negligence wrapped in a white coat. I’ve seen people die because no one checked the damn interaction. Stop pretending this is just a ‘technicality.’