Transferring a prescription shouldn’t feel like a game of telephone. One wrong digit, one missing decimal, one misread refill count-and a patient could get the wrong dose, the wrong drug, or no drug at all. In 2025, with technology and regulations updated, prescription transfer is safer than ever-but only if you follow the rules exactly. A single error in labeling or transfer can lead to a life-threatening mistake. The FDA estimates that standardized labels alone could prevent 1.5 million adverse drug events each year. This isn’t theoretical. It’s happening in pharmacies right now.
What’s Allowed in Prescription Transfers Today?
The rules changed in August 2023. For the first time ever, the DEA allowed electronic transfers of Schedule II controlled substances-like oxycodone or fentanyl-between retail pharmacies. Before that, these prescriptions couldn’t be transferred at all. Now, you can send them electronically, but only once. After that, the original prescription is void. Schedule III to V drugs (like codeine or anabolic steroids) can be transferred multiple times, as long as refills remain. Non-controlled prescriptions have the most flexibility-most states allow unlimited transfers.The key? Everything must be done electronically. Faxing, calling, or manually re-entering data is no longer acceptable for Schedule II prescriptions. Even for other schedules, electronic transfers are the gold standard. A 2022 University of Florida study found that NCPDP SCRIPT-compliant electronic systems maintain 98.7% data accuracy. Fax transfers? Only 82.3%. Phone transfers? Just 76.1%. The margin for error shrinks dramatically when you go digital.
What Must Be on Every Prescription Label?
A prescription label isn’t just a sticker. It’s a legal document. The FDA requires every label to include:- Patient’s full name
- Drug name (generic or brand)
- Strength in metric units (e.g., 5 mg, not 5.0 mg)
- Dosage form (tablet, capsule, liquid)
- Quantity dispensed
- Directions for use (e.g., “Take one by mouth daily”)
- Prescriber’s name
- Prescription number
- Date issued
- Number of refills authorized
- Pharmacy name, address, and phone number
There are no exceptions. And there are dangerous traps to avoid. Trailing zeros are banned. Writing “1.0 mg” instead of “1 mg” has caused ten-fold dosing errors. The NCCMERP analyzed over 2,300 medication errors and found this mistake in dozens of cases. Leading zeros are required too. “.4 mg” is a red flag-it must be “0.4 mg.” The same goes for insulin, which is the only exception to metric-only rules. Using apothecary units (like grains or drams) is outdated and dangerous. ASHP’s 2021 data showed 12% of dosage errors came from mixing metric and old systems.
How Transfers Work Between Pharmacies
The process is strict-and automated. When a patient asks to transfer a prescription:- The patient must initiate the request. Pharmacies can’t transfer without the patient’s consent.
- The receiving pharmacy checks if they can fill the prescription-especially important for Schedule II drugs, which can only be filled once.
- The transferring pharmacy sends an electronic record using NCPDP SCRIPT 2017071 or newer.
- The system must preserve every field: original fill date, remaining refills, prescriber DEA number, transfer date, and both pharmacists’ IDs.
- The receiving pharmacy adds “transfer” to the record and logs the original pharmacy’s details.
- The original prescription is marked as transferred and invalidated.
For Schedule II drugs, the DEA requires the receiving pharmacy to record the original pharmacy’s name, address, and DEA number. Wisconsin’s rules go further: they require this info printed on the back of the invalidated paper copy. California’s data shows that 23% of transfer failures happen because patients don’t confirm the new pharmacy has the drug in stock. A patient might transfer a Schedule II prescription only to find out the pharmacy doesn’t carry it-and then wait days for a refill. That’s why automated systems that check inventory before finalizing the transfer are becoming standard. One pharmacy tech reported a 99% success rate using this method.
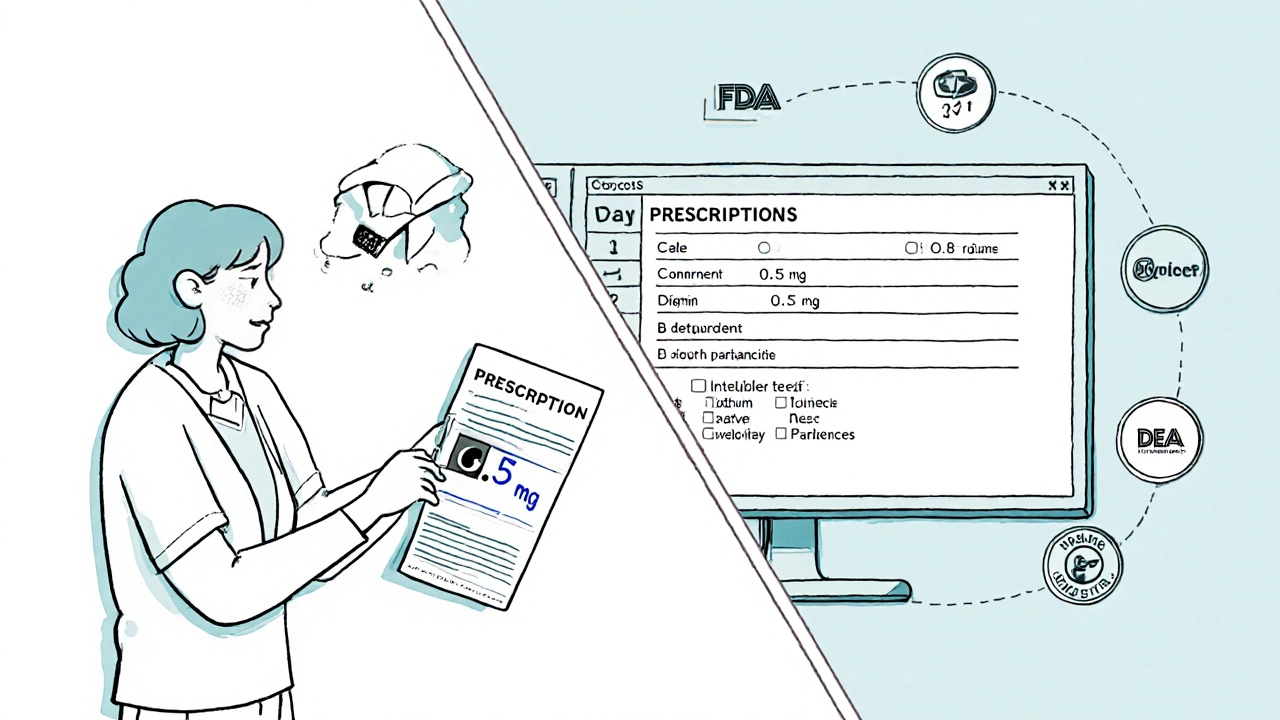
Why System Compatibility Matters
Not all pharmacy software talks to each other. Even with NCPDP standards, mismatches happen. The National Community Pharmacists Association found that 18% of pharmacies report data truncation during transfers-meaning part of the label gets cut off. That could mean missing directions, wrong strength, or no refill info. Independent pharmacies are hit hardest. Only 63% use certified electronic systems, compared to 87% of chain pharmacies. Rural areas are even worse: only 41% have reliable electronic transfer access, according to the National Rural Health Association. That’s why patients in these areas have a 15% higher rate of abandoning prescriptions after transfer attempts.When systems don’t sync, pharmacists have to manually verify every detail. That’s time-consuming. And humans make mistakes. That’s why barcode scanning and double-checking are critical. A 12-hospital study in JAMA Internal Medicine showed barcode verification cuts dispensing errors by 41%. Every pharmacist should verify: drug name, strength, quantity, directions, patient name, and refill count-twice. Dr. Michael Cohen of ISMP says standardized, patient-friendly labeling could prevent 30% of the 500,000 annual errors caused by misreading labels.
What Patients Need to Know
Patients aren’t just passive recipients. They’re part of the safety chain. Before asking for a transfer, they should:- Confirm the new pharmacy carries the medication-especially for controlled substances.
- Ask if the pharmacy can handle electronic transfers. Some small pharmacies still rely on fax.
- Never let someone else transfer their prescription without reviewing the label when picked up.
- Check for trailing zeros, missing decimals, or unclear directions.
- Ask for a printed copy of the label if the pharmacy only gives digital instructions.
Reddit threads like “Transfer horror stories” are full of patients who waited days because their new pharmacy didn’t have the drug. Others got the wrong dose because the label said “1.0 mg” instead of “1 mg.” A simple check could have prevented it.

What’s Coming in 2025 and Beyond
The FDA’s Patient Medication Information (PMI) rule goes fully live in 2025. It requires:- Standardized, easy-to-read labels in paper format by default
- Electronic labels only if the patient requests them
- Automated scanning systems that check label accuracy before the medication leaves the pharmacy
- Clear warnings for high-risk drugs
Early adopters report costs between $12,500 and $18,750 per pharmacy to upgrade systems. But the payoff is clear: fewer errors, fewer lawsuits, fewer deaths. Epic and Cerner have partnered with major pharmacy chains to link prescription transfers directly to electronic health records. ASHP predicts this will cut transfer errors by 75% by 2026.
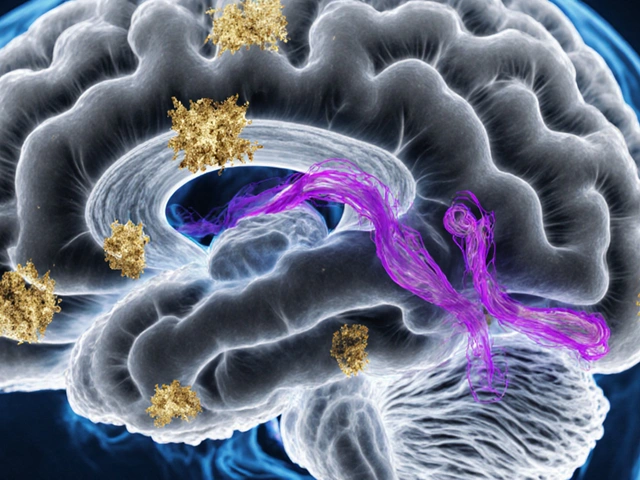
By 2030, the FDA expects 40% more prescriptions to contain multiple drugs. That means more chances for confusion. The only way to stay safe is to lock in accuracy at every step-from prescriber to label to transfer.
Common Mistakes and How to Avoid Them
Here are the top errors pharmacists make-and how to fix them:- Trailing zeros: Always write “5 mg,” never “5.0 mg.”
- Missing leading zeros: Write “0.5 mg,” not “.5 mg.”
- Using abbreviations: Never use “HCTZ” or “MOM.” Write out “hydrochlorothiazide” and “magnesium oxide mixture.”
- Forgetting refill status: Always check and display remaining refills.
- Skipping double-checks: Even with automation, verify the label manually before handing it to the patient.
- Assuming the patient knows: Don’t assume they understand “take once daily.” Write “Take one tablet by mouth every morning.”
Training matters. Pharmacists need about 8.5 hours of training to fully comply with the 2023 DEA rules. Staff turnover is a hidden risk-most pharmacies need to retrain every 6.2 months due to software updates. Don’t let knowledge gaps become patient risks.
Can I transfer a Schedule II prescription more than once?
No. Under the DEA’s 2023 rule, Schedule II controlled substance prescriptions (like oxycodone or fentanyl) can only be transferred electronically once. After that, the original prescription is voided and cannot be refilled or retransferred. The patient must get a new prescription from their prescriber if they need more medication.
What happens if the label says ‘1.0 mg’ instead of ‘1 mg’?
That’s a dangerous error. Trailing zeros after a whole number (like 1.0 mg, 5.0 mg) have caused ten-fold dosing mistakes-patients taking 10 times the intended dose. The FDA and NCCMERP have documented dozens of cases since 2018. Labels must show “1 mg,” not “1.0 mg.” Pharmacies are required to correct this before dispensing.
Can I transfer my prescription to any pharmacy?
You can request a transfer to any pharmacy that accepts electronic prescriptions. But not all pharmacies can handle controlled substances or have the right software. Always confirm the new pharmacy carries your medication and can process electronic transfers-especially for Schedule II drugs. If they can’t, you’ll face delays or have to go back to your original pharmacy.
Why do some pharmacies still use fax for transfers?
Fax is only allowed for Schedule III-V prescriptions and non-controlled drugs, and only if electronic transfer isn’t possible. Many small or rural pharmacies lack the technology or internet reliability to switch. But fax has a 17% higher error rate than electronic transfers. The DEA and FDA strongly discourage fax use because it increases the risk of misreading handwriting, missing refill info, or losing data.
How do I know if my prescription label is accurate?
Check five things: (1) Your name is spelled correctly, (2) the drug name matches what your doctor prescribed, (3) the strength has no trailing zeros (e.g., 5 mg, not 5.0 mg), (4) the directions are clear and complete, and (5) the number of refills left matches what your doctor authorized. If anything looks off, ask the pharmacist to verify it with the original prescription record before you leave.
Next Steps for Patients and Pharmacists
If you’re a patient: Always ask for a printed copy of your label. Don’t rely on digital apps or phone calls. Read it carefully. If it looks wrong, speak up. Don’t assume the pharmacy caught the mistake.If you’re a pharmacist: Use barcode scanning. Double-check every label. Train your team quarterly. Push for software upgrades that support the 2025 FDA PMI rule. If your system doesn’t auto-flag trailing zeros or missing leading zeros, demand an update.
Prescription safety isn’t about one perfect system. It’s about layers: accurate labeling, secure transfer, human verification, and patient awareness. Skip any layer, and someone could get hurt. The tools exist. The rules are clear. What’s left is doing the work-every time, without exception.






November 24, 2025 AT 02:46
Bro i just had a transfer go wrong and the label said '1.0 mg' for my blood pressure med. I took it and my heart felt like it was gonna explode. I called the pharmacy and they were like 'oh that's just a typo' like that's not a typo that's a death sentence. I swear if i died i'd haunt every pharmacist in the state.