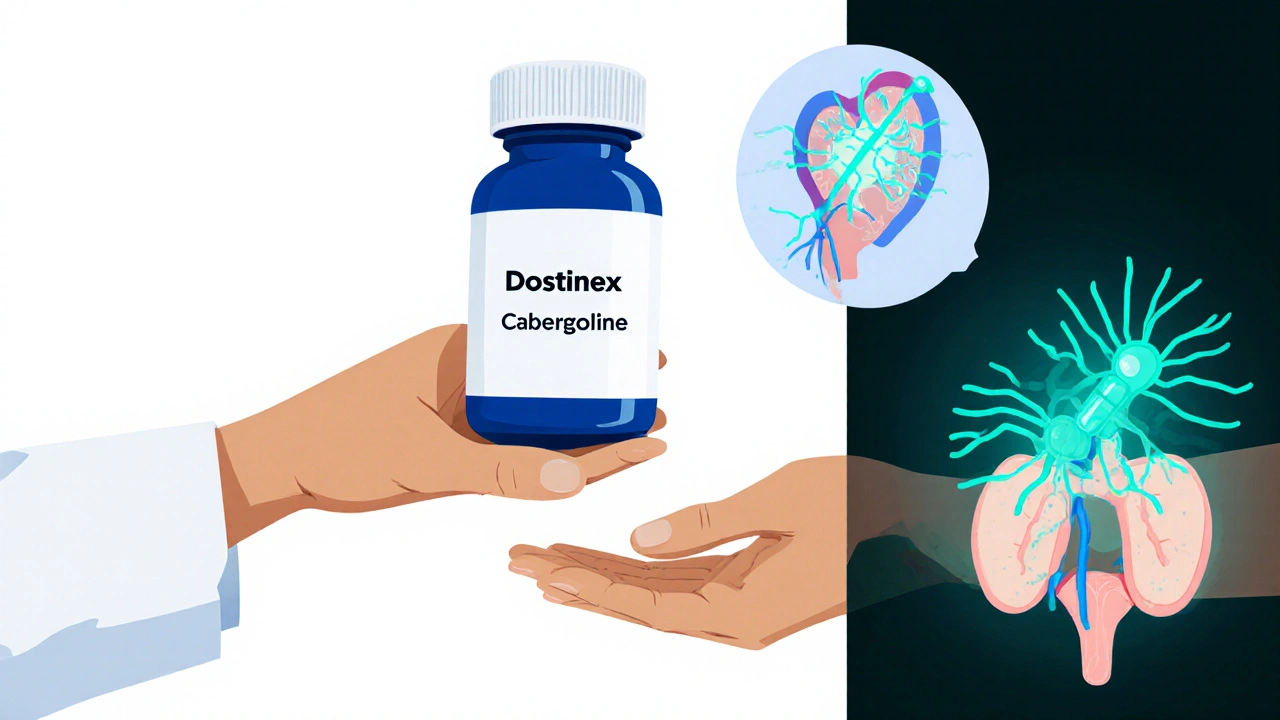
When your doctor prescribes a drug to lower elevated prolactin levels, you quickly discover there isn’t a one‑size‑fits‑all answer. Dostinex (Cabergoline) is a long‑acting dopamine agonist used primarily to treat hyperprolactinemia and prolactin‑secreting pituitary tumors. It was first approved in the 1990s and quickly became the go‑to option because of its convenient weekly dosing and strong efficacy.
What Is Dostinex (Cabergoline)?
Dostinex belongs to the class of medications called dopamine agonists. By binding to dopamine D2 receptors in the pituitary gland, it suppresses prolactin secretion. The result is a drop in serum prolactin, relief from symptoms such as menstrual irregularities, infertility, galactorrhoea, and, in many cases, shrinkage of the underlying Prolactinoma. Typical dosing starts at 0.25 mg twice a week, with titration up to 1 mg twice weekly for resistant cases.
How Does Cabergoline Work Compared to Other Dopamine Agonists?
All dopamine agonists share the same basic mechanism-stimulating dopamine receptors to inhibit prolactin release-but they differ in pharmacokinetics, potency, and side‑effect profile. Bromocriptine is an older, short‑acting agent that requires multiple daily doses. Quinagolide is a newer oral agent with a half‑life of about 15 hours, allowing once‑daily dosing. Cabergoline’s half‑life of 65 hours lets it be taken only twice a week, which many patients find far more convenient.
When Do Doctors Choose Alternatives?
Even though Dostinex is popular, certain situations push clinicians toward alternatives:
- Cost sensitivity: In some health systems, bromocriptine is significantly cheaper.
- Intolerance to nausea: Cabergoline can cause mild nausea, but some patients experience severe gastrointestinal upset that settles with bromocriptine.
- Cardiac concerns: High‑dose, long‑term Cabergoline has been linked-though rarely-to valvular heart disease. In patients with pre‑existing valve problems, doctors may opt for quinagolide or bromocriptine.
- Pregnancy planning: All three agents are considered relatively safe, but bromocriptine has the longest safety record in pregnancy.
Key Differences at a Glance
| Attribute | Dostinex (Cabergoline) | Bromocriptine | Quinagolide |
|---|---|---|---|
| Typical Dose Frequency | Twice weekly | 2-3 times daily | Once daily |
| Half‑life | ~65 hours | ~6 hours | ~15 hours |
| Prolactin‑lowering efficacy | 90‑95 % patients achieve normalization | 70‑80 % patients achieve normalization | 80‑85 % patients achieve normalization |
| Common side effects | Nausea, headache, dizziness | Nausea, hypotension, dizziness | Nausea, fatigue, dry mouth |
| Cost (US, generic, monthly) | $150‑$200 | $30‑$50 | $80‑$120 |
Choosing the Right Medication for You
Picking a therapy isn’t just about numbers; it’s about your lifestyle, health history, and personal tolerance. Below is a quick decision guide:
- Do you need minimal dosing? If you hate taking pills daily, Cabergoline’s twice‑weekly schedule is a clear win.
- Is cost the biggest driver? Bromocriptine’s generic price makes it attractive for cash‑pay patients or those with limited insurance coverage.
- Do you have heart valve concerns? Talk to your cardiologist. Quinagolide and bromocriptine have a lower theoretical risk of valvulopathy.
- Are you planning pregnancy? All three work, but bromocriptine’s long safety record often gives clinicians extra confidence.
Always involve your endocrinologist in the conversation. They’ll run baseline labs (serum prolactin, liver function, ECG if needed) and tailor the regimen.
Practical Tips for Managing Therapy
- Take with food: A light snack reduces nausea for all three agents.
- Monitor prolactin levels: Check at 4‑week intervals after starting or changing dose; then every 3‑6 months once stable.
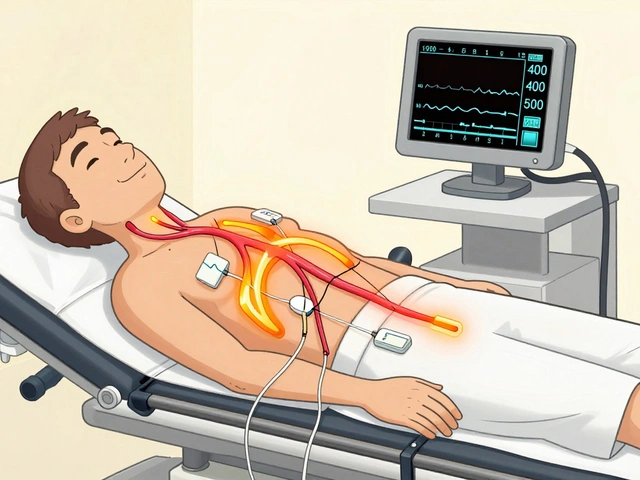
- Watch for cardiac symptoms: Shortness of breath, swelling of ankles, or new heart murmurs should prompt an echocardiogram, especially on long‑term Cabergoline.
- Adjust timing for sleep: Some patients feel drowsy after taking Cabergoline; schedule the dose earlier in the day if that’s an issue.
Frequently Asked Questions
Can I switch from bromocriptine to Dostinex?
Yes. Most endocrinologists cross‑taper by overlapping the drugs for a few days, then stop bromocriptine once Cabergoline reaches steady state (about two weeks).
What is the biggest safety concern with long‑term Cabergoline?
High‑dose, long‑duration therapy has been linked to valvular heart disease in Parkinson’s patients. In prolactinoma doses (<1 mg twice weekly), the risk is low, but annual echocardiograms are advised for treatment beyond five years.
Is quinagolide available everywhere?
It’s approved in Europe and parts of Asia but not in the United States. If you live in the U.S., bromocriptine or Cabergoline are your realistic options.
How quickly does prolactin drop after starting treatment?
Cabergoline typically reduces levels by 50‑60 % within the first two weeks. Full normalization often occurs by 8‑12 weeks. Bromocriptine may take longer, sometimes up to 6 months for the same effect.
Can these drugs be used for conditions other than prolactinoma?
Yes. They’re also prescribed for Parkinson’s disease, restless‑leg syndrome, and in some cases for preventing lactation after childbirth.
In a nutshell, Dostinex offers the most convenient schedule and highest efficacy, but alternatives like bromocriptine and quinagolide fill important niches around cost, cardiac safety, and regional availability. Discuss these points with your provider, track your labs, and you’ll find the regimen that best fits your life.



October 25, 2025 AT 14:28
If one were to rank the subtleties of dopamine agonism the way connoisseurs rank vintage Bordeaux, Dostinex undeniably occupies the loftiest shelf. Its bi‑weekly cadence whispers of a pharmacological aristocracy that the quotidian bromocriptine can only dream of. Yet the price tag reads like a ticket to an exclusive gala, leaving the mere mortals to count pennies. The occasional nausea is merely a reminder that even gods endure minor inconveniences. In the grand theater of endocrine manipulation, Cabergoline plays the lead, while the understudies scramble for applause.