Statin Tolerance Calculator
Your Personalized Plan
Action RequiredSelect your current statin and dose to see your personalized plan.
Important: Always discuss these recommendations with your doctor before making any changes to your medication.
Statin medications save lives. They cut LDL cholesterol by up to 60%, slash heart attack risk, and prevent strokes in millions of people worldwide. But for a significant number of users, the side effects - especially muscle pain - make staying on them feel impossible. If you’ve stopped your statin because of sore legs, fatigue, or general achiness, you’re not alone. And you don’t have to give up on the protection these drugs offer. The truth is, most people who think they can’t tolerate statins actually can - with the right dose adjustment or switch.
Why Muscle Pain Happens (and Why It Might Not Be the Statin)
The most common reason people quit statins is muscle pain. Doctors call it statin-associated muscle symptoms, or SAMS. It can feel like soreness, weakness, or cramping, often in the thighs or shoulders. About 1% to 10% of users report it, depending on the study. But here’s the twist: a major 2023 trial called SAMSON, which tracked over 6,000 people who thought they couldn’t handle statins, found that 90% of them had the same symptoms when taking a sugar pill as when taking the real drug. That’s not a typo. Most of the pain people blame on statins may actually be the nocebo effect - the opposite of placebo. If you’ve heard horror stories about statins, your brain might be primed to feel pain even when the drug isn’t causing it. That doesn’t make the pain any less real. But it does mean the solution isn’t always quitting the medication.First Step: Don’t Quit Right Away
If you’re having muscle symptoms, don’t just stop your statin and assume it’s the drug. The first thing your doctor should do is check for other causes. Hypothyroidism, vitamin D deficiency, and even normal age-related joint or muscle wear can mimic statin side effects. In fact, 15% to 20% of people reporting muscle pain from statins actually have an underactive thyroid. A simple blood test can rule this out. Also, check your medications. Some drugs - like certain antibiotics, antifungals, or even grapefruit juice - can interfere with how your body breaks down statins, making side effects more likely. If you’re on multiple meds, ask your doctor to review them. A drug interaction might be the real culprit.Dose Adjustment: Less Can Be More
Many people assume if a statin causes side effects, the only option is to stop it. But lowering the dose often works. For example, if you’re on 40mg of atorvastatin and feel achy, try dropping to 20mg. You’ll still get 30-40% LDL reduction - enough to make a big difference for most people. Even better: switch from daily dosing to every other day or twice weekly. This works especially well with longer-acting statins like rosuvastatin and atorvastatin. Rosuvastatin lasts nearly 20 hours in your body. Taking it every other day still keeps your cholesterol low. One patient in Melbourne, 68, switched from daily 10mg atorvastatin to 20mg every Monday, Wednesday, and Friday. His LDL stayed at 72 mg/dL. His muscle pain vanished. Studies show this approach works for up to 70% of people who thought they couldn’t tolerate statins. The American College of Cardiology recommends trying this before switching drugs. Start with a 2-week break to confirm symptoms go away, then restart at a lower or less frequent dose. Monitor creatine kinase (CK) levels if symptoms are severe - but for mild discomfort, this isn’t always needed.
Switching Statins: The 75% Success Rate
Not all statins are created equal. Some are more likely to cause muscle pain than others. Simvastatin, especially at doses above 20mg, has the highest risk. Lovastatin is similar. If you’re on one of these and having trouble, switching is often the answer. The key is choosing a statin that uses a different metabolic pathway. Simvastatin and atorvastatin are broken down by the CYP3A4 enzyme. Many drug interactions happen here. Rosuvastatin and pravastatin use different pathways - so switching to one of these avoids the problem. Real-world data from Geisinger Health System tracked over 12,000 patients who switched statins after side effects. About 75% of them tolerated the new one. Many moved from simvastatin to rosuvastatin. Others switched from atorvastatin to pravastatin. In both cases, muscle pain dropped sharply. Start low. If you’re switching to rosuvastatin, begin with 5mg twice a week. Wait four weeks. If you feel fine and your cholesterol is still in range, increase to every other day. Then daily if needed. This step-by-step approach gives your body time to adjust.Alternatives When Statins Still Don’t Work
If dose changes and switches still cause symptoms, you’re not out of options. You just need a different kind of tool. The first-line alternative is ezetimibe. It’s a pill that blocks cholesterol absorption in the gut. It lowers LDL by 15-25% - not as much as a statin, but enough to help, especially when combined with lifestyle changes. It’s cheap, well-tolerated, and has no muscle side effects. For higher-risk patients - those with diabetes, a history of heart attack, or very high LDL - PCSK9 inhibitors are an option. These are injectables given every two or four weeks. They drop LDL by 50-70%. But they cost about $5,800 a year, and insurance often requires prior authorization. They’re not for everyone, but for those who truly can’t take statins, they’re life-changing. Bile acid resins like cholestyramine can also help, but they cause bloating and gas in up to 40% of users. That’s why they’re rarely used as a first alternative.Supplements? CoQ10 and Vitamin D
You’ll hear a lot about Coenzyme Q10 (CoQ10). Statins lower CoQ10 levels in the body, and some believe that’s why muscles hurt. It sounds logical. But here’s the catch: no large, well-designed study has proven CoQ10 supplements reliably fix statin muscle pain. That said, many patients report feeling better taking 200mg daily. If you’re willing to try it, it’s safe. It won’t hurt. But don’t expect miracles. Vitamin D is different. Deficiency is common - affecting 40-60% of adults. Low vitamin D is linked to muscle weakness and pain. If your levels are low, correcting them can make a huge difference. Get tested. If you’re deficient, take 1,000-2,000 IU daily. Many people find their muscle symptoms improve within weeks.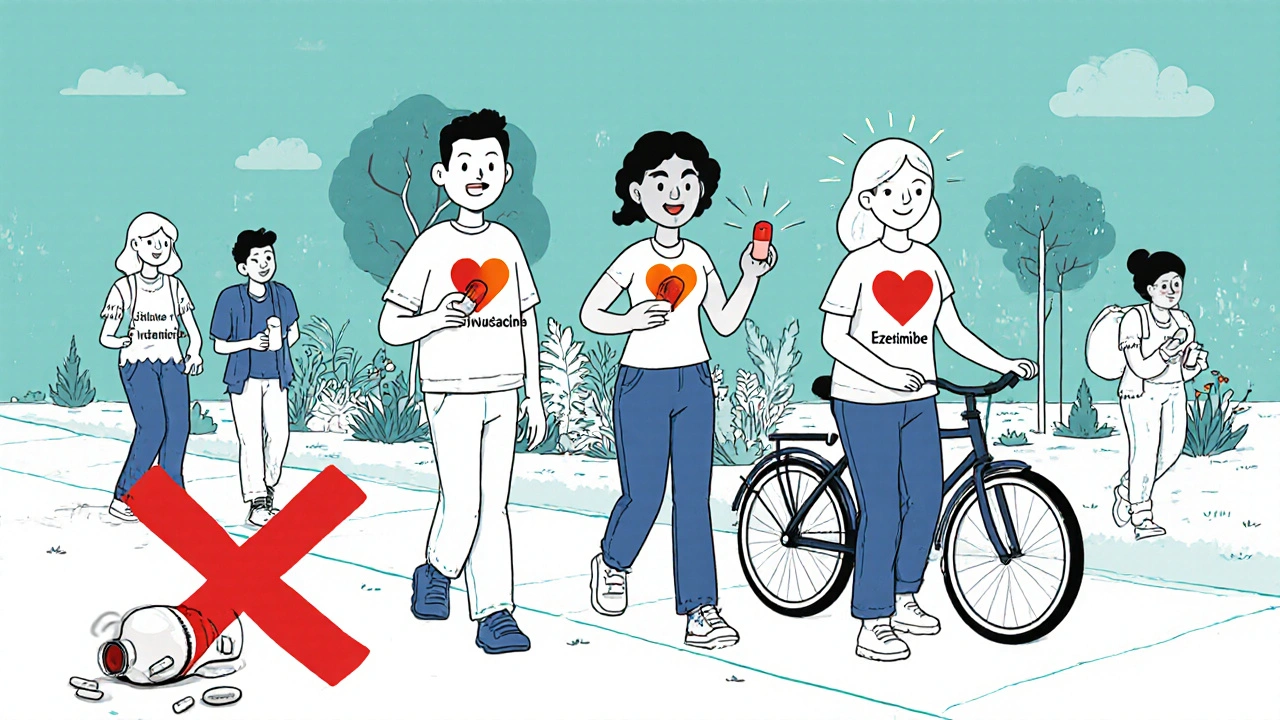
What Doesn’t Work - And What to Avoid
Don’t assume you’re one of the 1-2% who truly can’t tolerate statins. That number is small. Most people who quit statins do so because they didn’t get the right advice. Avoid going cold turkey without a plan. If you stop statins and your cholesterol spikes, your heart risk goes up fast. Don’t restart on the same dose that caused problems. Don’t switch to a higher dose hoping it’ll “get stronger.” That usually makes things worse. Also, skip the internet myths. Some claim apple cider vinegar or turmeric can replace statins. They can’t. Statins are the only drugs proven to reduce heart attacks and death in high-risk patients. No supplement comes close.Long-Term Success: It’s About Persistence
The goal isn’t to find the perfect statin. It’s to find a way to stay on treatment. The cardiovascular benefits are enormous. For every 25 people treated with a statin for five years, one major heart event is prevented. The risk of serious muscle damage (rhabdomyolysis)? Less than 1 in 10,000. People who stick with statins - even at lower doses or alternate schedules - live longer, healthier lives. A 2022 study from Kaiser Permanente showed that when clinics used structured dose-adjustment and switching protocols, statin discontinuation rates dropped from nearly 19% to under 10%. If you’ve struggled with side effects, you’re not broken. You just haven’t found the right fit yet. Talk to your doctor. Ask about trying a different statin. Ask about every-other-day dosing. Ask about checking your thyroid and vitamin D. Don’t give up. Your heart is worth it.Can I take statins every other day instead of daily?
Yes, for longer-acting statins like rosuvastatin and atorvastatin, every other day or even twice-weekly dosing can work. These statins stay active in your body for 19-20 hours, so skipping days still keeps cholesterol low. Studies show 70% of people who couldn’t tolerate daily dosing tolerate intermittent schedules well. Start with half the daily dose every other day and monitor your LDL after 4-6 weeks.
Which statin has the least side effects?
Rosuvastatin and pravastatin generally have the best tolerability profiles. Simvastatin, especially at doses above 20mg, carries the highest risk of muscle pain. Rosuvastatin isn’t broken down by the CYP3A4 liver enzyme, which reduces interactions with other drugs and lowers muscle side effect risk. Pravastatin is also low-risk and works well for older adults or those with kidney issues.
What should I do if my muscle pain returns after switching statins?
If pain returns after switching, go back to your doctor. You may need to try another statin with a different metabolic pathway. For example, if you switched from simvastatin to atorvastatin and still had pain, try rosuvastatin or pravastatin. Also, consider intermittent dosing - even if you switched statins, taking it less frequently can help. Rule out vitamin D deficiency and thyroid problems again.
Is it safe to stop statins for a few weeks to reset?
Yes, a short break of 2-4 weeks is often recommended to confirm that symptoms are truly linked to the statin. This is called a “drug holiday.” After stopping, if your muscle pain improves, it’s likely the statin was the cause. But don’t stop longer than 6 weeks if you’re at high risk for heart disease. Your LDL will rise quickly, and your heart risk increases. Always restart under medical supervision.
Do I need to take CoQ10 with my statin?
No, you don’t need to take CoQ10 - but it’s safe to try. Some people report less muscle pain when taking 200mg daily, though large studies haven’t proven it works. It won’t replace the need for dose adjustment or switching statins. If you’re already taking it and feel better, keep going. If not, focus on proven strategies first: checking vitamin D, thyroid levels, and trying a different statin or schedule.
Next Steps: What to Do Today
If you’re struggling with statin side effects, here’s your action plan:- Don’t quit without talking to your doctor.
- Ask for blood tests: thyroid (TSH), vitamin D, and creatine kinase (CK).
- Request a switch to rosuvastatin or pravastatin if you’re on simvastatin or atorvastatin.
- Try lowering the dose or switching to every other day dosing.
- If symptoms persist, ask about ezetimibe as a non-statin option.
- Track your symptoms and LDL levels over 4-6 weeks after any change.






November 23, 2025 AT 09:57
Wow. This is one of the most clinically nuanced pieces on statin tolerance I’ve read in years. The SAMSON trial reference alone elevates this from blog post to guideline material. I’ve seen so many patients quit statins after one bad experience, only to have their LDL skyrocket and end up in the ER six months later. The nocebo effect is massively under-discussed in primary care - we need more of this kind of education.