Drug Interaction Mechanism Identifier
Identify Drug Interaction Type
Enter two drugs to see if their interaction is pharmacokinetic (PK) or pharmacodynamic (PD), with explanation and clinical guidance.
Two drugs taken together can save your life-or send you to the hospital. It all comes down to whether the interaction is pharmacokinetic or pharmacodynamic. Most people think of drug interactions as simple conflicts: "Don’t take this with that." But the real science behind why they happen is far more precise-and far more important.
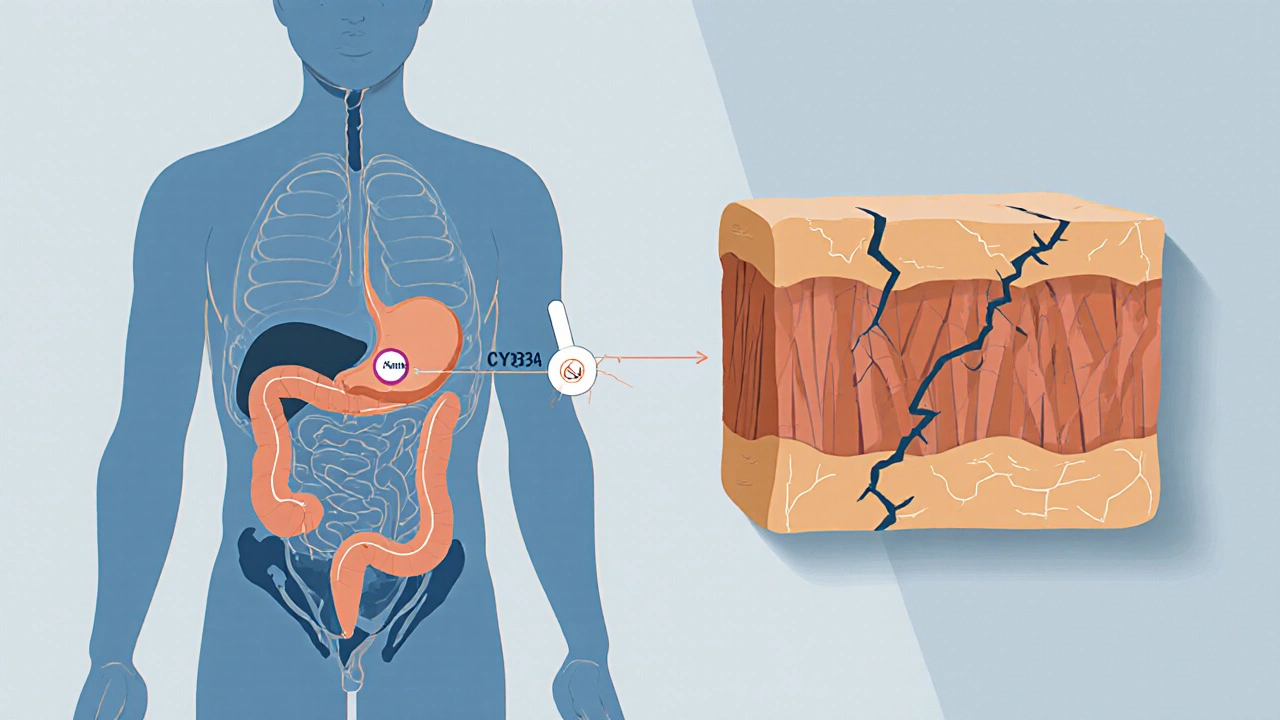
What Pharmacokinetic Interactions Do to Your Body
Pharmacokinetic interactions are about what your body does to the drug. Think of it like a delivery system. If one drug changes how fast another gets absorbed, distributed, broken down, or flushed out, you’ve got a pharmacokinetic (PK) interaction. These are the most common type of clinically significant drug interactions, making up nearly half of all serious cases.Take CYP3A4, a liver enzyme that handles about 75% of all drug metabolism. If you’re on simvastatin for cholesterol and start taking clarithromycin for a sinus infection, that antibiotic blocks CYP3A4. Suddenly, your simvastatin levels spike-up to 10 times higher than normal. That’s not just a minor bump. It can cause muscle damage, kidney failure, even death. The FDA recommends cutting simvastatin to 10 mg or avoiding it entirely with clarithromycin.
It’s not just metabolism. Antacids like Tums can bind to antibiotics like ciprofloxacin in your gut, cutting absorption by 75-90%. That means the antibiotic doesn’t reach the infection. Warfarin, a blood thinner, can be pushed off protein-binding sites by drugs like phenylbutazone, making 300% more of it float around freely in your blood. That’s a recipe for uncontrolled bleeding.
Even excretion matters. Probenecid, used for gout, blocks the kidney’s ability to clear penicillin. That’s not a bug-it’s a feature. Doctors used to give probenecid with penicillin to make the antibiotic last longer. Today, we see it as a risk when patients take both without knowing why.
These interactions don’t happen overnight. CYP3A4 inhibitors like clarithromycin or grapefruit juice take 3-5 days to reach full effect. But once they do, the change is powerful. That’s why therapeutic drug monitoring (TDM) is critical for drugs with narrow therapeutic windows-like warfarin, digoxin, or phenytoin. A simple blood test can tell you if the drug level is safe or dangerous.
What Pharmacodynamic Interactions Do to Your Body
Now flip the script. Pharmacodynamic (PD) interactions are about what the drug does to your body-not how much of it is there, but how it acts. Two drugs can be at perfect concentrations, but if they both hit the same target, things go wrong.There are three main types:
- Synergistic: The combined effect is greater than the sum. Take sildenafil (Viagra) and nitroglycerin. Together, they drop blood pressure so hard it can cause cardiac arrest. That’s why the warning is black-and-white: never mix them.
- Additive: Effects pile up. Warfarin and aspirin both thin blood. Together, bleeding risk jumps. Same with alcohol and benzodiazepines-both depress the brain. Add them, and you risk stopping breathing.
- Antagonistic: One drug cancels the other. Naloxone (Narcan) blocks opioid receptors to reverse overdoses. Beta-blockers and beta-agonists fight over the same heart receptors. One lowers heart rate, the other raises it. If you take both, they neutralize each other.
These interactions are sneaky. You might not see a change in drug levels, but your body reacts anyway. A 2023 review found that 85% of CNS drug interactions-like mixing antidepressants and opioids-are pharmacodynamic. Serotonin syndrome from combining SSRIs and MAO inhibitors? That’s PD. It’s not about too much serotonin in the blood. It’s about too much serotonin signaling in the brain.
Even seemingly unrelated drugs can clash. NSAIDs like ibuprofen reduce the effectiveness of ACE inhibitors by 25-30%. Why? Because NSAIDs block prostaglandins that help blood vessels relax. The blood pressure pill still works-but not as well. Patients think their medication failed. It didn’t. Another drug canceled its effect.
Why the Difference Matters in Real Life
Knowing whether an interaction is PK or PD changes everything about how you manage it.For PK interactions, you can often adjust the dose. Lower the statin. Space out the antibiotic and antacid. Monitor blood levels. It’s fixable.
For PD interactions? Sometimes, you just can’t. You can’t give someone a lower dose of nitroglycerin to make it safer with Viagra. You can’t reduce the serotonin effect of an SSRI without losing its benefit. The only safe move is to avoid the combination entirely.
That’s why the UK’s Specialist Pharmacy Service says: "Understanding the mechanism is crucial." A pharmacist who sees a patient on warfarin and amiodarone doesn’t just check a database. They ask: Is this a metabolism issue (PK)? Amiodarone inhibits CYP2C9, which breaks down warfarin. Or is it a bleeding risk (PD)? Both drugs thin blood. Answer: both. That’s why they need weekly INR checks and a clear warning.
Older adults are at highest risk. One in six people over 65 takes five or more medications. That’s a minefield. A 72-year-old on digoxin (for heart rhythm), lisinopril (for blood pressure), and trimethoprim (for a UTI) might not know that trimethoprim can raise digoxin levels by 30% (PK) and also cause potassium loss, which makes digoxin more toxic (PD). Two different mechanisms. One dangerous outcome.
How Modern Tools Help (and Still Fall Short)
Electronic health records now flag thousands of potential interactions. Epic’s system alone lists over 1,200 high-risk PK interactions and nearly 1,000 PD ones. But alerts are noisy. Clinicians see 20 warnings per day. Many ignore them.That’s why pharmacist-led medication reviews cut adverse events by 42%. Pharmacists don’t just read alerts. They ask: "Is this a real risk? What’s the mechanism? Is there a safer alternative?" They know that a PK interaction with a narrow-therapeutic-index drug needs a lab test. A PD interaction with CNS depressants needs a breathing check.
Machine learning is getting better. A 2023 AI model predicted PD interactions with 89% accuracy-better than traditional methods. But it still can’t replace a clinician who understands physiology. An AI might flag that a patient is on an SGLT2 inhibitor and a loop diuretic. It knows the risk of dehydration. But only a human can ask: "Are they drinking enough? Are they dizzy? Are they losing weight?" That’s where the real judgment happens.
The FDA and EMA now require drug makers to test interactions with 11 CYP enzymes and 8 transporters-not just the big ones. Pharmacogenomics is adding another layer. If you’re a poor metabolizer of CYP2D6, even a small dose of codeine can turn into dangerous morphine levels. That’s PK. But if you’re also on an SSRI that blocks CYP2D6? Now you’ve got a double hit. That’s why CPIC now has 32 gene-drug pair guidelines.
What You Should Do
If you’re on multiple medications, here’s what actually works:- Keep a list. Write down every pill, supplement, and herbal product. Include doses and why you take them.
- Ask your pharmacist: "Is there any interaction I should worry about?" Pharmacists are trained to spot PK and PD risks. They’re not just dispensers-they’re safety experts.
- Know your high-risk drugs. Warfarin, digoxin, lithium, phenytoin, and certain antibiotics are common troublemakers.
- Watch for symptoms. Dizziness, confusion, bleeding, muscle pain, or sudden drops in blood pressure? Don’t assume it’s aging. It could be a drug interaction.
- Don’t assume natural means safe. St. John’s wort induces CYP3A4 and can make birth control, antidepressants, and heart meds fail. Grapefruit juice? It’s a CYP3A4 inhibitor. One glass can mess with your meds for days.
The goal isn’t to avoid all combinations. It’s to avoid the dangerous ones. Many drug pairs are safe. Some even help. But you need to know why.
What’s Changing Now
The field is moving fast. The WHO estimates better PK/PD understanding could prevent 1.3 million adverse events worldwide by 2030. That’s billions in saved healthcare costs.New biologics-like immune checkpoint inhibitors for cancer-are creating new PD risks. Combine them with immunosuppressants, and you can trigger autoimmune reactions that weren’t predicted in trials.
Real-world data from the FDA’s Sentinel Initiative has already found 17 new PD interactions in just two years. One of them? SGLT2 inhibitors (like dapagliflozin) with loop diuretics. Together, they increase dehydration risk by more than double. No one saw that coming in clinical trials. But now we know.
The message is clear: drug interactions aren’t just a list of "don’t mix." They’re a science. And the science is evolving.
What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic (PK) interactions change how your body handles a drug-like how fast it’s absorbed, broken down, or cleared. Pharmacodynamic (PD) interactions change how the drug affects your body, even if the drug level stays the same. PK is about concentration; PD is about effect.
Can you fix a pharmacokinetic interaction by changing the dose?
Yes, often. If a drug raises the level of another by blocking its metabolism, lowering the dose of the affected drug can keep it in a safe range. For example, reducing simvastatin from 80 mg to 10 mg when taking clarithromycin avoids muscle damage. But this only works for drugs with a wide safety margin. For narrow-therapeutic-index drugs like warfarin, monitoring (like INR tests) is just as important as dose changes.
Why are pharmacodynamic interactions harder to predict?
Because they depend on how drugs interact at the receptor or system level-not just how much is in the blood. Two drugs can be at perfect levels, but if they both lower blood pressure or both depress breathing, the combined effect can be dangerous. These effects aren’t always linear, and sometimes they involve multiple pathways. That’s why combinations like NSAIDs and ACE inhibitors reduce blood pressure control by 25-30%-it’s not obvious from the drug labels alone.
Are herbal supplements safe to take with prescription drugs?
No, not without checking. St. John’s wort induces liver enzymes and can make birth control, antidepressants, and heart medications less effective. Garlic and ginkgo can increase bleeding risk with warfarin or aspirin. Even green tea can interfere with some chemotherapy drugs. Just because it’s "natural" doesn’t mean it’s safe with your meds.
Can pharmacokinetic interactions be tested with blood work?
Yes, for certain drugs. Therapeutic drug monitoring (TDM) measures blood levels of drugs like warfarin, digoxin, lithium, and phenytoin. If a new drug is added and the level spikes or drops, it’s likely a PK interaction. TDM doesn’t work for all drugs, but for those it does, it’s a powerful tool to prevent harm.
How do I know if a drug interaction is serious?
Look for three signs: 1) The drug has a narrow therapeutic index (like warfarin or digoxin), 2) It’s used for a life-threatening condition, or 3) The combination affects the brain, heart, or kidneys. If you feel dizzy, confused, weak, have unusual bleeding, or your blood pressure drops suddenly-call your doctor. Don’t wait.
Drug interactions aren’t something to ignore. They’re not just warnings on a label. They’re real, measurable, and often preventable. Whether it’s a liver enzyme blocking a drug’s breakdown or two drugs teaming up to lower your blood pressure too far-knowing the difference between pharmacokinetic and pharmacodynamic helps you ask the right questions. And in medicine, the right question can save your life.





November 20, 2025 AT 13:03
Just read this and my brain exploded. PK vs PD isn’t just jargon-it’s the difference between your meds working or turning you into a human pincushion. I’ve seen people on 5+ drugs and no one ever explains this. Why is this not taught in high school? 🤯