Statins—yeah, those so-called cholesterol busters—are everywhere, but what gets more prescriptions than almost anything else on the planet? Lipitor. Odds are, you’ve heard of it at the doctor’s office, seen it splashed across a TV ad, or maybe someone in your family takes it. But why do doctors reach for Lipitor so often? What’s really going on under the hood with this little white pill? Let’s take a look, and maybe bust a few myths along the way.
What Exactly Is Lipitor and Why Do Doctors Love It?
Lipitor, if you want the science-speak, is called atorvastatin. It showed up in pharmacies back in 1996 and quickly took over the statin market. Its main job? Lowering LDL (the so-called "bad cholesterol") while giving HDL (the "good cholesterol") a tiny sympathetic nudge upward. The less LDL in your arteries, the smaller your risk for heart attacks and strokes. At its peak, Lipitor was making about $13 billion a year worldwide. That’s not just big; that’s blockbuster big.
Doctors often recommend Lipitor because it’s well-researched, generally well-tolerated, and extremely effective. Studies show Lipitor can drop LDL cholesterol by as much as 60% for some folks who stick with it. That’s a massive shift, especially if your family tree looks like a medical horror movie when it comes to heart problems.
But the story isn’t quite as simple as "high cholesterol = take Lipitor = never worry about heart attacks again." The American College of Cardiology recommends statins for people who already have heart disease, are diabetic and over 40, or have a 10-year risk for heart disease above 7.5% (yep, your doc probably ran those numbers on you). Yet, not everyone with even a slightly high cholesterol number gets a green light for statin therapy—other risk factors, lifestyle, and age all matter too.
Another thing that gives Lipitor an edge is its flexible dosing. Whether your bad cholesterol is sky-high or just slightly off, docs can tweak the dose pretty easily—anywhere from 10 mg to 80 mg a day—while monitoring your blood work. It also plays nicely with other medications, although there are some exceptions we’ll get into soon.
How Does Lipitor Tackle Cholesterol in Your Body?
Lipitor isn’t magic—it works by getting in the way of something called HMG-CoA reductase. That's the enzyme your liver uses to make cholesterol. By blocking this process, Lipitor tells your liver, “Maybe make a little less cholesterol, okay?” And when your liver gets stingy, it starts pulling more cholesterol out of your blood.
The effects are fast. Most people see their cholesterol numbers drop within two weeks, with the full impact showing up after about four to six weeks. Just a heads up: you won't notice or "feel" these changes happening. No energy boost, no sudden drop in your craving for cheeseburgers—just better lab results the next time your doctor has you pee into a cup or stick out your arm for a blood test.
Your liver’s not the only thing affected by Lipitor, though. Some people notice changes in their blood sugar. Rare side effects can touch your muscles and, in very uncommon cases, even your memory. On the plus side, research from a 2022 meta-analysis in the Journal of the American Heart Association shows that statins, including Lipitor, can lower the chances of heart attacks and strokes by about 25% compared to placebo. That’s no small potatoes.
Still, every body is different. Lipitor gets processed through your liver and leaves the body mostly through your poop. If you’ve got chronic liver problems, or a history of certain muscle diseases, your doctor might pause before writing that prescription.
Common Side Effects and What to Watch Out For
Most people take Lipitor without too much drama, but, let’s be real, every drug has its downside. The most common hiccups are mild and often fade as your body adjusts. We’re talking headache, a bit of belly discomfort, maybe some muscle aches. Some people say they feel tired or a little foggy at first.
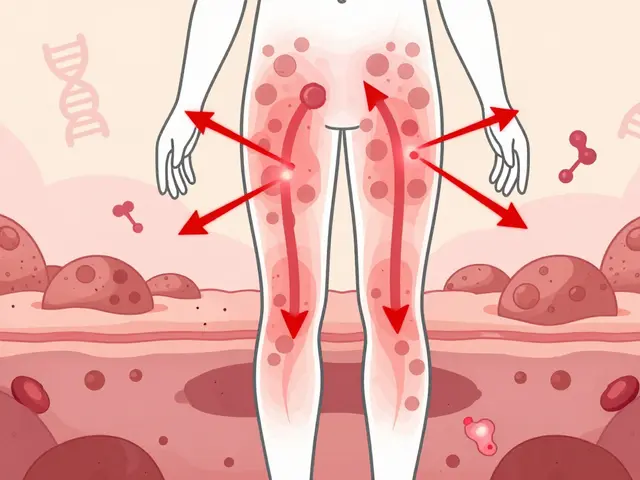
Muscle aches are the side effect that gets the most buzz. In most cases, it’s not a big deal—a bit of soreness, especially after working out. Rarely, Lipitor can cause more serious issues like myopathy or rhabdomyolysis—complicated words for “your muscles are in trouble.” If you get unexplained muscle pain, weakness, especially with dark urine, call your doctor ASAP. In my years writing about medicine, I've heard from people who shrugged off muscle cramps, thinking it was just part of aging or a tough week at the gym. Sometimes, it really is the statin. Wise move: speak up if something feels off.
Liver enzymes can go up a bit—doctors usually check your blood work a few weeks after you start, just in case. Every now and then, Lipitor messes with blood sugar, nudging it up enough to push some folks toward diabetes, especially if they’re already close. Hair loss, memory problems, and digestive issues have popped up in some cases, but these are pretty uncommon and often get better after stopping or changing the dose.
Here's a quick look at the numbers from clinical studies about side effects:
| Side Effect | Reported Frequency (approx.) |
|---|---|
| Muscle pain/weakness | 3-7% |
| Digestive upset (nausea, diarrhea) | 2-5% |
| Headache | 1-4% |
| Elevated liver enzymes | 0.5-2% |
Most side effects show up in the first few weeks and mellow out or disappear. But for a handful of people, the drug just isn't a good fit. Your doc can always switch you to a different statin or try a lower dose if you hit a speed bump.
Who Should Avoid Lipitor and What to Discuss With Your Doctor
Lipitor isn’t for everyone. If you’re pregnant, planning to get pregnant, or breastfeeding, this drug is strictly off-limits. Cholesterol is actually important for developing babies, and Lipitor can mess with that. Also, if you have liver disease—especially if your liver numbers are off the charts—Lipitor might do more harm than good.
Allergies to statins are rare but real. If you broke out in a rash, had hives, or couldn’t breathe last time you took a statin, make sure your doctor knows before you pick up your next prescription. Ditto for folks who’ve ever had muscle problems related to statin use.
Certain meds don’t play nice with Lipitor. Gemfibrozil, cyclosporine, a few HIV treatments, and some antibiotics (think clarithromycin) can bump up Lipitor levels in your blood, raising your risk for side effects. If you’re on more than five prescription meds, have a quick medication review with your pharmacist or doctor. That little step can save you a world of hassle. And one you might not expect: even grapefruit juice, in big amounts, can mess with how Lipitor breaks down, so docs often recommend limiting it to less than a quart a day (and who drinks more than that, anyway?).
- Talk to your doctor about any muscle soreness, especially if it comes on suddenly.
- Mention any plans for pregnancy or if you’re breastfeeding.
- Bring up all other meds and supplements you’re taking, even if they seem unrelated.
- Share any history of liver or kidney issues, even if they’re old news.
- Let your doctor know about your family history of muscle or liver problems.
Your doctor might order blood tests before and after you start Lipitor, just to keep an eye on your liver, kidney function, and blood sugar. Don’t skip those labs—they’re not just busywork. They catch problems before they get serious.
How to Get the Most From Lipitor: Tips for Everyday Life
If you’re prescribed Lipitor, here’s how to keep things running smoothly and avoid surprises:
- Take it consistently—same time every day, with or without food. Creating a routine (like brushing your teeth) makes it way less likely you’ll miss a dose.
- If you do forget, don’t double up. Just take the next one at your usual time. Doubling increases your risk of side effects, and it won’t help your cholesterol any faster.
- Check your pharmacy’s generic options. Atorvastatin (the generic for Lipitor) can save you hundreds of dollars a year, and it’s the same active ingredient.
- Keep a record of your cholesterol numbers each time you get labs done. Seeing your progress makes it easier to stick to the plan—and it’s a great tool for those quick doctor visits.
- Don’t ditch healthy habits. Even with lipitor, diet and exercise matter—a lot. The combo works better than the pill alone for lowering cholesterol and protecting your heart.
- Grapefruit juice and alcohol in moderation—unless your doc says otherwise. Both can affect how your body handles Lipitor.
- Watch for muscle pain, weakness, or brownish pee. These can be serious; make that call if things feel off.
- Ask about drug interactions if you start anything new, including herbal supplements like St. John’s Wort.
Real talk: Even after years on Lipitor, you could see cholesterol numbers creep up. Bodies change, and so do cholesterol levels—especially if pounds sneak up, meals get a little heavier, or you’re dealing with more stress. Regular follow-ups matter. Don’t skip out on your doctor’s reminders for blood work and check-ins.
Lipitor by the Numbers: The Global Impact and Future Trends
If you want to know just how big of a force Lipitor has been in heart health, check this out: at its peak, one out of every five adults over 40 in the U.S. was on a statin, and Lipitor dominated the market. Since the generic version, atorvastatin, became available in 2011, costs have plummeted. Today, you can grab a month’s supply for the price of a couple of coffees. That shift has opened the door for millions more people to access one of the most proven heart protection tools ever invented.
Still, there’s plenty of debate: Should healthy people with only slightly high cholesterol get statins? Do we start too many people on these meds? Should we be paying more attention to lifestyle changes first? The best data says statins, and Lipitor especially, save lives if you’re in a moderate or high-risk category. But medicine’s never one-size-fits-all—what works for someone else might not work for you.
Big pharma is always working on the next big thing, but Lipitor’s twenty-five-year run at the top isn’t ending soon. If you’re curious, there’s even research into whether statins could help with conditions most people wouldn’t expect, like Alzheimer’s and certain cancers. Some of that is early, still-in-the-lab stuff, but it shows how versatile these medications might turn out to be.
If you ever feel lost sorting cholesterol numbers or staring at all those pill bottles, know you’re not alone. Lipitor’s story isn’t just about a pill—it’s about millions of people living longer and dodging the world’s #1 killer: heart disease. Whether you’re on Lipitor, thinking about it, or just looking out for someone you love, it’s worth learning how this little tablet made such a massive difference—and how, with a smart plan, you can take control of your own heart health journey.






May 22, 2025 AT 19:09
Listen up, folks-statins like Lipitor have been a game‑changer for heart health, and that’s not just hype. In my part of India we call it the “cholesterol shield” because it actually saves lives. The drug’s safety profile is pretty solid, but you still need regular blood work to keep an eye on liver enzymes. If you’re on other meds, double‑check for interactions-especially with grapefruit, that’s a classic slip‑up. Bottom line, take it as prescribed and don’t skip those doctor visits. It definatly feels like a must‑have prescription for anyone with a family history of heart disease.