When you have rheumatoid arthritis, knowing how active your disease is isn’t just about how you feel on a given day. It’s about tracking real, measurable changes in your joints, inflammation levels, and long-term damage. Doctors don’t guess anymore. They use tools - CDAI, DAS28, and imaging - to see exactly where you stand and whether your treatment is working. These aren’t just numbers on a page. They’re the backbone of modern RA care, helping to stop joint damage before it’s visible and avoid unnecessary drug changes.
What CDAI Tells You (And What It Doesn’t)
The Clinical Disease Activity Index, or CDAI, is simple. It adds up four things: the number of tender joints, the number of swollen joints, how you rate your overall disease activity (on a scale of 0 to 10), and how your doctor rates it. No blood tests. No fancy machines. Just a quick exam and a few questions. That’s why it’s the go-to tool in most U.S. rheumatology clinics.
A CDAI score under 2.8 means you’re in remission. Between 2.8 and 10? Low disease activity. 10 to 22 is moderate. Over 22? High activity. That’s it. No calculations needed. Many clinics have it built right into their electronic health records - it takes less than two minutes to complete.
But here’s the catch: CDAI doesn’t measure inflammation directly. If your body is quietly burning with inflammation but your joints aren’t visibly swollen or tender, CDAI might say you’re doing fine. That’s why some patients feel worse than their score suggests. Fatigue, morning stiffness, or general malaise don’t show up in CDAI - even though they’re real and disabling. One study found that fatigue alone accounts for 14% of what patients consider a meaningful change in their condition - something CDAI completely misses.
DAS28: The Lab-Dependent Alternative
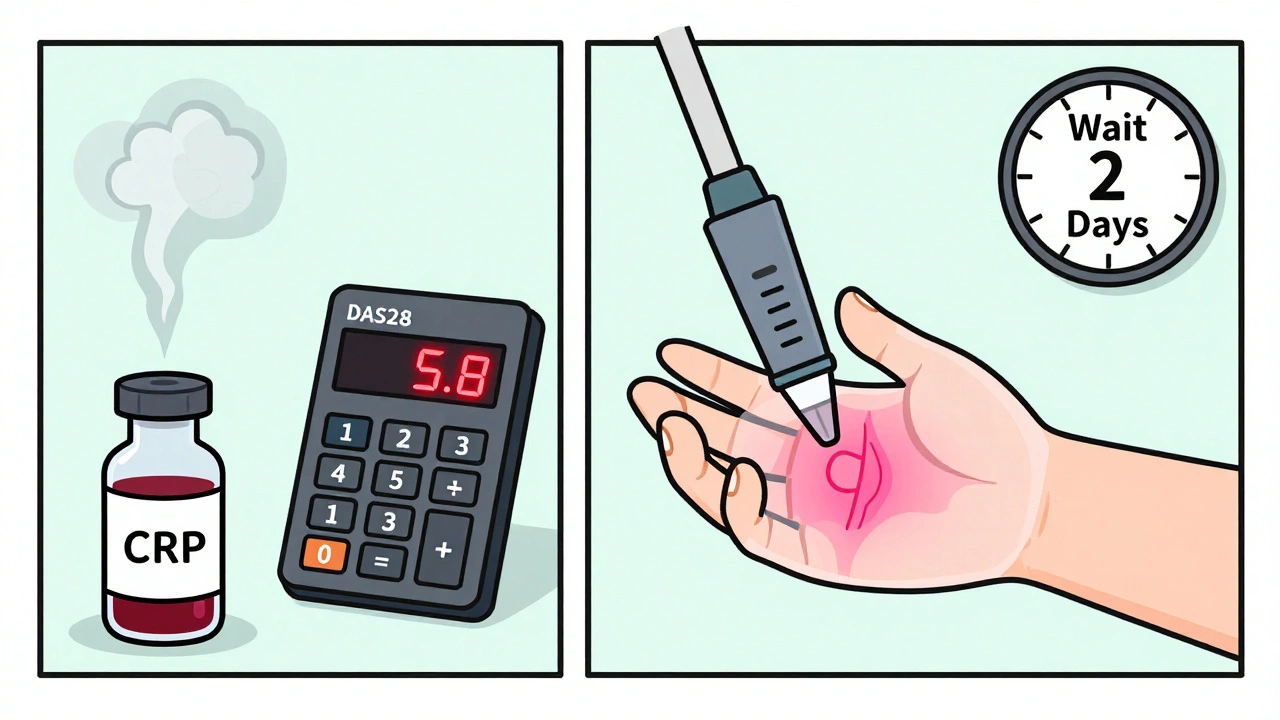
DAS28 is more complex. It uses the same joint counts as CDAI, but adds a blood marker - either ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein). These measure inflammation in your bloodstream. The formula looks intimidating, but the idea is simple: if your blood shows inflammation, your score goes up, even if your joints feel okay.
DAS28-CRP (using CRP) is now more common than DAS28-ESR because CRP results come back faster and are more stable. A score under 2.6 means remission. Between 2.6 and 3.2? Low activity. 3.2 to 5.1? Moderate. Above 5.1? High.
The problem? You need lab results. In real-world clinics, blood work often doesn’t come back until after your appointment. Doctors end up making decisions on a hunch, then adjusting later when the CRP comes in. One survey found that 57% of rheumatologists say they often make provisional treatment calls while waiting for results. That’s not ideal. It delays care, creates confusion, and can lead to over- or under-treatment.
Still, DAS28 is better at catching hidden inflammation. For patients with early RA or those on biologics, it’s often more sensitive than CDAI alone. In Europe, DAS28 is still the standard. In the U.S., CDAI has taken over - not because it’s better, but because it’s faster and easier to use daily.
Imaging: Seeing What the Eye Can’t
There’s a big gap between what your joints feel like and what’s happening inside them. That’s where imaging comes in.
Conventional X-rays have been the gold standard for decades. They show bone erosion and joint space narrowing - the permanent damage RA causes. The Sharp/van der Heijde score tracks this over time. A change of 5 points or more in a year means your disease is progressing. But X-rays are slow. It takes 6 to 12 months of active inflammation before damage shows up. By then, it’s too late to reverse it.
Ultrasound changed the game. It can see synovitis - swollen joint lining - months before X-rays show anything. Power Doppler ultrasound picks up blood flow in inflamed tissue, which means it can spot active inflammation even when joints don’t look swollen. Studies show ultrasound finds synovitis in 85% of cases where a physical exam misses it. And it’s fast, cheap (around $150 in the U.S.), and can be done right in the clinic. Some rheumatologists now use it during every visit. One study found that ultrasound changed treatment plans in 22% of cases where doctors would’ve kept the same therapy based on exam alone.
MRI is the most powerful tool. It shows bone edema - swelling inside the bone itself - which is often the first sign of future erosion. MRI can predict which joints will be damaged next with 89% accuracy. But it’s expensive ($1,200 per scan), takes time, and isn’t available everywhere. Most clinics only use MRI for complex cases or research. Still, for patients with high disease activity and no clear response to treatment, an MRI can reveal hidden damage that explains why they’re still struggling.
How These Tools Work Together
No single tool tells the whole story. That’s why the best care combines them.
In routine visits, most U.S. clinics use CDAI. It’s fast, reliable, and tied to outcomes. If your CDAI score is high - say, above 10 - your doctor might order an ultrasound to check for hidden synovitis. If the ultrasound shows active inflammation but your joints don’t feel swollen, that’s a red flag. You might need a stronger medication, even if your CDAI isn’t in the “high” range.
If your CDAI is low but you’re still tired and in pain, ultrasound or MRI might show ongoing inflammation. That’s when you and your doctor have a real conversation: Is your treatment working? Or are you just tolerating symptoms?
Imaging isn’t for everyone. If you’ve been in remission for two years with no symptoms and normal CDAI scores, you probably don’t need an MRI every year. But if your score jumps suddenly, or your pain doesn’t match your exam, imaging becomes critical.
One big issue: discordance. In about one-third of patients, how they feel (patient global assessment) doesn’t match what the doctor sees (physician global assessment). Patients often report higher pain levels. That doesn’t mean they’re exaggerating - it means RA affects more than joints. Fatigue, brain fog, and emotional stress all feed into how you feel. CDAI and DAS28 don’t capture that. That’s why some experts argue we need better patient-reported tools.

What’s New and What’s Coming
Technology is catching up. New software like QUASAR can automatically analyze ultrasound images and score inflammation without human input - reducing bias and saving time. The ACR just launched an EHR module called “RA Monitor” that automatically triggers an imaging referral if your CDAI score hits 10 or higher. That’s a game-changer for busy clinics.
AI is starting to read MRI and ultrasound scans with 92% accuracy, matching expert radiologists. In the future, you might wear a small sensor that tracks your joint movement and activity levels day and night. Combine that with daily symptom logs on your phone, and your doctor gets a full picture - not just a snapshot from one visit.
Right now, the goal is treat-to-target: get your disease activity as low as possible, ideally into remission. Studies show that using these tools to guide treatment cuts joint damage by 30% to 50% compared to old-school care. That’s not a small win. It’s the difference between staying active and needing joint replacements in your 40s or 50s.
What Patients Should Know
You’re not just a number. But those numbers matter. Ask your doctor: What score are we using? Why? What are we looking for? If you’re on a biologic and your CDAI is low but you’re still exhausted, say so. Push for an ultrasound if your pain doesn’t match your exam. Don’t assume imaging is only for “bad cases.”
Also, be honest. If you’re not taking your meds regularly, or you’re skipping appointments because you feel “okay,” your score won’t reflect the truth. These tools only work if your input is accurate.
And don’t fear imaging. Ultrasound is painless, quick, and shows real-time results. You can see the inflammation in your wrist while the tech is scanning. That’s powerful. It turns abstract disease into something visual - something you can understand and fight.
RA monitoring isn’t about perfection. It’s about progress. And with CDAI, DAS28, and imaging, you and your doctor have more tools than ever to keep you moving - without letting the disease win.







December 2, 2025 AT 20:29
CDAI is a joke if you're on biologics. I've had 0 swollen joints for 18 months but my CRP is through the roof and I can't get out of bed. Doctors treat the score not the patient. CDAI is for lazy clinicians who don't want to order labs.
Stop pretending simplicity equals accuracy. This isn't a kindergarten report card.