Medication Safety Checker
How this tool works
Based on the article's research, healthcare teams use pharmacists to identify potential interactions between medications. This tool simulates how collaborative care prevents side effects by checking your medication list for common interactions.
When you’re taking five or more medications, side effects aren’t just annoying-they can be dangerous. One wrong combination, a missed dose, or a drug that doesn’t mix with your liver condition can land you back in the hospital. But here’s the truth: pharmacists, doctors, and specialists working as a team cut these risks by more than half. It’s not magic. It’s structured collaboration-and it’s happening right now in clinics, hospitals, and community pharmacies across the country.
Why Siloed Care Fails on Side Effects
Picture this: A 72-year-old patient sees their cardiologist for high blood pressure, their endocrinologist for diabetes, and their primary care doctor for arthritis. Each prescribes a new medication. No one talks to the others. Two weeks later, they’re in the ER with dizziness and low potassium. Why? Because the blood pressure drug and the diabetes drug together caused a dangerous electrolyte shift. The pharmacist never saw the full list. The doctors didn’t know what the others prescribed. This isn’t rare. Studies show that 43% of patients on five or more medications have at least one harmful drug interaction. In traditional care, these errors happen because no single provider has the full picture. Doctors focus on treating the disease. Specialists focus on their organ system. Pharmacists? They’re often left out of the room until discharge. That’s changing. Teams that bring pharmacists into the conversation from day one reduce medication-related hospitalizations by 23.1%. That’s not a guess-it’s a 2021 systematic review published in the Journal of Interprofessional Care. And the reason is simple: pharmacists know what’s in the bottle, how it interacts, and whether the patient can actually afford or take it.The Pharmacist’s Role: More Than Just Filling Prescriptions
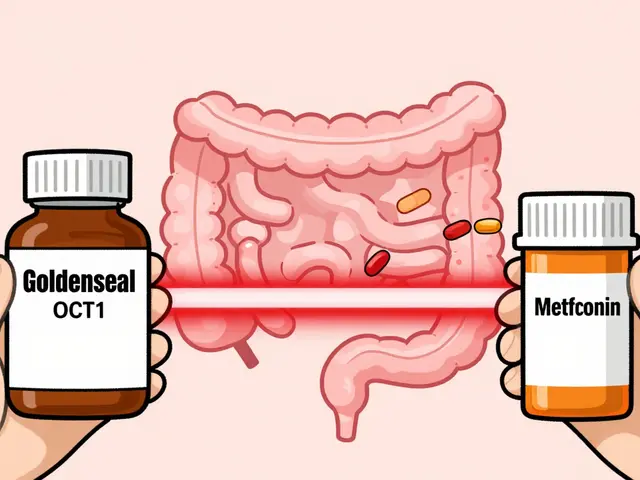
Pharmacists aren’t just checking for typos anymore. In collaborative models, they’re clinical decision-makers. They review every medication a patient takes-not just what’s on the current prescription, but supplements, over-the-counter drugs, and even herbal remedies. They spot interactions others miss. For example, a statin and a grapefruit juice habit? That’s a liver risk. A diuretic and a kidney patient? That’s an electrolyte trap. In a landmark 2019 New England Journal of Medicine study, pharmacist-led teams achieved 94% blood pressure control in African-American men with resistant hypertension. The standard care group? Only 29%. How? Pharmacists adjusted doses, removed redundant drugs, and followed up weekly. They didn’t wait for the patient to come back. They called. They asked: “Are you taking this?” “Can you afford it?” “Are you dizzy when you stand?” They also handle medication reconciliation-comparing what a patient was taking before hospitalization to what they’re prescribed after. This single task reduces medication errors by 67%, according to a 2022 JAMA Internal Medicine study. That’s 67% fewer cases of someone going home with a drug they’re allergic to, or doubling up on the same medicine because two doctors prescribed it.Doctors and Specialists: Letting Go of Control
Some doctors still think, “I’m the expert. I decide.” But the data doesn’t lie. In a 2023 survey by the American Society of Health-System Pharmacists, 87% of U.S. hospitals now have formal agreements where pharmacists can adjust anticoagulants, diabetes meds, and antibiotics without waiting for a doctor’s approval. That’s not a loophole-it’s a protocol. Specialists benefit too. A cardiologist can focus on heart function while the pharmacist manages the five drugs that affect it. A rheumatologist doesn’t have to memorize every NSAID interaction. The pharmacist does. This isn’t delegation. It’s specialization. But there’s resistance. In a 2021 ASHP survey, 37% of pharmacists reported physicians were hesitant to share decision-making. Why? Fear of losing control. Lack of trust. But when teams work together for 6-8 months, that changes. One primary care clinic in Minnesota saw physician buy-in jump from 40% to 89% after just one year of daily 15-minute huddles. Pharmacists walked in with medication lists, flagged risks, and suggested alternatives. Doctors started asking: “What do you think we should do?”
How It Works: The Daily Rhythm of a Collaborative Team
It doesn’t require a fancy system. Just structure.- Daily huddles: Pharmacists join morning rounds. They flag 2-3 high-risk patients per physician. No meetings. No emails. Just 10 minutes standing in the hallway.
- Shared EHR: All providers use the same electronic health record with HL7 FHIR standards. When a pharmacist changes a dose, the doctor sees it instantly. No delays. No confusion.
- Collaborative practice agreements: These are legal documents that spell out exactly what the pharmacist can do. Adjust warfarin? Yes. Prescribe a new diabetes drug? Only if the doctor signs off. Define it in writing. No guesswork.
- Follow-up calls: After a new med is started, the pharmacist calls the patient in 3 days. “How’s your stomach?” “Any new rashes?” “Can you afford this?” That’s how they catch problems before they become emergencies.
Real Results: Numbers That Matter
- **94% blood pressure control** in high-risk patients with pharmacist-led teams vs. 29% in standard care (NEJM, 2019) - **67% fewer medication errors** after pharmacist-led reconciliation (JAMA Internal Medicine, 2022) - **23.1% lower hospital readmissions** in teams with integrated pharmacists (Journal of Interprofessional Care, 2021) - **1.2% greater HbA1c reduction** in diabetic patients under collaborative care (Diabetes Care, 2022) - **89% patient satisfaction** in collaborative care models (Journal of the American Pharmacists Association, 2023) And here’s the kicker: it saves money. Avalere Health estimates these teams save $28.7 billion a year in the U.S. by preventing hospitalizations and ER visits. That’s not theoretical. That’s real dollars.
Where It’s Working-and Where It’s Not
This model thrives in places with clear rules and funding. In accountable care organizations (ACOs), 76% now have embedded pharmacists. Medicare Advantage plans reward them for improving medication adherence. In integrated health systems like Kaiser Permanente or the VA, pharmacists are full members of the care team. But outside those systems? It’s patchy. Only 28 states reimburse Medicaid for pharmacist services. Many private insurers still treat pharmacists as dispensers, not clinicians. And in rural areas? There’s often no pharmacist on-site at all. The biggest barrier isn’t skill. It’s structure. Without a collaborative practice agreement, a pharmacist can’t adjust a dose-even if they see a clear risk. Without shared EHR access, they’re working in the dark. Without reimbursement, clinics can’t afford to hire them.What’s Next: The Future Is Already Here
In 2025, CMS plans to start directly reimbursing pharmacists for comprehensive medication management. That’s a game-changer. It means pharmacists won’t have to wait for a doctor to bill for their work. They can bill themselves. By 2026, 92% of academic medical centers plan to expand pharmacist roles. Telehealth is part of it too. During the pandemic, pharmacist-led virtual check-ins reduced therapy delays by 63%. Now, that’s standard. The Institute for Healthcare Improvement predicts that by 2030, 75% of U.S. primary care will use this model. Why? Because it works. Patients get fewer side effects. Fewer trips to the ER. Fewer pills they don’t need. And they live longer.What You Can Do
If you’re a patient: Ask if your care team includes a pharmacist. If you’re on five or more meds, request a medication review. Say: “Can we schedule a time for the pharmacist to look at everything I’m taking?” If you’re a provider: Start small. Have a 10-minute huddle with your local pharmacist. Share one high-risk patient. See what they notice. You’ll be surprised. If you’re a system leader: Fund the EHR integration. Create collaborative agreements. Pay pharmacists for clinical time. This isn’t a cost. It’s a return on investment. Side effects don’t happen because of bad doctors. They happen because of broken systems. Fix the system-and you fix the side effects.Can pharmacists really change my medication without my doctor’s approval?
Yes-but only if there’s a formal collaborative practice agreement in place. These are legal documents that outline exactly what a pharmacist can do, like adjusting doses of blood thinners, diabetes drugs, or antibiotics. In 48 states, pharmacists can enter into these agreements with physicians. In hospitals and integrated health systems, this is routine. But in independent clinics, it’s still rare unless the practice has adopted team-based care.
Why don’t all doctors work with pharmacists?
Some physicians worry about losing control or don’t know how to use pharmacists effectively. Others haven’t seen the evidence. A 2021 survey found 37% of doctors were initially resistant. But once teams work together for 6-8 months, trust builds. Doctors who use pharmacists report fewer medication errors, less burnout, and better patient outcomes. The shift isn’t about replacing doctors-it’s about adding expertise.
Do I need to go to a special clinic to get this kind of care?
No. Many community pharmacies now offer Medication Therapy Management (MTM) at no extra cost if you’re on Medicare Part D. You can walk in and ask for a free review of all your medications. Hospitals and primary care clinics with ACOs or value-based care contracts also embed pharmacists. Ask your doctor: “Is there a pharmacist on our care team?” If not, request one.
How do I know if a drug interaction is serious?
Serious interactions often cause dizziness, confusion, irregular heartbeat, unexplained bruising, or sudden changes in energy or mood. If you’re on five or more medications, even a common OTC painkiller like ibuprofen can raise your blood pressure or harm your kidneys. Don’t guess. Ask your pharmacist to review your full list every 6 months. They’re trained to spot hidden risks.
Is this model only for older adults with many meds?
No. While it’s most common in older adults, anyone on multiple medications benefits. Younger patients with autoimmune diseases, mental health conditions, or chronic pain often take 4-6 drugs. Pharmacists help reduce side effects like weight gain, fatigue, or GI issues. The goal isn’t age-it’s complexity. If your treatment plan feels overwhelming, a pharmacist can simplify it.






February 14, 2026 AT 15:20
I love how this post paints pharmacists as superheroes, but let’s be real-most of them are just scanning barcodes and answering the same three questions all day. I’ve been to like five pharmacies in the last year, and not once did anyone ask if I was dizzy or could afford my meds. They just handed me the bottle and said, 'Have a nice day.'