ADHD Stimulant Heart Risk Assessment Tool
Personalized Risk Assessment
This tool helps evaluate your cardiac risk when taking stimulant medications for ADHD based on clinical guidelines. It is not a substitute for professional medical advice.
When you start a stimulant medication for ADHD, you’re not just looking for better focus-you’re hoping to regain control of your life. But what if that same pill could quietly mess with your heart? It’s not a scare tactic. It’s a real, documented risk that doctors are still learning how to manage. For millions of people taking amphetamines like Adderall or methylphenidate like Ritalin, the benefits are clear: improved attention, less impulsivity, better performance at school or work. But behind those gains is a quiet conversation between your nervous system and your heart-one that can sometimes go wrong.
How Stimulants Can Trigger Heart Rhythm Problems
Stimulants work by flooding your brain with dopamine and norepinephrine. That’s what helps you concentrate. But those same chemicals also hit your heart. They make it beat faster, push blood harder through your arteries, and change the electrical signals that keep your heartbeat steady. In most people, this is harmless. But in some, it’s enough to trigger an arrhythmia-a heartbeat that’s too fast, too slow, or irregular.
Research shows the biggest risk comes in the first 30 days after starting the medication. A 2021 study of adults over 65 found their chance of a dangerous ventricular arrhythmia tripled during that window. Even more concerning, illicit stimulants like cocaine and methamphetamine do far more damage. They don’t just speed up your heart-they block key ion channels that control electrical flow in heart muscle. Cocaine, for example, can prolong the QT interval on an ECG, a red flag for sudden cardiac arrest. Methamphetamine does the same, while also causing long-term scarring in heart tissue. These aren’t theoretical risks. Real people, often young, end up in emergency rooms because of them.
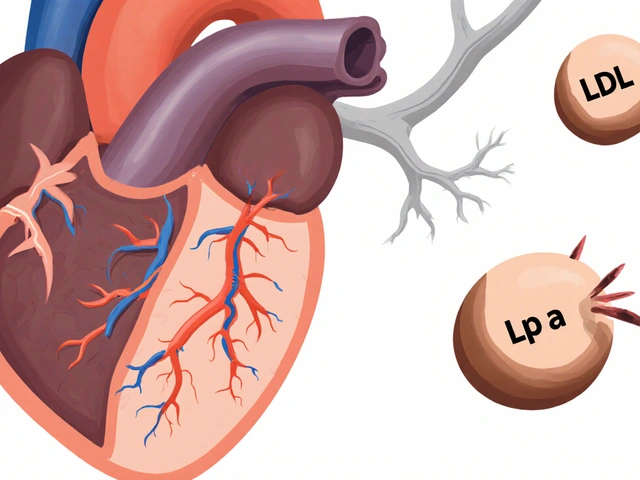
The Big Contradiction: Do Prescription Stimulants Really Increase Heart Risk?
Here’s where things get confusing. Some studies say yes-prescription stimulants raise heart risk. Others say no. A 2022 meta-analysis in JAMA Network Open looked at over a million patients and found no statistically significant link between ADHD meds and cardiovascular disease. So which one do you believe?
The truth lies in the details. The risk isn’t the same for everyone. For a healthy 12-year-old with no family history of heart disease, the chance of a serious event is extremely low-about 1 in 100,000 per year, according to a 2011 study of over 1.2 million children. But for a 70-year-old with high blood pressure and a history of fainting? The numbers shift dramatically. The same drug that helps a teenager focus might be dangerous for someone older. And the longer you take it, the more your heart may change. A 2024 study from the American College of Cardiology found that young adults on stimulants for eight years had a 57% higher risk of developing cardiomyopathy-a condition that weakens the heart muscle and can lead to arrhythmias.
There’s also a difference between amphetamines and methylphenidate. Amphetamines release more norepinephrine and dopamine all at once, which may make them slightly harder on the heart. Methylphenidate works more slowly and steadily. While direct comparisons on arrhythmia rates are limited, clinical experience suggests methylphenidate may be the safer pick for people with even mild heart concerns.
Who Needs to Worry? The Real Risk Factors
You don’t need an ECG before every prescription. But you do need to ask the right questions.
- Have you or any close relative had sudden cardiac death before age 50?
- Do you have a known heart condition-like long QT syndrome, hypertrophic cardiomyopathy, or a history of heart murmurs?
- Have you ever passed out for no reason, especially during exercise?
- Do you have uncontrolled high blood pressure?
- Are you using any other medications that affect heart rhythm, like antidepressants or antibiotics?
If you answered yes to any of these, your doctor should take extra steps. That might mean an ECG, a referral to a cardiologist, or avoiding stimulants altogether. Even if you’re young and healthy, if you’ve had unexplained palpitations or chest tightness, it’s worth getting checked. These aren’t rare events-they’re preventable if caught early.
What Doctors Actually Do in Practice
In real clinics, not every patient gets an ECG. Most doctors follow the guidelines from the American Heart Association and the American Academy of Pediatrics: a detailed medical history and a physical exam. They listen for heart murmurs, check your pulse, and measure your blood pressure. That’s it-for most people.
But monitoring doesn’t stop there. After starting a stimulant, your doctor will likely ask you to come back in one to three months to check your blood pressure and heart rate again. If your systolic pressure jumps above the 95th percentile for your age and height, they’ll adjust your dose or switch you to something else. That happens in about 1-2% of patients. It’s not common, but it’s common enough to matter.
For kids with congenital heart disease-especially if it’s repaired but not fully stable-doctors are more cautious. Some will still prescribe stimulants, but only after a cardiologist signs off. For adults with a history of arrhythmias, stimulants are often avoided unless absolutely necessary.
What to Do If You’re Worried About Your Heart
If you’re already on a stimulant and you’re feeling off-heart racing, dizzy, chest tight, or faint-you need to act. Don’t wait. Call your doctor. Get your blood pressure checked. Ask for an ECG. It’s a simple, painless test that can rule out serious problems.
Don’t stop your medication cold turkey. That can cause a crash-fatigue, depression, worse ADHD symptoms. Talk to your doctor first. They can help you taper safely or switch to an alternative.
Non-Stimulant Alternatives That Actually Work
There are three main non-stimulant options approved for ADHD, and they’re not just backup plans-they’re legitimate treatments.
- Atomoxetine (Strattera): A norepinephrine reuptake inhibitor. It doesn’t speed up your heart like stimulants do. It takes 4-8 weeks to kick in, but once it does, it works all day. About 50-60% of people respond well. Side effects? Nausea, fatigue, and in rare cases, liver issues or mood changes.
- Guanfacine (Intuniv): Originally a blood pressure drug. It calms the brain’s overactive signals without stimulating the heart. Works well for impulsivity and emotional regulation. Takes 2-4 weeks to show results. Common side effects: drowsiness, low blood pressure, dry mouth.
- Clonidine (Kapvay): Similar to guanfacine. Helps with hyperactivity and sleep problems. Often used in combination with other meds. Side effects include drowsiness and dizziness, especially when standing up.
These aren’t as fast or as powerful as stimulants. But for someone with a family history of sudden cardiac death, a history of arrhythmias, or high blood pressure, they’re the safer path. And for many, they’re enough.
The Bottom Line: Balance, Not Fear
Stimulants aren’t dangerous for most people. But they’re not risk-free. The key isn’t avoiding them entirely-it’s knowing who’s at risk and how to monitor it. For the vast majority of patients, the benefits of better focus, better grades, better jobs, better relationships far outweigh the tiny chance of a heart problem.
But if you have even one red flag in your history-if you’ve ever fainted, if someone in your family died suddenly before 50, if your blood pressure is climbing-you need to be proactive. Ask for an ECG. Ask about alternatives. Don’t let fear stop you from getting help-but don’t ignore warning signs either.
The field is changing. New guidelines from the American College of Cardiology are coming in late 2025. They’ll likely push for more personalized risk assessment-maybe even genetic testing down the road to see who’s more sensitive to stimulant effects. Until then, the best tool you have is your own body. Listen to it. Talk to your doctor. And don’t assume that because you’re young, you’re invincible.
Do all stimulants carry the same heart risk?
No. Amphetamines like Adderall and Vyvanse tend to have a slightly stronger effect on heart rate and blood pressure than methylphenidate-based drugs like Ritalin and Concerta. This is because they cause a more rapid release of norepinephrine. While direct comparisons on arrhythmia rates are limited, clinical experience suggests methylphenidate may be a safer choice for people with existing heart concerns.
Should I get an ECG before starting ADHD medication?
Routine ECGs aren’t required for everyone. Major guidelines from the American Heart Association and American Academy of Pediatrics say a thorough medical history and physical exam are enough for most patients. But if you have symptoms like fainting, chest pain, palpitations, or a family history of sudden cardiac death before age 50, an ECG is strongly recommended.
Can stimulants cause sudden cardiac death?
The risk is extremely low in healthy individuals-studies estimate it at about 1 in 100,000 per year. But in people with undiagnosed heart conditions like long QT syndrome or hypertrophic cardiomyopathy, the risk increases. Illicit stimulants like cocaine carry a much higher risk. The key is identifying hidden heart problems before starting medication, not avoiding treatment altogether.
How long does it take for heart risks to appear?
The highest risk for arrhythmias is in the first 30 days after starting a stimulant, especially in adults over 65. For structural heart changes like cardiomyopathy, the risk builds over years-studies show a 57% higher risk after eight years of use in young adults. That’s why ongoing monitoring matters, not just a one-time check.
Are non-stimulant ADHD meds as effective?
They’re less effective on average. Stimulants help about 70-80% of patients. Non-stimulants like Strattera, Intuniv, and Kapvay work for about 50-60%. But for people who can’t take stimulants due to heart risks, they’re often the best option. Many patients find they work well enough to improve daily functioning, even if they don’t feel as sharp as they did on stimulants.
What should I do if I feel my heart racing on ADHD meds?
Don’t panic, but don’t ignore it. Take your pulse. If it’s over 100 beats per minute at rest and you feel lightheaded, dizzy, or chest-tight, call your doctor. Get your blood pressure checked. Ask for an ECG. Your doctor may lower your dose, switch you to a different medication, or recommend a cardiology consult. Never stop suddenly-work with your provider to taper safely.
What Comes Next?
The future of ADHD treatment is personal. We’re moving away from one-size-fits-all prescriptions. In the next few years, genetic tests may help identify who’s more likely to have heart rhythm changes from stimulants. Wearable ECG monitors could alert doctors to early signs of trouble before symptoms appear. And new non-stimulant drugs are in development that target ADHD without touching the heart at all.
For now, the message is simple: Be informed. Be honest with your doctor. Ask questions. And if you have a family history of heart trouble, don’t assume you’re fine just because you’re young. The best treatment is the one that helps you live better-without putting your heart at risk.




November 22, 2025 AT 00:53
Stimulants are a tool, not a threat. The real issue isn't the medication-it's the lack of personalized monitoring. I've seen patients on Adderall for a decade with zero cardiac issues because their doctors tracked BP and heart rate every 3 months. The 57% cardiomyopathy risk? That's over eight years of unmonitored use. With proper care, the benefits massively outweigh the risks.