Swimmer’s ear isn’t just a nuisance after a long day at the pool-it’s a real infection that can turn simple actions like chewing or touching your ear into sharp, unbearable pain. Medically called otitis externa, this condition hits hard and fast, often within two days of water exposure. It’s not caused by dirty water alone; it’s about moisture trapped in the ear canal, creating the perfect breeding ground for bacteria. Up to 98% of cases are bacterial, mostly from Pseudomonas aeruginosa or Staphylococcus aureus, and it’s not rare-nearly 2.4 million Americans visit a doctor for it every year, mostly during summer months.
What Does Swimmer’s Ear Actually Feel Like?
If you’ve ever had swimmer’s ear, you know it’s not like a regular earache. The pain isn’t dull or distant-it’s intense, localized, and gets worse when you tug on your earlobe or press the small bump in front of your ear (the tragus). That’s the tragus test, and doctors use it because it’s 94% accurate at telling swimmer’s ear apart from middle ear infections. Most people report pain so severe they can’t sleep on that side. You might also notice drainage-first clear fluid, then thick yellow or green pus. Hearing can drop by 20 to 30 decibels, making voices sound muffled, like you’re underwater. Your ear canal will look swollen, sometimes so much that it’s nearly closed off.
Children between 7 and 12 years old are most at risk, followed by teens and young adults. Men are diagnosed more often than women, likely because they swim more frequently and are less likely to seek help early. If you have eczema or psoriasis on your scalp or ears, you’re also at higher risk. The real kicker? It’s not the swimming itself-it’s what you do after.
Why Do People Keep Getting It?
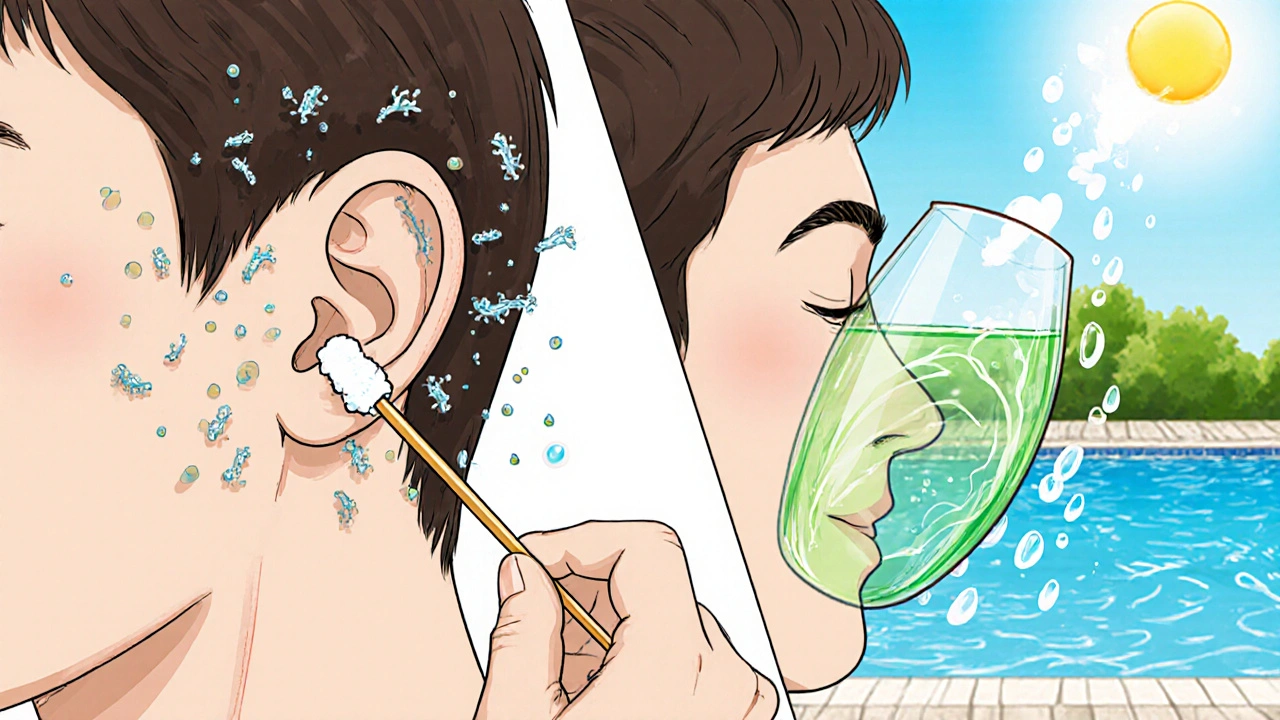
Most people think swimmer’s ear comes from swimming in polluted water. But the real culprit? Moisture and trauma. If you swim more than four days a week, your risk jumps 7.2 times. But even one swim can trigger it if water doesn’t drain properly. The biggest mistake? Using cotton swabs. About 65% of cases caused by injury come from people poking around their ear canals trying to dry them out. That tiny cotton tip scrapes the skin, creates micro-tears, and pushes wax deeper-exactly what bacteria need to invade.
Another common error is not drying the ears properly. Many think shaking your head or using a hairdryer on high heat helps. It doesn’t. High heat can burn the skin, and shaking isn’t enough to remove trapped water. Even showering right after swimming can wash away natural protective oils and re-wet the canal. One patient on Reddit said using a cool hairdryer, held 12 inches away for 30 seconds after every swim, stopped his four-year cycle of infections. That’s the kind of simple fix that works.
How It’s Treated: The Real Rules
Swimmer’s ear isn’t something you wait out. Left untreated, it can spread to surrounding tissue or cause chronic infection. But the good news? It responds incredibly well to the right treatment-when done correctly.
First-line treatment is antibiotic ear drops. The most common are ciprofloxacin 0.3% and hydrocortisone 1% (brand name Cipro HC). These aren’t just antibiotics-they reduce swelling too. The standard dose is 10 drops in the affected ear, twice a day for seven days. Studies show 92.4% of patients clear the infection within a week. For fungal cases (rare, about 2%), doctors prescribe clotrimazole drops for two weeks.
Pain control matters. Mild pain (about a third of cases) can be managed with acetaminophen. But for moderate to severe pain-most cases-you’ll need something stronger. Oxycodone at 0.15 mg per kg of body weight, every 4 to 6 hours, is often needed. Don’t skip this. Uncontrolled pain leads to poor sleep, missed work, and worse outcomes.
But here’s the part most people miss: keeping your ear dry during treatment is non-negotiable. A 2021 JAMA study showed that patients who didn’t protect their ears during treatment had a 63% failure rate. That’s double the failure rate of those who stayed dry. You can’t just avoid swimming-you need to avoid showers, baths, and even steam. Use a cotton ball coated in petroleum jelly to block water. Some patients use earplugs designed for showering, but they need to fit perfectly.

How to Use Ear Drops Right
Even the best drops won’t work if they don’t reach the infection. Most people squirt the drops in and immediately sit up. That’s wrong. You need to lie on your side with the infected ear up. After putting in the drops, stay still for at least five minutes. Cold drops can cause dizziness, so hold the bottle in your hand for a minute before use. Pull the earlobe up and back for adults (down and back for kids) to straighten the canal. Use a calibrated 1mL dropper-most over-the-counter bottles aren’t accurate, and dosing errors happen in 42% of cases without one.
Studies using fluorescent dye show that following this technique improves delivery to the infected area by 83%. First-timers get it right only 38% of the time. Experienced patients? 92%. That’s why some clinics now offer 12-minute instructional videos instead of just verbal instructions. If your doctor doesn’t show you how, ask for a demo or look up a trusted video from Mayo Clinic or Cleveland Clinic.
Prevention: What Actually Works
Prevention isn’t about avoiding water-it’s about managing it. Here’s what science says works:
- Alcohol-vinegar rinse: Mix 70% isopropyl alcohol with 30% white vinegar. Use 1-2 teaspoons after swimming. The alcohol dries the canal, the vinegar changes pH to stop bacterial growth. A 2022 study with 1,200 swimmers showed a 72% drop in infections.
- Custom earplugs: Silicone, moldable plugs cost $45-$120 but block 68% of moisture. Foam plugs? Only 42% effective. If you swim regularly, custom plugs pay for themselves in avoided doctor visits.
- No cotton swabs: This can’t be repeated enough. Never insert anything smaller than your elbow into your ear. If you feel wax buildup, see an audiologist. They have tools that won’t damage your canal.
- Limit post-swim water exposure: Don’t shower immediately after swimming. Wait at least two hours, or rinse off before getting in the water. Reducing moisture time by under two minutes cuts infection risk by 37%.
And if you’ve had three or more episodes in a year? You’re in the 14% of people with recurring swimmer’s ear. The biggest predictor? Continuing to use cotton swabs despite advice. One study found 87% of recurrent cases involved people who ignored the no-poking rule.
When to See a Doctor
Don’t wait until you can’t sleep. If you have severe pain, pus, or hearing loss, see a provider within 24 hours. Many patients wait days because they think it’s just a “bad earache.” But misdiagnosis is common-25% of cases are wrongly labeled as middle ear infections. That delay adds an average of 3.2 days to recovery.
Telehealth is now a real option. Devices like TytoCare let you take a clear video of your ear canal with a smartphone otoscope. Studies show they’re 89% accurate compared to in-person exams. If your clinic offers virtual visits, use them. Time-to-treatment drops from 3.2 days to just 1.1 days.
What’s New in Treatment
Antibiotic resistance is creeping in. About 8.7% of Pseudomonas strains are now resistant to ciprofloxacin. New treatments are in development, like cadazolid-otic drops, which are showing 96.3% effectiveness in early trials. The FDA approved a new hydrogel ear wick in early 2023 that holds medication in the canal three times longer than regular drops-perfect for swollen ears.
Even more exciting: microbiome-sparing treatments. Researchers are testing a therapy using harmless bacteria from your own skin (Staphylococcus hominis) to crowd out the bad ones. Early results suggest it could cut recurrence rates from 14% to under 7%. That’s a game-changer for chronic sufferers.
Why This Matters Beyond the Pain
Swimmer’s ear isn’t just a summer problem. With climate change extending swimming seasons, cases are projected to rise 12.3% by 2030. But education can offset most of that increase. Simple, consistent habits-drying ears, avoiding swabs, using vinegar rinses-can prevent the vast majority of cases.
And it’s not just about avoiding pain. Each episode costs the U.S. healthcare system an average of $117 if treated early, $312 if you go to the ER. The preventive market is growing fast-alcohol-vinegar solutions like Swim-EAR now make up 37% of sales. That’s not marketing hype. That’s people learning what works.
Can swimmer’s ear go away on its own?
Sometimes, mild cases may improve without treatment, but it’s risky. Most infections worsen without antibiotics, leading to more pain, longer recovery, and possible complications. Waiting more than 48 hours increases the chance of the infection spreading or becoming chronic. Treatment with ear drops is fast, effective, and prevents long-term damage.
Is swimmer’s ear contagious?
No, swimmer’s ear is not contagious. You can’t catch it from someone else. It’s caused by bacteria or fungi that grow in your own ear canal when moisture and skin damage create the right environment. Sharing towels or earbuds won’t spread it-but sharing cotton swabs can damage your own ears and increase your risk.
Can I swim while I have swimmer’s ear?
No. Swimming during treatment can reintroduce water, delay healing, and increase failure rates by 40%. Avoid all water exposure-including showers-for the full 7-day course. Use waterproof ear protection or cotton balls with petroleum jelly if you must bathe. Return to swimming only after your doctor confirms the infection is fully cleared.
Why do my ears still feel blocked after treatment?
It’s normal to feel fullness or muffled hearing for a few days after the infection clears. Swelling in the ear canal takes time to go down completely. If the feeling lasts more than a week, or if you have new pain, drainage, or dizziness, return to your provider. You might have residual wax buildup or a minor reaction to the drops.
Are over-the-counter ear drops safe for swimmer’s ear?
Most OTC ear drops are designed for earwax removal or mild irritation, not bacterial infections. They won’t cure swimmer’s ear. Some contain alcohol or vinegar, which can help prevent infection-but if you already have symptoms, you need prescription antibiotic drops. Using the wrong drops can mask symptoms and delay proper treatment.


November 14, 2025 AT 21:34
Been swimming every weekend for years and never had swimmer’s ear until I started using cotton swabs after dives. Stopped using them and started the vinegar-alcohol rinse after every swim. No more infections in 18 months. Simple stuff works if you actually do it.