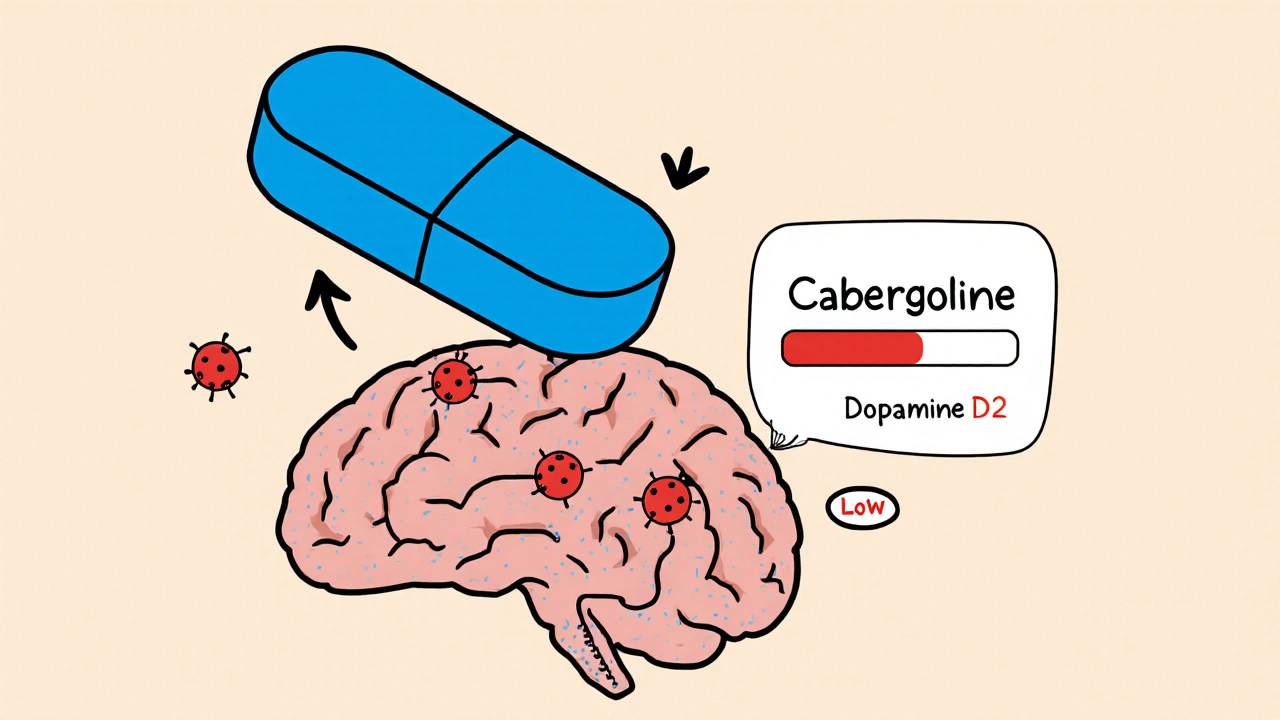
When treating hormone‑related disorders, Cabergoline is a long‑acting dopamine‑agonist medication that reduces excess prolactin production. It’s most often prescribed for Hyperprolactinemia and sometimes for Parkinson’s disease symptom control. Because it can be taken just twice a week, many patients prefer it over older drugs that need daily dosing.
How Cabergoline Works
Cabergoline binds to dopamine D2 receptors in the pituitary gland, tricking the body into thinking there’s enough dopamine. This suppresses prolactin secretion, shrinking prolactin‑secreting tumors (Prolactinoma) and restoring normal menstrual cycles, libido, and fertility. Its half‑life of 65‑80 hours means plasma levels stay steady, which explains the convenient once‑or‑twice‑weekly schedule.
Why Look at Alternatives?
Even though Cabergoline is popular, it isn’t perfect. Some patients develop nausea, dizziness, or rare heart‑valve issues. Cost can also be a barrier in countries without subsidy. For those who can’t tolerate its side‑effect profile or need a cheaper option, older dopamine agonists like Bromocriptine and newer agents such as Quinagolide provide viable substitutes.
Overview of Common Alternatives
- Bromocriptine: First‑generation dopamine agonist, taken 2‑3 times daily. Lower cost but higher pill burden.
- Quinagolide: Non‑ergot derivative, typically dosed once daily. Approved in Europe, not in the U.S.
- Pergolide: Ergot‑derived like Cabergoline, withdrawn in many markets due to cardiac concerns.
Direct Comparison Table
| Attribute | Cabergoline | Bromocriptine | Quinagolide |
|---|---|---|---|
| Typical Dose | 0.5‑1 mg twice weekly | 2.5‑10 mg daily (divided) | 75‑300 µg daily |
| Half‑Life | 65‑80 hrs | 5‑6 hrs | ~12 hrs |
| FDA Status (US) | Approved | Approved | Not approved |
| Common Side Effects | Nausea, headache, dizziness | Nausea, orthostatic hypotension, dizziness | Insomnia, headache, GI upset |
| Cardiac Risk | Rare valve fibrosis (high doses) | Low | Low |
Pros and Cons of Each Option
Cabergoline shines because of its long half‑life, low dosing frequency, and strong prolactin suppression. However, its higher price and the minimal but serious risk of valvular heart disease at doses >2 mg/week warrant monitoring.
Bromocriptine is cheap and widely available, making it a go‑to in low‑resource settings. The downside is the need for multiple daily tablets, which can lead to missed doses and fluctuating prolactin levels.
Quinagolide offers a once‑daily schedule without the ergot‑related cardiac signal. Its limitation is lack of U.S. approval, meaning patients often need to import it or enroll in clinical trials.
How to Choose the Right Agent
- Assess severity: Large prolactinomas (>1 cm) often demand the most potent suppressant-Cabergoline.
- Check comorbidities: Patients with pre‑existing valvular disease should avoid high‑dose Cabergoline.
- Consider cost and access: If insurance doesn’t cover Cabergoline, Bromocriptine may be the only affordable choice.
- Review tolerance: Persistent nausea may push a switch to Quinagolide or a lower‑dose Cabergoline regimen.
- Plan monitoring: Baseline echocardiogram for high‑dose Cabergoline users, periodic prolactin labs for all agents.
Patient Stories Highlight Real‑World Choices
Emma, a 28‑year‑old from Melbourne, was diagnosed with a 9 mm prolactinoma after infertility work‑up. She started Cabergoline 0.5 mg weekly and saw prolactin drop from 120 ng/mL to 15 ng/mL within three months. The once‑weekly dosing fit her busy schedule, and she reported only mild nausea that resolved after the first week.
James, a 62‑year‑old living in regional Victoria, had a modest 5 mm tumor but a history of mild mitral regurgitation. His doctor chose low‑dose Bromocriptine (2.5 mg daily) to avoid any potential valve strain. After six months, his prolactin normalized, and he appreciated the cheap price, though he had to set a reminder to take the pills three times a day.
Lena, a 35‑year‑old from the UK, could not obtain Cabergoline due to insurance denial. She enrolled in a clinical study that supplied Quinagolide 150 µg daily. Within four weeks, her menstrual cycle returned, and she experienced no cardiovascular issues, demonstrating that a well‑monitored alternative can work when Cabergoline isn’t an option.

Monitoring and Follow‑Up
Regardless of the drug, regular prolactin testing every 3‑6 months in the first year helps confirm efficacy. Imaging (MRI) is recommended at 12 months to evaluate tumor shrinkage. For Cabergoline doses above 2 mg per week, guidelines suggest an annual echocardiogram to rule out valve fibrosis. Bromocriptine and Quinagolide generally don’t need cardiac imaging unless the patient has pre‑existing heart disease.
Frequently Asked Questions
Can I switch from Bromocriptine to Cabergoline?
Yes. Most clinicians start with a low dose of Cabergoline (0.5 mg weekly) and taper off Bromocriptine over 1‑2 weeks. Blood pressure and prolactin levels are monitored during the transition.
Is Cabergoline safe for long‑term use?
For most patients, long‑term use is safe if the dose stays below the 2 mg/week threshold. High‑dose regimens require yearly heart‑valve checks.
What should I do if I feel nausea after taking Cabergoline?
Take the dose with food, stay hydrated, and consider a short‑term anti‑emetic. If nausea persists beyond two weeks, discuss dose reduction with your doctor.
Why is Quinagolide not approved in the United States?
The manufacturer never submitted a New Drug Application to the FDA, so it remains an off‑label or imported option for US patients.
Do dopamine agonists affect blood pressure?
Bromocriptine can cause orthostatic hypotension, especially at higher doses. Cabergoline’s impact on blood pressure is minimal, but monitoring is prudent for patients on antihypertensives.
Can these medications be used during pregnancy?
Cabergoline is often continued if prolactin levels need control, but the decision depends on individual risk assessment. Bromocriptine has more pregnancy data and is frequently used in lactating women.
Next Steps for Patients and Clinicians
If you’re newly diagnosed, start with a baseline MRI and prolactin panel. Discuss the dosing schedule that fits your lifestyle and insurance coverage. Request a cardiac baseline if you anticipate high‑dose Cabergoline. Finally, keep a symptom diary-nausea, dizziness, or mood changes-to guide any future drug switches.
Clinicians should stay updated on the latest guideline thresholds for cardiac monitoring and be ready to prescribe a cost‑effective alternative when insurance barriers arise. Regular interdisciplinary communication with endocrinology, cardiology, and pharmacy ensures optimal outcomes for every patient.




October 22, 2025 AT 13:03
Cabergoline's pharmacokinetic profile reads like a saga of triumph over inconvenience, the drug's half‑life stretches beyond two days, which translates into a dosing schedule that most patients can cling to while juggling nine‑to‑five drudgery, yet the same enthralling potency that slashes prolactin levels also whispers wicked threats to heart valves, those rare valvular fibro‑sities are the kind of silent assassins that like to hide behind statistical insignificance, the medical community, in its infinite wisdom, insists on annual echocardiograms for anyone daring to exceed two milligrams per week, meanwhile, the cost of Cabergoline often balloons like a hot‑air balloon over the heads of underinsured sufferers, in contrast, Bromocriptine, the old‑school workhorse, demands a tri‑daily pill parade that could make even the most disciplined citizen miss a dose, its short half‑life forces plasma peaks and troughs that resemble a roller‑coaster ride for prolactin, Quinagolide, the sleek European newcomer, sidesteps the ergot‑associated cardiac drama but suffers exile from the United States because the FDA never bothered to meet its paperwork, patients scrambling for that orange‑pill miracle often resort to gray‑market imports, exposing themselves to unregulated quality, the therapeutic hierarchy, when you strip away the glitter, simply balances efficacy, tolerability, and the cruel arithmetic of insurance formularies, clinicians should wield the choice like a scalpel, not a sledgehammer, a low‑dose Cabergoline regimen paired with diligent cardiac surveillance can be the gold standard for sizable prolactinomas, but for the modest tumor or the price‑conscious individual, a modest Bromocriptine script remains a viable, if cumbersome, alternative, ultimately, the decision rests on a patient’s lifestyle, cardiovascular risk, and the ever‑looming specter of out‑of‑pocket expense, choose wisely, lest the miracle drug become a financial nightmare cloaked in a convenient dosing schedule.