Irritable Bowel Syndrome: Causes, Triggers, and Practical Management
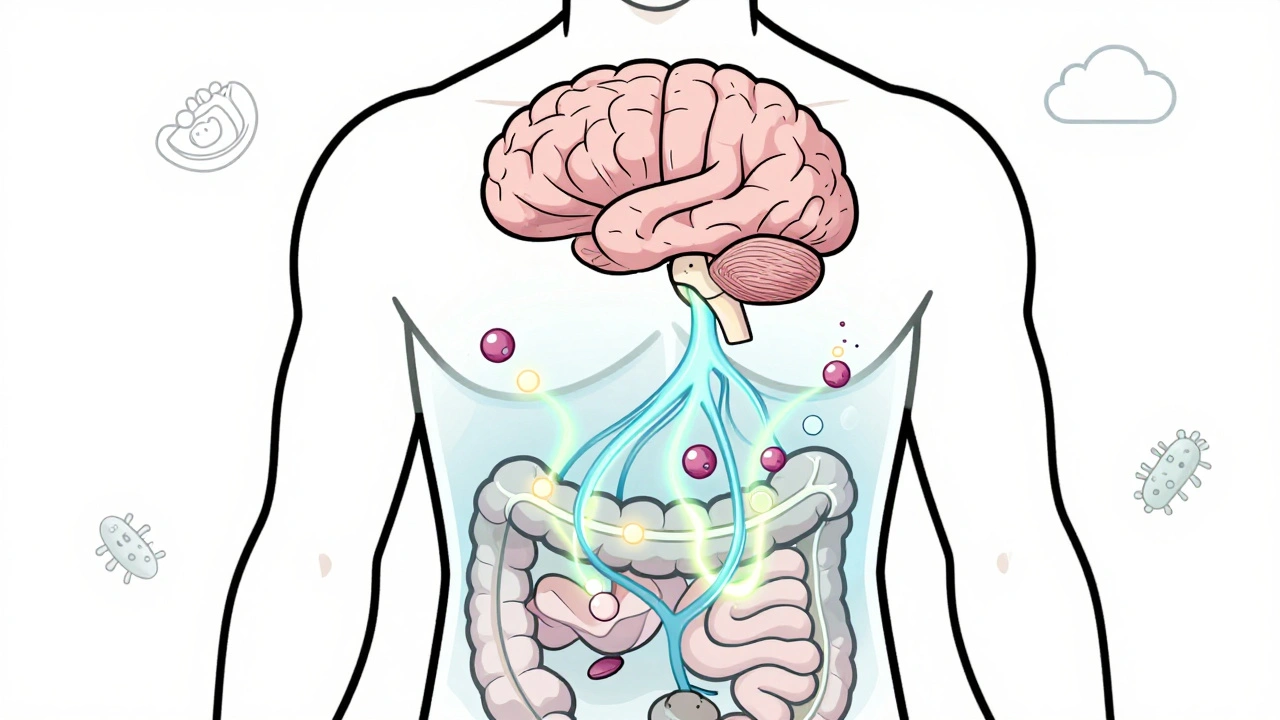
When your gut acts up without a clear reason—bloating after meals, sudden cramps, or switching between constipation and diarrhea—you might be dealing with irritable bowel syndrome, a functional gastrointestinal disorder characterized by chronic abdominal discomfort and altered bowel habits without structural damage. Also known as spastic colon, it’s not an infection, not cancer, and not something you can see on a scan—but it’s very real, and it affects more than 1 in 10 people worldwide. Unlike inflammatory diseases, IBS doesn’t damage the intestines, but it can wreck your daily life. People with IBS often feel dismissed because tests come back normal. But normal labs don’t mean normal symptoms. The problem lives in the brain-gut connection, where stress, food, and even gut bacteria send mixed signals that turn normal digestion into a painful mess.
What triggers IBS varies wildly. For some, it’s gluten or dairy. For others, it’s coffee, artificial sweeteners, or even just eating too fast. gut microbiome, the collection of bacteria living in your digestive tract that influences digestion, immunity, and even mood plays a huge role. Studies show people with IBS often have less diverse gut bacteria than those without it. And stress, a psychological factor that directly impacts gut motility and sensitivity through the vagus nerve doesn’t just make symptoms worse—it can turn a quiet flare into a full-blown episode. You can’t just take a pill and fix it. Managing IBS means learning your personal triggers, adjusting what you eat, and finding ways to calm your nervous system.
There’s no one-size-fits-all cure, but there are proven ways to reduce flare-ups. Low-FODMAP diets have helped many people track down food triggers with real results. Probiotics, especially strains like Bifidobacterium infantis, show promise in easing bloating and irregularity. Even simple habits—like chewing slowly, drinking enough water, and walking after meals—can make a difference. And while medications exist for specific symptoms, most people find long-term relief through lifestyle tweaks, not pills. The goal isn’t to eliminate IBS, but to take back control so it doesn’t run your schedule.
Below, you’ll find real-world guides on how other people manage their symptoms, what medications help (and what doesn’t), and how to spot when something else might be going on. Whether you’re just starting to figure out your gut issues or you’ve been living with this for years, these posts give you clear, no-fluff advice based on actual patient experiences and clinical evidence.
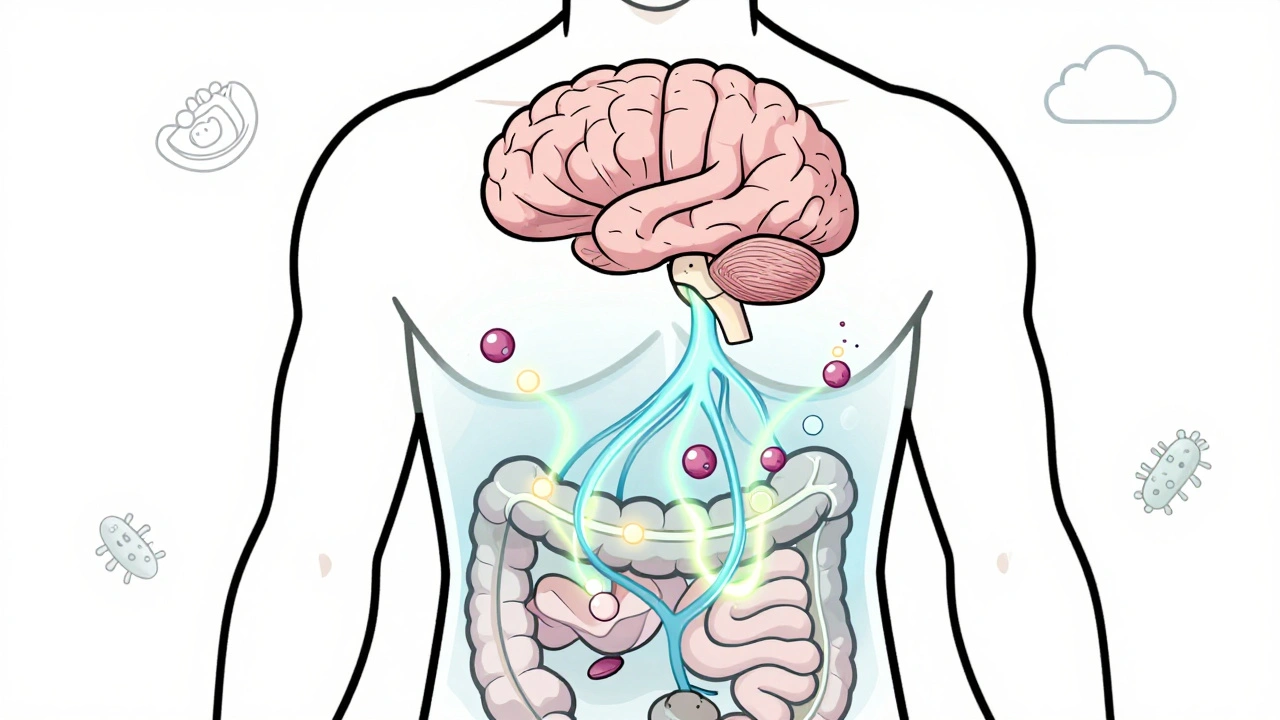
Irritable Bowel Syndrome is not just a digestive issue-it's a breakdown in gut-brain communication. Learn how serotonin, gut bacteria, and brain wiring affect symptoms-and what treatments actually work.