For millions of people worldwide, abdominal pain, bloating, and unpredictable bowel changes aren’t just annoying-they’re life-limiting. If you’ve been told it’s "just stress" or "all in your head," you’re not alone. But here’s the truth: irritable bowel syndrome isn’t a psychological disorder. It’s a real, measurable breakdown in communication between your gut and your brain.
The Gut-Brain Axis Isn’t Metaphor-It’s Biology
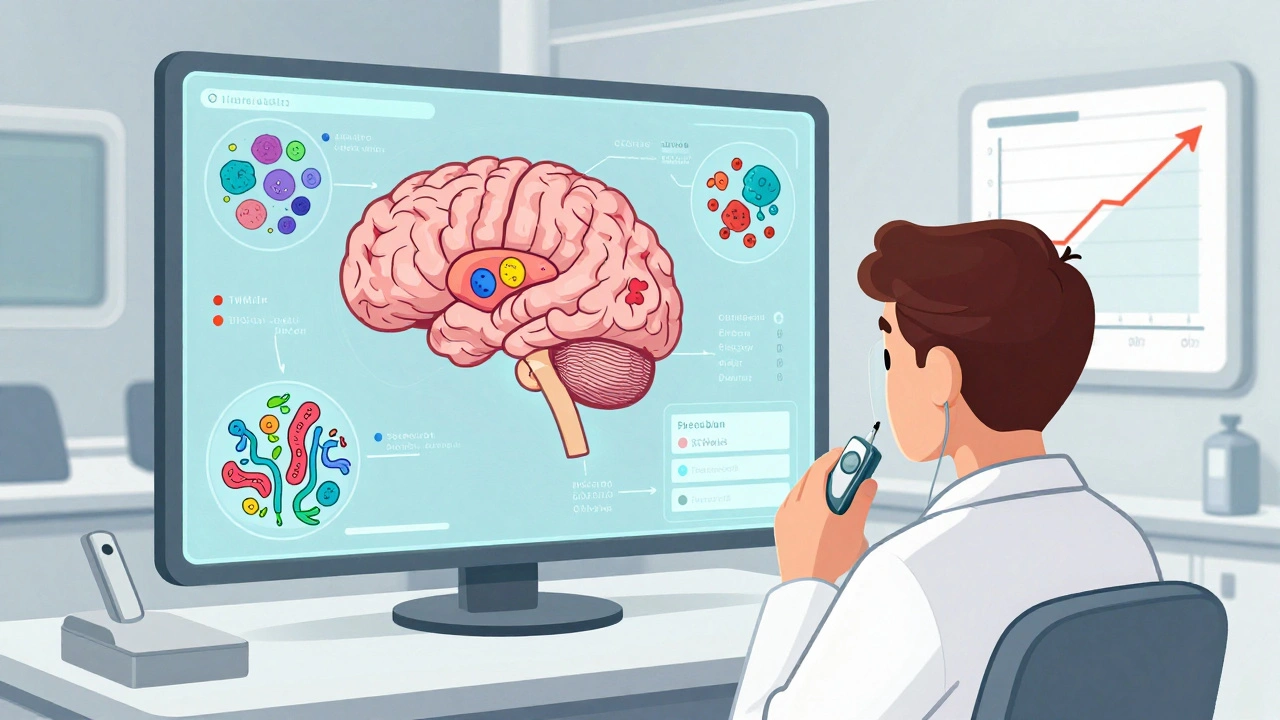
For decades, IBS was treated like a simple bowel problem. Doctors focused on motility, inflammation, or food intolerances. But starting in the 2000s, brain scans and blood tests began revealing something deeper: people with IBS have measurable differences in how their brains process signals from their guts.
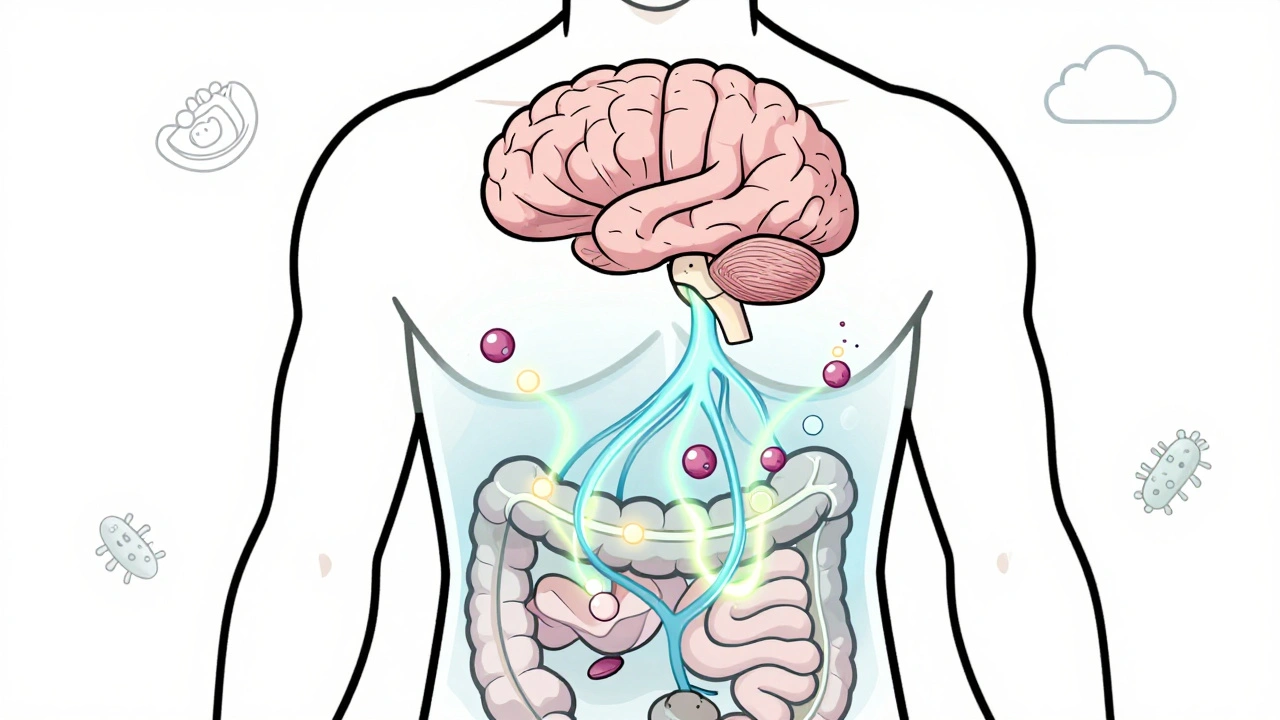
This isn’t speculation. It’s science. The gut-brain axis is a two-way highway made of nerves, hormones, and immune signals. Your gut has its own nervous system-the enteric nervous system-with over 100 million neurons. That’s more than your spinal cord. It talks directly to your brain through the vagus nerve. When this line breaks down, your brain misreads gut signals. A normal stretch in your intestine? Your brain hears it as pain. A slight delay in digestion? Your brain interprets it as urgency.
Studies show people with IBS have less gray matter in areas that control emotion and pain filtering-like the prefrontal cortex. Meanwhile, areas that detect bodily sensations, like the insula and hypothalamus, become overactive. It’s like your brain’s volume knob for gut signals is stuck on high.
Why Serotonin Is the Key Player (And Why It’s Not Just About Mood)
You’ve heard serotonin is the "happy chemical." But here’s the twist: 95% of your body’s serotonin is made in your gut-not your brain. Enterochromaffin cells in your intestinal lining produce it to control movement, secretion, and pain sensing.
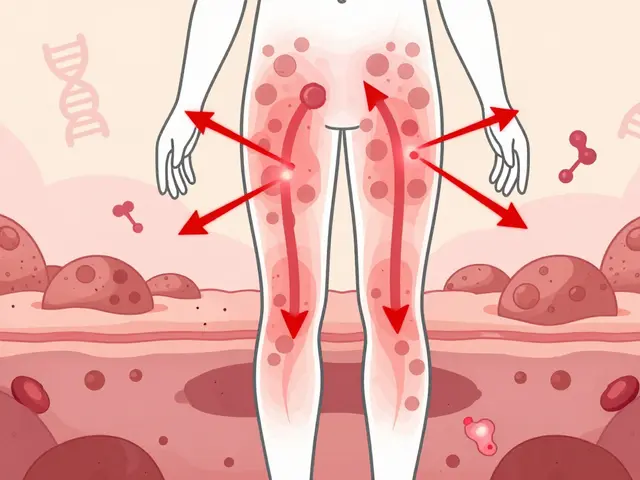
In IBS-D (diarrhea-predominant), these cells pump out too much serotonin-up to 60% more than in healthy people. That speeds up digestion, causes urgency, and triggers cramping. In IBS-C (constipation-predominant), serotonin levels drop. The gut slows down. Stools harden. Pain builds.
This isn’t random. It’s why drugs like alosetron (for IBS-D) and prucalopride (for IBS-C) work. They don’t just mask symptoms-they tweak the serotonin system directly. But they’re not magic. They help about half the people who take them. And side effects can be serious. That’s why newer treatments are focusing on the whole system, not just one chemical.
The Microbiome Isn’t Just Bacteria-It’s a Communication Network
Your gut isn’t sterile. It’s home to trillions of microbes. And they’re not just along for the ride-they’re active players in the gut-brain conversation.
People with IBS often have imbalances in Firmicutes and Bacteroidetes, two major bacterial groups. These microbes don’t just digest fiber-they produce short-chain fatty acids, neurotransmitters, and immune signals that reach the brain. Some strains, like Bifidobacterium infantis 35624, have been shown in clinical trials to reduce bloating and pain in 30-40% of users. That’s better than placebo, but not a cure.
Fecal transplants (FMT) have shown promise too-some studies report up to 60% symptom improvement. But results are inconsistent. Why? Because the microbiome is personal. What works for one person might do nothing-or make things worse-for another. That’s why the future isn’t one-size-fits-all probiotics. It’s personalized microbiome mapping.

Diet Changes Work-But Not Because You’re "Sensitive"
The low-FODMAP diet isn’t a fad. It’s backed by over 20 randomized trials. About 50-76% of people with IBS see real improvement. But here’s what most people don’t realize: FODMAPs don’t cause inflammation. They don’t damage your gut. They just ferment too fast.
When you eat onions, garlic, apples, or wheat, the sugars in them (fructans, fructose, lactose) get pulled into the small intestine. Your body can’t fully absorb them. So they rush into the colon, where bacteria feast on them. That creates gas. That gas stretches the bowel. And if your brain is already hypersensitive, that stretch feels like a cramp.
The diet works because it removes the triggers-not because you’re allergic. The key is doing it right: strict elimination for 4-6 weeks, then careful reintroduction. Most people quit too early. Others stay on it too long and risk nutrient gaps. Working with a dietitian isn’t optional-it’s essential.
Gut-Directed Hypnotherapy: The Silent Game-Changer
Imagine a treatment that works better than most medications, has zero side effects, and lasts for years. That’s gut-directed hypnotherapy.
In clinical trials, 70-80% of IBS patients who completed 7-12 sessions saw major symptom relief. At six months, most still felt better. Compare that to standard care-only 35-40% improve. And unlike drugs, hypnotherapy doesn’t just mask pain. It retrains your brain.
During sessions, you’re guided into a relaxed state while listening to recordings that help you visualize your gut calming down. Your brain learns to interpret gut signals differently. Over time, the pain pathways quiet down. It’s like cognitive behavioral therapy for your intestines.
It’s not woo. It’s neuroscience. And it’s available-though hard to find. In rural areas, there’s roughly one certified practitioner for every 500,000 people. Online programs are helping bridge the gap, but quality varies. Look for those backed by universities or hospitals.
Why So Many People Are Still Struggling
Here’s the ugly truth: most people with IBS wait 3-7 years to get diagnosed. They see five or more doctors. They’re told they’re anxious, overeating, or "just need to relax."
Even after diagnosis, treatment is patchy. Many doctors still treat IBS like a stomach bug. They prescribe loperamide or antispasmodics-drugs that help a little, but often cause dizziness, dry mouth, or constipation. Nearly half of patients stop taking them within three months.
Cost is another barrier. Gut-directed hypnotherapy can cost $1,200-$2,500 out-of-pocket. The low-FODMAP diet requires time, planning, and sometimes expensive specialty foods. Insurance rarely covers it.
And here’s the kicker: people who understand the gut-brain axis stick to treatment better. One survey found that those who learned how their brain and gut connect had 30% higher adherence and 25% greater symptom improvement. Knowledge isn’t just power-it’s healing.
What’s Next? The Future of IBS Treatment
The IBS market is booming. Companies are pouring money into therapies that target the gut-brain axis directly. In 2023, a new blood test called VisceralSense™ started measuring 12 microbial metabolites and serotonin ratios to predict which treatment will work for you. Accuracy? 85%.
Drugs like etrasimod, which modulates immune signaling in the gut, showed 52% symptom improvement in phase III trials-far outperforming placebo. Transcutaneous vagus nerve stimulation (tVNS), a non-invasive device you wear behind the ear, is showing promise in early trials. And the NIH just launched a $15 million project to build personalized treatment algorithms based on your unique gut-brain profile.
This isn’t science fiction. It’s happening now. The goal isn’t to cure IBS. It’s to turn it from a chronic, unpredictable condition into a manageable one-like diabetes or high blood pressure.
What You Can Do Today
You don’t need to wait for the next breakthrough. Start here:
- Learn the basics of the gut-brain axis. Understanding why your body reacts this way reduces fear-and fear makes symptoms worse.
- Try the low-FODMAP diet with a dietitian. Don’t guess. Track what you eat and how you feel.
- Look into gut-directed hypnotherapy. Search for programs certified by the American Society of Clinical Hypnosis or similar bodies.
- Ask your doctor about serotonin-targeted meds if diet and therapy don’t help. Don’t assume they’re all risky-some are safer than you think.
- Join a community. Reddit’s r/IBS has over 140,000 people sharing what works. You’re not alone.
IBS isn’t your fault. It’s not weakness. It’s a biological miscommunication. And the good news? We’re finally learning how to fix it-not by silencing symptoms, but by restoring the conversation between your gut and your brain.



December 2, 2025 AT 14:59
IBS is just stress.