CCB Drug Interaction Checker
Check Your Medication Safety
Identify potential interactions between your calcium channel blocker and other medications, foods, or supplements
Interaction Results
Key information: CCBs are metabolized by CYP3A4 enzyme. When combined with inhibitors, levels can rise dangerously.
Calcium channel blockers (CCBs) are among the most commonly prescribed heart medications in the U.S., with over 50 million people using them to treat high blood pressure, chest pain, and irregular heartbeats. But behind their widespread use lies a hidden risk: how your body processes these drugs can change dramatically depending on what else you’re taking. Some CCBs can become dangerously strong when mixed with common medications, foods, or even supplements. Others are much safer. Knowing the difference isn’t just helpful-it can be life-saving.
How Calcium Channel Blockers Work and Why Metabolism Matters
Calcium channel blockers stop calcium from entering heart and blood vessel cells. This relaxation of blood vessels lowers blood pressure and reduces the heart’s workload. But how your body breaks down these drugs determines how long they last, how strong their effect is, and whether they’ll cause side effects.
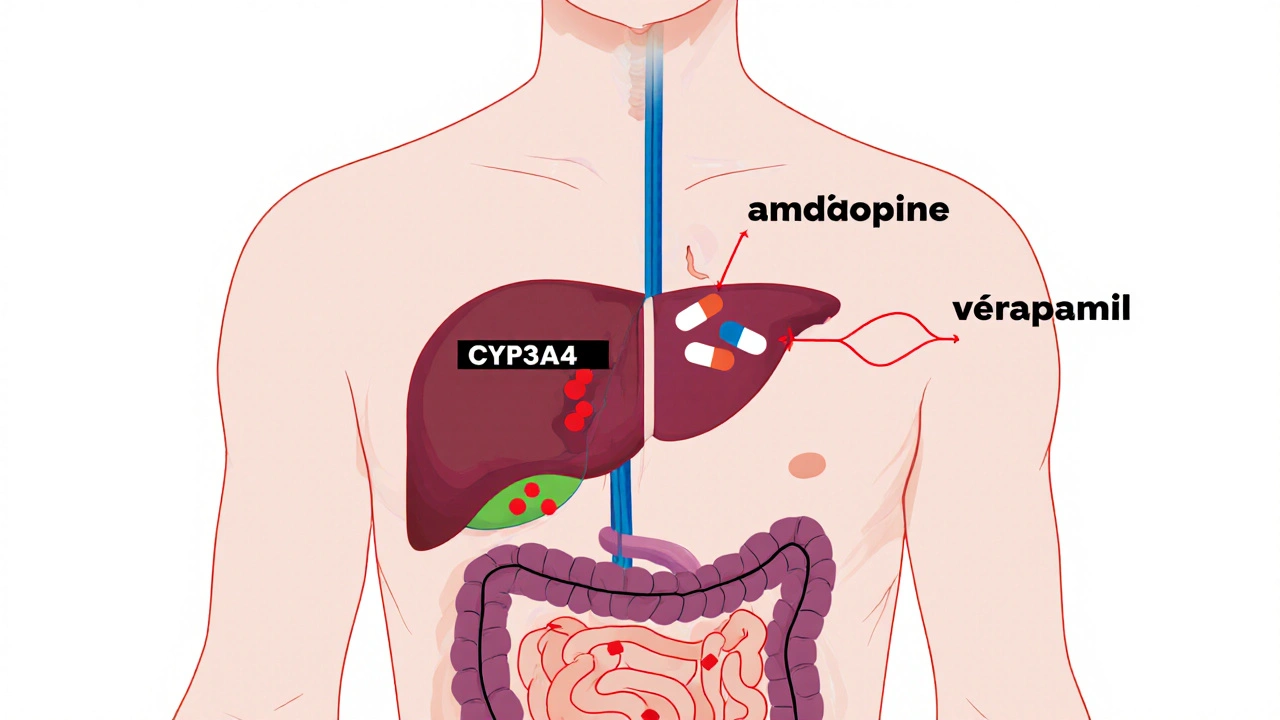
Most CCBs are processed by an enzyme called CYP3A4, found mainly in the liver and intestines. This enzyme is like a gatekeeper-it breaks down many drugs so they can be cleared from your body. But if something blocks or slows down CYP3A4, the CCB builds up in your bloodstream. That’s when you risk dangerously low blood pressure, slow heart rate, dizziness, or even heart block.
Not all CCBs are the same. They’re split into two groups: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine; and non-dihydropyridines (non-DHPs) like verapamil and diltiazem. DHPs mainly affect blood vessels. Non-DHPs also slow the heart’s electrical system. This difference matters because non-DHPs are more likely to interfere with other drugs-and be interfered with themselves.
Why Amlodipine Is the Safest Choice for Most People
If you’re on multiple medications, amlodipine is often the best CCB option. It’s metabolized by CYP3A4, but unlike verapamil or diltiazem, it doesn’t block the enzyme. That means it’s less likely to cause dangerous interactions.
When a patient takes a strong CYP3A4 inhibitor like ketoconazole or clarithromycin, verapamil’s blood levels can spike by 60-70%. Amlodipine’s levels rise by only about 40%. That might sound similar, but the consequences aren’t. Verapamil can cause heart block or fainting at high levels. Amlodipine rarely does. Studies show that only 12% of patients on amlodipine need a dose change when taking moderate CYP3A4 inhibitors. For diltiazem, it’s 45%.
Another advantage: amlodipine has a long half-life-30 to 50 hours. That means one daily dose keeps blood pressure steady. Verapamil, with a half-life of just 4-12 hours, needs to be taken twice a day. More doses mean more chances for interaction errors.
Doctors now recommend starting with amlodipine 2.5 mg daily in older adults or those on multiple drugs. About 78% of clinics follow this guideline. It’s not just theory-it’s cutting hospital visits.
The Dangerous Duo: Grapefruit Juice and CCBs
Grapefruit juice isn’t just a healthy breakfast addition-it’s a silent drug amplifier. It blocks CYP3A4 in the gut, so more of the CCB enters your bloodstream before it’s broken down.
On patient forums, 68% of users who reported unexpected low blood pressure were taking grapefruit juice with their CCB. Forty-seven cases required emergency care. The effect is strongest with felodipine and nifedipine. Amlodipine is less affected, but even it can rise by 30% in concentration with regular grapefruit juice use.
The FDA warns that grapefruit juice can make some CCBs as potent as doubling the dose. One glass in the morning can affect drug levels for up to 72 hours. That’s why pharmacists now routinely ask: “Do you drink grapefruit juice?” before filling a CCB prescription.

Verapamil and Diltiazem: High Risk, High Reward
Verapamil and diltiazem are powerful for controlling heart rhythm, but they come with heavy baggage. Both are not just metabolized by CYP3A4-they actively inhibit it. That means they don’t just get affected by other drugs; they change how other drugs are processed.
Diltiazem can make simvastatin (a cholesterol drug) 400% more potent. That raises the risk of muscle damage, kidney failure, or even rhabdomyolysis. Verapamil increases digoxin levels by 50-75% by blocking a transporter called P-glycoprotein. Digoxin toxicity can cause fatal heart rhythms.
Because of this, the European Society of Cardiology explicitly says: do not use verapamil with strong CYP3A4 inhibitors. That includes antifungals like itraconazole, antibiotics like clarithromycin, and HIV drugs like ritonavir. These combinations have caused 17 documented cases of complete heart block-requiring pacemakers.
Even when used alone, non-DHPs need careful monitoring. Trough levels of verapamil should stay between 50-150 ng/mL. But only 32% of community pharmacies test for this. Most rely on symptoms-dizziness, slow pulse, swelling-which often appear too late.
Age, Kidneys, and the Hidden Risk of Polypharmacy
Older adults are at the highest risk. By age 65, the body’s ability to metabolize drugs drops by 30-50%. Kidney function declines too. But here’s the twist: CCBs are mostly cleared as metabolites through the kidneys. Less kidney function means those metabolites hang around longer.
Patients over 65 have 3.2 times more severe interactions than younger patients. Those with kidney disease (eGFR under 60) see interaction severity jump by 47%. That’s why FDA guidelines say: reduce verapamil by 50% if your kidney function is between 30-60 mL/min. Amlodipine? No adjustment needed.
And most older adults aren’t on just one drug. Over 58% of Medicare patients take five or more medications. Statins, antidepressants, painkillers, antifungals-all can interfere. One patient taking amlodipine, atorvastatin, and fluconazole might be fine. Add grapefruit juice and clarithromycin? That’s a storm waiting to happen.
What You Should Do: A Practical Guide
Here’s how to stay safe with calcium channel blockers:
- Know your CCB. If you’re on verapamil or diltiazem, assume you’re at higher risk. Amlodipine is safer.
- Avoid grapefruit juice. Not just the fruit-juice, smoothies, even some candies contain it.
- Review all your meds. Tell your doctor and pharmacist every pill, supplement, and herb you take. Even over-the-counter ones like St. John’s Wort (which lowers CCB levels) or turmeric (which can inhibit CYP3A4).
- Watch for symptoms. Unexplained dizziness, swelling in the ankles, slow pulse, fainting, or extreme fatigue could mean your CCB level is too high.
- Ask about testing. If you’re on verapamil or diltiazem with other high-risk drugs, ask if therapeutic drug monitoring is right for you.
Community pharmacists spend over 12 minutes per CCB prescription checking for interactions. That’s because they’ve seen the results: 18% of CCB prescriptions need changes to avoid harm.
The Future: Personalized Dosing and Real-Time Alerts
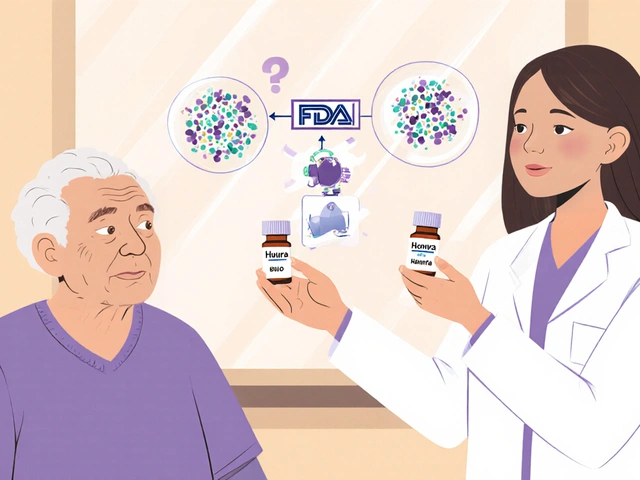
The tide is turning. In 2023, the FDA approved CCB-Check, a tool that integrates with electronic health records to warn doctors in real time if a CCB interaction is likely. Hospitals using it saw a 31% drop in hospitalizations from CCB-related issues.
Research is now looking at genetics. About 27% of people have CYP3A4 gene variants that make them slow or fast metabolizers. A slow metabolizer on standard verapamil might need half the dose. A fast metabolizer might need more.
By 2027, personalized dosing based on liver function, kidney health, genetics, and current medications will likely be standard. Until then, the safest approach is simple: choose amlodipine when possible, avoid grapefruit, and always tell your provider what else you’re taking.
Calcium channel blockers save lives. But they’re not harmless. Their power lies not just in what they do-but in how your body handles them. Get that right, and you avoid danger. Get it wrong, and the consequences can be severe.
Can I take calcium channel blockers with statins?
It depends on the statin and the CCB. Simvastatin and lovastatin are broken down by CYP3A4, so combining them with diltiazem or verapamil can raise statin levels dangerously-by up to 400%. This increases the risk of muscle damage. Amlodipine is safer with statins. Atorvastatin is also less risky than simvastatin. Always ask your pharmacist to check for interactions before starting both drugs together.
Does grapefruit juice affect all calcium channel blockers the same way?
No. Felodipine and nifedipine are most affected-blood levels can double. Amlodipine is affected too, but less so, with about a 30% increase. Verapamil and diltiazem are less impacted by grapefruit juice because their absorption isn’t as dependent on gut CYP3A4. Still, no CCB is completely safe with grapefruit. The safest choice is to avoid it entirely.
Why is amlodipine preferred over verapamil for older patients?
Amlodipine has a longer half-life (30-50 hours), so it’s dosed once daily, reducing the chance of missed doses or overdosing. It doesn’t slow heart rate as much, making it safer for people with existing slow rhythms. It also doesn’t inhibit CYP3A4, so it’s less likely to interfere with other medications. And unlike verapamil, it doesn’t need dose adjustments for kidney problems. These factors make it the top choice for seniors on multiple drugs.
Can I stop my calcium channel blocker if I start a new medication?
Never stop a CCB without talking to your doctor. Stopping suddenly can cause rebound high blood pressure, chest pain, or even a heart attack. If a new drug interacts with your CCB, your doctor may switch you to a safer alternative like amlodipine, adjust the dose, or monitor you closely. Never make changes on your own.
How do I know if my calcium channel blocker is causing an interaction?
Watch for signs like sudden dizziness, fainting, very slow pulse (under 50 bpm), swelling in legs or ankles, extreme fatigue, or shortness of breath. If you’ve recently started a new medication, supplement, or started drinking grapefruit juice, these could be red flags. Check your blood pressure at home if possible. If you notice any of these, contact your doctor right away. Don’t wait for symptoms to get worse.





November 30, 2025 AT 13:49
Okay so let me get this straight - grapefruit juice turns your blood pressure med into a sledgehammer? I drank a whole damn glass this morning and now I’m dizzy as hell. My pharmacist looked at me like I’d just confessed to summoning Cthulhu. Don’t let your breakfast kill you, people.