Most people don’t realize that nearly two out of three people under 50 carry one form of herpes simplex virus. It’s not rare. It’s not exotic. It’s common - and often misunderstood. HSV-1 and HSV-2 are not the same, even though they look alike. One causes cold sores. The other is linked to genital outbreaks. But today, that line is blurring. More than half of new genital herpes cases in the U.S. are now caused by HSV-1, not HSV-2. That shift changed everything - from how doctors treat it to how people live with it.
What Are HSV-1 and HSV-2?
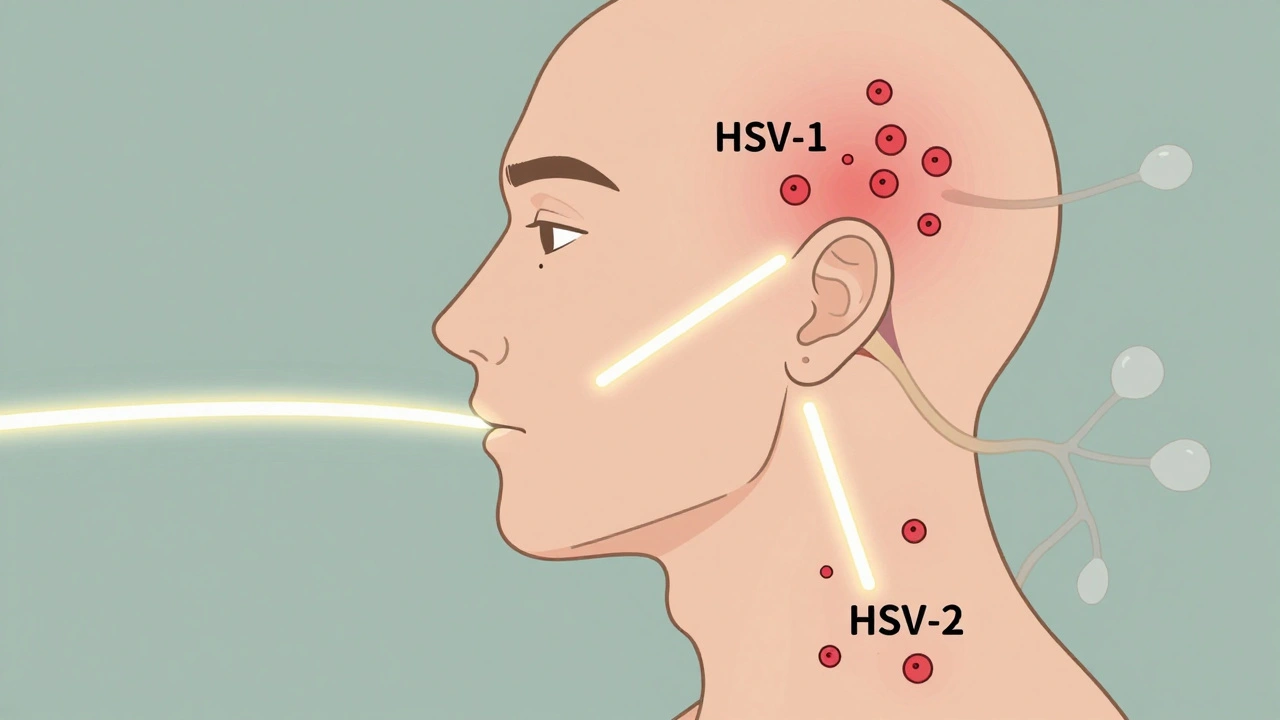
Herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) are two distinct viruses that share about half their DNA. Both are enveloped, double-stranded DNA viruses that invade nerve cells and stay there for life. After the first infection, they retreat to sensory ganglia - HSV-1 hides in the trigeminal ganglion near your ear, while HSV-2 settles in the sacral nerves at the base of your spine. They don’t cause symptoms all the time. In fact, most people never know they have it until an outbreak happens - or until they get tested.
HSV-1 is mostly known for oral herpes. It causes cold sores or fever blisters around the mouth. But in the last 20 years, it’s become the leading cause of new genital herpes infections in high-income countries. Studies show it now accounts for 30-50% of genital cases. HSV-2, on the other hand, remains the main cause of recurrent genital outbreaks. About 70-80% of genital herpes cases are still HSV-2. But here’s the key difference: HSV-1 genital infections recur far less often - about 0.2 to 0.5 times a year. HSV-2 recurs 4 to 5 times a year on average.
What Do Outbreaks Look Like?
An outbreak doesn’t start with blisters. It starts with a warning. A tingling, burning, or itching sensation in the area where the virus lives. This prodrome lasts less than six hours in recurrent HSV-1 cases, but can stretch longer with HSV-2. Within a day or two, small fluid-filled blisters appear. They cluster, burst, turn into open sores, then crust over. Healing takes 7 to 21 days for a first outbreak. Recurrences heal faster - usually in 5 to 10 days.
Primary oral HSV-1 infection in children often looks like herpetic gingivostomatitis. Fever spikes to 39°C or higher. Mouth ulcers make eating and drinking painful. Swollen gums, bad breath, and trouble swallowing are common. About 5-10% of these kids end up in the hospital for IV fluids.
Primary genital HSV-2 is even more intense. Nine out of ten people with their first outbreak report painful ulcers. Most have trouble urinating. Nearly two-thirds feel swollen lymph nodes in the groin. Over half report discharge. About 4 in 10 get fevers and muscle aches. It’s not just uncomfortable - it’s exhausting. One Reddit user described it: “First outbreak lasted 18 days. Fever hit 39.2°C. Twelve ulcers. Couldn’t pee without lidocaine.”
Asymptomatic Shedding Is Real
You don’t need symptoms to spread HSV. That’s the hardest part for people to accept. Both HSV-1 and HSV-2 can shed virus from skin or mucous membranes even when there’s no sore, no tingling, no sign of anything wrong.
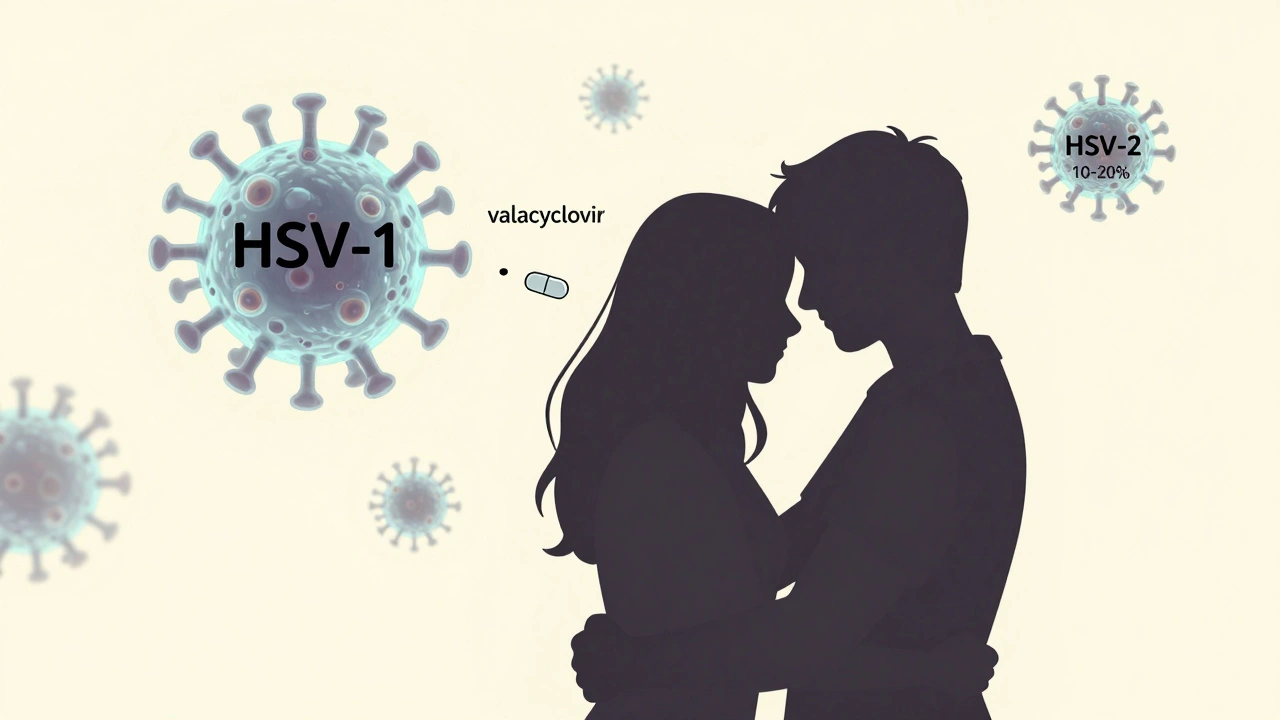
HSV-2 sheds asymptomatically on 10-20% of days. HSV-1 genital shedding happens on 5-10% of days. That’s why transmission happens - often from people who have no idea they’re infectious. Daily suppressive therapy with valacyclovir cuts transmission risk by nearly half. For couples where one partner has HSV-2 and the other doesn’t, daily treatment reduces the chance of spread from about 4% per year to just 2%.
Antiviral Therapy: What Works and When
There are three main antivirals used for HSV: acyclovir, valacyclovir, and famciclovir. All work the same way - they block the virus from copying itself. But they differ in how often you take them and how well they’re absorbed.
For a first genital outbreak, the CDC recommends acyclovir 400mg three times daily for 7-10 days. Valacyclovir 1g twice daily for the same period works just as well and is easier to take. These drugs shorten healing time from 19 days to about 10. Pain drops from 12 days to 8. The sooner you start - within 24 hours of symptoms - the better. Waiting 72 hours cuts the benefit in half.
For frequent recurrences (six or more a year), daily suppressive therapy is the standard. Valacyclovir 500mg once daily reduces outbreaks by 70%. For those with more than 10 outbreaks a year, 1g daily is more effective. Studies show it also reduces asymptomatic shedding by 90%.
For oral herpes, episodic treatment works well. Taking valacyclovir 2g twice daily for one day can stop a cold sore before it fully forms - if you catch it during the tingling stage.
Special Cases: Eyes, Babies, and Immune Problems
HSV-1 is the #1 cause of infectious corneal blindness in the U.S., with about 50,000 new cases of herpes keratitis each year. It’s treated with topical trifluridine drops - one drop every two hours while awake. Healing time drops from 21 days to 14.
Neonatal herpes is rare - 1 in 3,200 births - but deadly. About 70% of cases come from HSV-2, usually from an infected mother during delivery. If untreated, mortality is 60%. With prompt IV acyclovir, it drops to 20%. That’s why doctors now screen pregnant women with active outbreaks near delivery. If there’s a lesion at labor, a C-section is recommended.
Immunocompromised patients - those with HIV, transplants, or cancer - are at high risk for severe or prolonged outbreaks. For them, higher doses are needed. IV acyclovir at 5mg/kg every 8 hours is standard for mucocutaneous infections. For herpes encephalitis, it’s 10mg/kg. About 10% of HSV isolates in HIV patients with CD4 counts below 100 are resistant to acyclovir. That’s when foscarnet or the newer drug pritelivir is used.
Resistance and New Treatments
Antiviral resistance used to be rare. Now, it’s rising. In transplant patients, 15% of HSV strains don’t respond to acyclovir. In advanced HIV, it’s 10%. That’s why newer drugs are being developed. Pritelivir, approved by the FDA in 2023, works differently - it blocks viral helicase, not DNA replication. In trials, it reduced viral shedding by 87% in 48 hours - better than foscarnet. It’s now the go-to for acyclovir-resistant cases.
Therapeutic vaccines are in early trials. GEN-003 and Simplirix showed 50% reduction in viral shedding in phase II studies. But they’re not ready yet. For now, antivirals remain the only proven tool.
Diagnosis: What Tests Actually Tell You
Doctors don’t just guess anymore. PCR testing of a lesion swab is the gold standard - 95-98% accurate. It can tell HSV-1 from HSV-2. Viral culture is older and less sensitive - only 70-80% accurate. Blood tests (serology) detect antibodies. Type-specific gG tests like HerpeSelect or EUROIMMUN’s recomLine can distinguish HSV-1 from HSV-2 with over 96% accuracy. But they’re not useful right after infection. It takes 12-16 weeks for antibodies to show up. So if you just had symptoms, get a PCR. If you’re asymptomatic and want to know your status, get a blood test after 4 months.
Living With HSV: The Emotional Side
It’s not just the physical symptoms. It’s the shame. The fear of telling partners. The anxiety over outbreaks. A 2023 survey by the American Sexual Health Association found 74% of people with HSV feel stigma-related anxiety. Nearly half say it’s hurt their relationships. One in three delayed telling a partner for over six months.
But many find relief. On Drugs.com, 82% of users who took valacyclovir said it reduced outbreak duration. 58% said pain was much less. Side effects? Headache (22%), nausea (15%). A small number report kidney issues - mostly if they already have kidney disease.
One thing most people learn: outbreaks get easier. The first one is brutal. The fifth? Often just a few tiny bumps and a day of discomfort. Daily antivirals make that even better. And knowing you’re not alone helps. Online communities like Reddit’s r/Herpes have over 1.2 million members. People share stories, tips, and support. It’s not a cure - but it’s a lifeline.
What’s Next?
The future of HSV management is clearer than ever. Wider use of suppressive therapy could cut transmission by 30% by 2030. Better diagnostics - like the new EUROIMMUN test replacing the discontinued HerpeSelect - are closing gaps in detection. And with pritelivir now available, resistant cases have a real option.
But the biggest barrier isn’t medicine. It’s silence. People still think herpes means promiscuity. It doesn’t. It means you’re human. It means you’ve been exposed to a virus that lives in nearly 7 out of 10 people worldwide. Treatment works. Transmission can be managed. Life doesn’t stop.
Can HSV-1 cause genital herpes?
Yes. While HSV-1 is best known for cold sores, it now causes 30-50% of new genital herpes cases in high-income countries. This shift happened because more people are engaging in oral-genital contact. HSV-1 genital infections tend to recur less often than HSV-2 - about once a year or less - and shed virus less frequently.
Is there a cure for herpes simplex virus?
No, there is no cure. Once you’re infected, the virus stays in your nerve cells for life. But it doesn’t always cause symptoms. Antiviral medications like acyclovir, valacyclovir, and famciclovir can control outbreaks, reduce transmission, and prevent complications. Many people live decades without noticeable symptoms.
How effective is daily antiviral therapy in preventing transmission?
Daily suppressive therapy with valacyclovir 500mg reduces transmission of HSV-2 to uninfected partners by about 48%. For HSV-1 genital infections, the reduction is similar but less studied. When combined with condom use and avoiding sex during outbreaks, transmission risk drops even further - to under 1% per year in some couples.
Can you get herpes from sharing towels or toilet seats?
It’s extremely unlikely. HSV doesn’t survive long outside the body - usually less than a few hours on dry surfaces. Transmission requires direct skin-to-skin contact with an infected area, especially during active shedding or outbreaks. You can’t catch it from toilet seats, towels, or swimming pools.
Should I get tested for herpes if I don’t have symptoms?
It depends. Routine screening isn’t recommended for people without symptoms. But if you have a partner with HSV, or if you’ve had unprotected sex with multiple partners, a blood test can tell you if you’ve been exposed. Type-specific serologic tests (like EUROIMMUN recomLine) are accurate after 12-16 weeks post-exposure. Knowing your status helps you make informed decisions about protection and disclosure.
What should I do if I think I’m having my first outbreak?
See a healthcare provider within 24 hours of noticing symptoms - tingling, burning, or blisters. Get a PCR test from a swab of the lesion. Start antiviral treatment immediately. Acyclovir or valacyclovir can shorten the outbreak by half and reduce pain. Avoid sexual contact until sores are fully healed. Keep the area clean and dry. Over-the-counter pain relievers and cool compresses help with discomfort.
Can herpes cause encephalitis or blindness?
Yes, but rarely. HSV-1 is responsible for 95% of sporadic herpes encephalitis cases - a serious brain infection that can cause seizures, confusion, and memory loss. It requires urgent IV antiviral treatment. HSV-1 also causes herpes keratitis, the leading infectious cause of corneal blindness in the U.S., with about 50,000 cases yearly. Early treatment with antiviral eye drops can prevent permanent damage.
Are there natural remedies that work for herpes?
No natural remedy has been proven to stop outbreaks or reduce transmission. Lysine supplements, tea tree oil, and zinc creams may soothe symptoms for some, but they don’t affect the virus. Antivirals are the only treatment backed by decades of clinical trials. Relying on unproven methods can delay effective care and increase the risk of complications or spreading the virus.
Can I still have a normal sex life with herpes?
Absolutely. Many people with HSV have long-term, healthy relationships. Using condoms, taking daily antivirals, and avoiding sex during outbreaks reduces transmission risk to less than 1% per year. Open communication with partners is key. Most partners are supportive once they understand the facts. You’re not broken. You’re not dangerous. You’re just someone who carries a common virus - and you have tools to manage it.
How much do antiviral medications cost?
With insurance, valacyclovir 500mg daily costs $35-$60 per month. Without insurance, it can be $300-$400. Generic acyclovir is cheaper - about $10-$20 per month. Many pharmacies offer discount programs. Some clinics provide free or low-cost antivirals for low-income patients. Don’t let cost stop you from getting treatment - ask your doctor about options.



December 3, 2025 AT 07:01
Man, I had my first outbreak last year and thought I was gonna die. Turns out it’s just a pesky roommate in my nerves. Valacyclovir saved my sex life. No shame in taking it daily.