Every year, millions of people in the U.S. stop taking their medication-not because it doesn’t work, but because they don’t understand what they’re taking. A lot of those cases involve generic medications. Patients see a different color, shape, or label and assume it’s a new drug, a weaker version, or even a mistake. They skip doses. They quit altogether. And then they end up in the hospital.
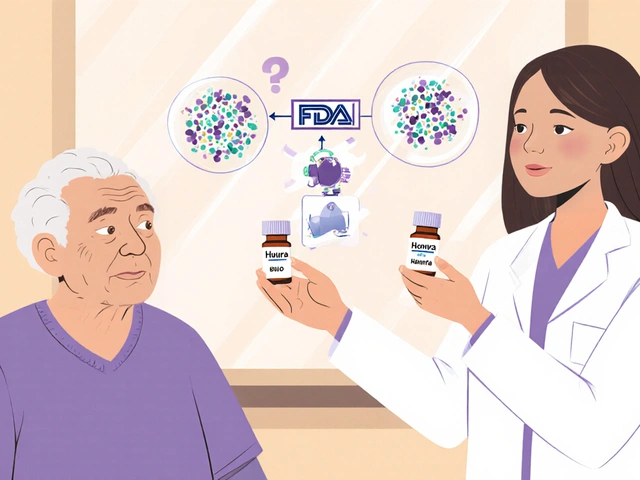
The truth? Generic drugs are not second-rate. They’re the exact same medicine as the brand-name version, down to the active ingredient. The FDA requires them to work the same way, in the same amount of time, with the same safety profile. Yet, 47% of patients with low health literacy don’t believe this. They think generics are inferior. And that belief costs lives-and billions of dollars.
What Health Literacy Really Means (And Why It Matters for Medicines)
Health literacy isn’t just about reading. It’s about understanding what you’re told, asking the right questions, and making decisions based on that information. The Centers for Disease Control and Prevention (CDC) defines it as the ability to find, understand, and use health information to make smart choices. For prescriptions, that means knowing:
- What the pill is for
- How much to take and when
- Why your doctor switched you from a brand-name drug to a generic
- That a different-looking pill can still be the same medicine
Here’s the hard part: only 12% of U.S. adults have proficient health literacy. That means 88% struggle with basic health instructions. For people managing chronic conditions-diabetes, high blood pressure, depression-this gap is deadly.
Why Generics Are the Missing Link
Generics make up 90% of all prescriptions filled in the U.S. But they account for just 23% of total drug spending. Why? Because patients don’t trust them. A Harvard study found that 68% of people worry generics won’t work as well as brand-name drugs. Only 29% have the same concern about brand-name drugs.
That’s not because generics are less effective. It’s because the system never taught them otherwise.
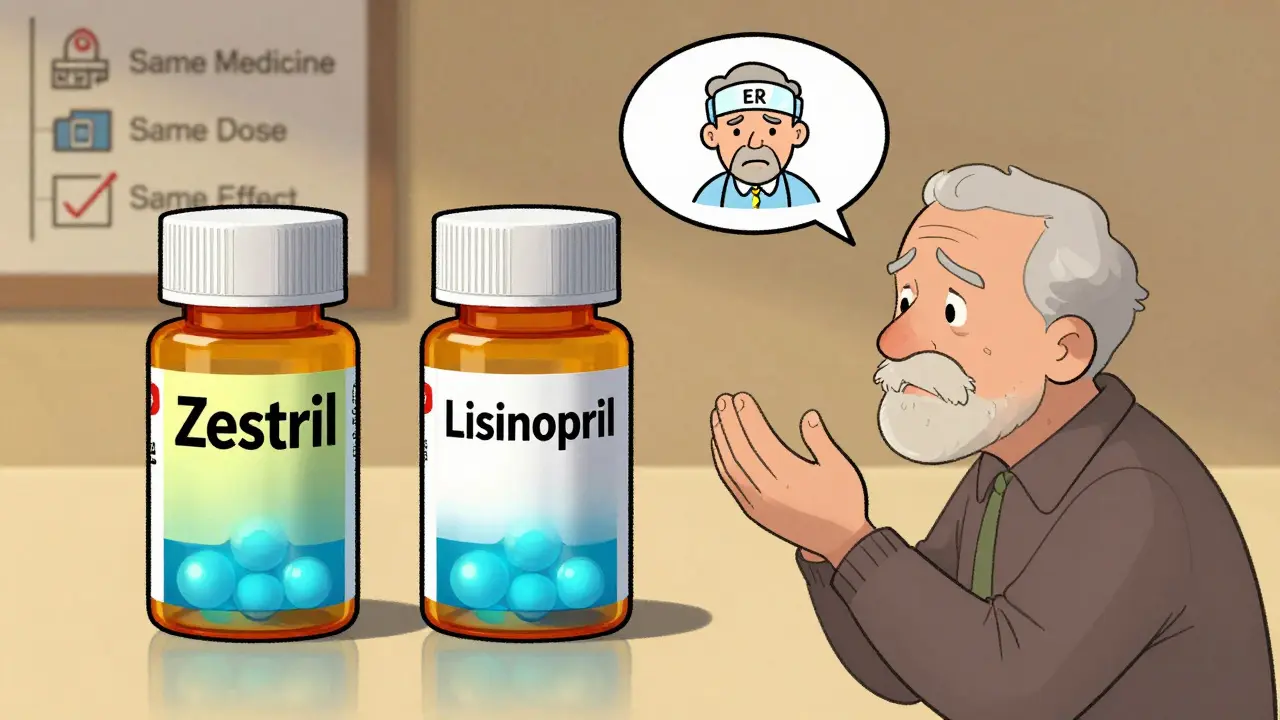
Take blood pressure medication. A patient might have taken Lisinopril 10mg from a blue pill with a brand name for years. Then, their pharmacy switches them to a white oval pill labeled “Lisinopril.” The patient thinks: “This isn’t the same. My doctor wouldn’t give me a weaker drug.” So they stop taking it. Their blood pressure spikes. They end up in the ER. That’s not rare. It’s common.
Studies show that patients with low health literacy are 32% more likely to be hospitalized due to medication errors. And nearly half of those errors involve generics.
The Three Big Knowledge Gaps
There are three core misunderstandings that keep people from using generics-even when it’s the best choice:
- They don’t know generics contain the same active ingredient. The FDA requires generics to match the brand-name drug’s strength, purity, and performance. But labels don’t explain that. They just say “Lisinopril.” No mention of “same as Zestril.”
- They think different looks mean different strength. Pills change color, shape, or size because of inactive ingredients-fillers, dyes, coatings. These don’t affect how the medicine works. But patients don’t know that. One Reddit user stopped their antidepressant because the generic looked “too small.” They thought it was a placebo.
- They don’t understand bioequivalence. The term sounds like jargon. But it’s simple: generics must deliver 80-125% of the same amount of drug into the bloodstream as the brand. That’s the legal standard. It’s not random. It’s science. Yet, 90% of patients have never heard this.
When you combine these gaps with language barriers, low income, or being over 65, the risk multiplies. Immigrants and non-English speakers are 3.2 times more likely to misunderstand generic labels. Elderly patients often juggle multiple prescriptions. A change in pill appearance can trigger confusion, fear, and non-adherence.
What Happens When Patients Don’t Understand
The consequences aren’t theoretical. They’re measurable.
- Patients with low health literacy are 23% less likely to take their meds as prescribed.
- When generics are involved, that number jumps.
- Medication errors tied to generics account for 18% of all hospitalizations related to drug misuse.
- Employers and insurers lose $1.2 billion a year because patients stick with expensive brand-name drugs they don’t understand-or stop taking meds altogether.
One woman in Georgia switched from a brand-name statin to a generic. She didn’t realize it was the same drug. She thought the pharmacy made a mistake. She went back to the brand, paid $300 a month, and kept getting chest pain. Her doctor finally asked: “Did you know the generic was the same?” She cried. “I thought I was being cheated.”
How to Close the Gap
Fixing this isn’t about more pamphlets. It’s about better communication.
Pharmacists are on the front lines. They spend an average of 4.2 minutes explaining generics. But when a patient has low health literacy? That jumps to 9.7 minutes. That’s not efficient. It’s necessary.
The most effective tools are simple:
- The Teach-Back Method: “Tell me in your own words why you’re taking this pill.” If they say, “It’s the same as the blue one,” they get it. If they say, “I think this is weaker,” they need more.
- Visual aids: Side-by-side images of brand and generic pills with labels saying “Same active ingredient.”
- Plain language labels: Replace “Lisinopril” with “This is the same medicine as Zestril. Same dose. Same effect.”
- Digital tools: Apps that let patients scan a pill and see a comparison with the brand name. One study showed a 35% improvement in understanding after using these tools.
Health systems that used these methods saw a 29% drop in medication errors and a 22% increase in adherence within a year.
The Bigger Picture: Cost, Trust, and Equity
Generics save money. A lot of it. But if patients don’t trust them, they won’t use them. That means:
- People pay more out of pocket.
- Insurance companies pay more.
- Hospitals pay more for preventable ER visits.
When patients receive clear, simple information about generics, they’re 83% more likely to stick with their medication. And they’re 14% less likely to visit the ER for medication problems. That’s $675 saved per person each year.
And yet, only 38% of healthcare organizations have any program to teach patients about generics. That’s not just a gap in education. It’s a gap in justice.
Low-income patients, non-English speakers, older adults-they’re not ignoring generics because they’re careless. They’re being failed by a system that assumes they already understand.
What’s Changing Now
In 2023, the FDA launched the Generics Awareness Campaign, training pharmacists and releasing plain-language materials. The CDC added “improving understanding of medication alternatives” to its 2023 Health Literacy Action Plan. Starting in 2024, Medicare Part D plans must assess patients’ health literacy before prescribing.
Pilot programs are already showing results. One hospital integrated a health literacy check into its electronic records. When a patient’s literacy score was low, the system automatically flagged their prescription for extra counseling. Within 18 months, generic-related medication errors dropped by 27%.
This isn’t about making patients smarter. It’s about making the system clearer.
What You Can Do
If you take medication-especially generics:
- Ask your pharmacist: “Is this the same as the brand name?”
- Ask: “What’s the active ingredient?” (It’s the same in both.)
- Use a pill identifier app if you’re confused by the shape or color.
- Don’t assume a change means a problem. Ask first.
If you’re a caregiver, provider, or family member:
- Use plain language. No jargon.
- Use the Teach-Back method. Have them explain it back.
- Keep a list of all medications with brand and generic names side by side.
Knowledge gaps don’t close themselves. They need action. And they need to be addressed-every time a prescription is filled.




February 9, 2026 AT 14:57
I can't believe this is even a debate. I mean, seriously? People think generics are 'weaker'?? Like, have you seen the FDA's guidelines?? I looked up the bioequivalence standards last week because I was paranoid after my pharmacist switched my antidepressant from the blue pill to a tiny white one. Turns out? It's literally the same molecule. Same absorption rate. Same half-life. The only difference? The filler is cornstarch instead of lactose. And the color? Dye. That's it. I cried. Not because I was scared-but because I realized I'd been paying $300/month for NOTHING. The system is rigged. And no one tells you this. Why? Because Big Pharma doesn't want you to know you're being scammed. #WakeUp