Every time you pick up a new prescription, you’re holding a safety checklist. The small print on that label isn’t just bureaucracy-it’s your first line of defense against dangerous mistakes. Prescriber verification isn’t optional. It’s a habit that can stop a wrong drug, a wrong dose, or even a wrong person’s prescription from ending up in your hands.
What You Need to Check on Every Label
When you get your medication, don’t just grab it and go. Spend 60 seconds. Seriously. The FDA recommends it. So do pharmacists. Here’s what to look for, in order:
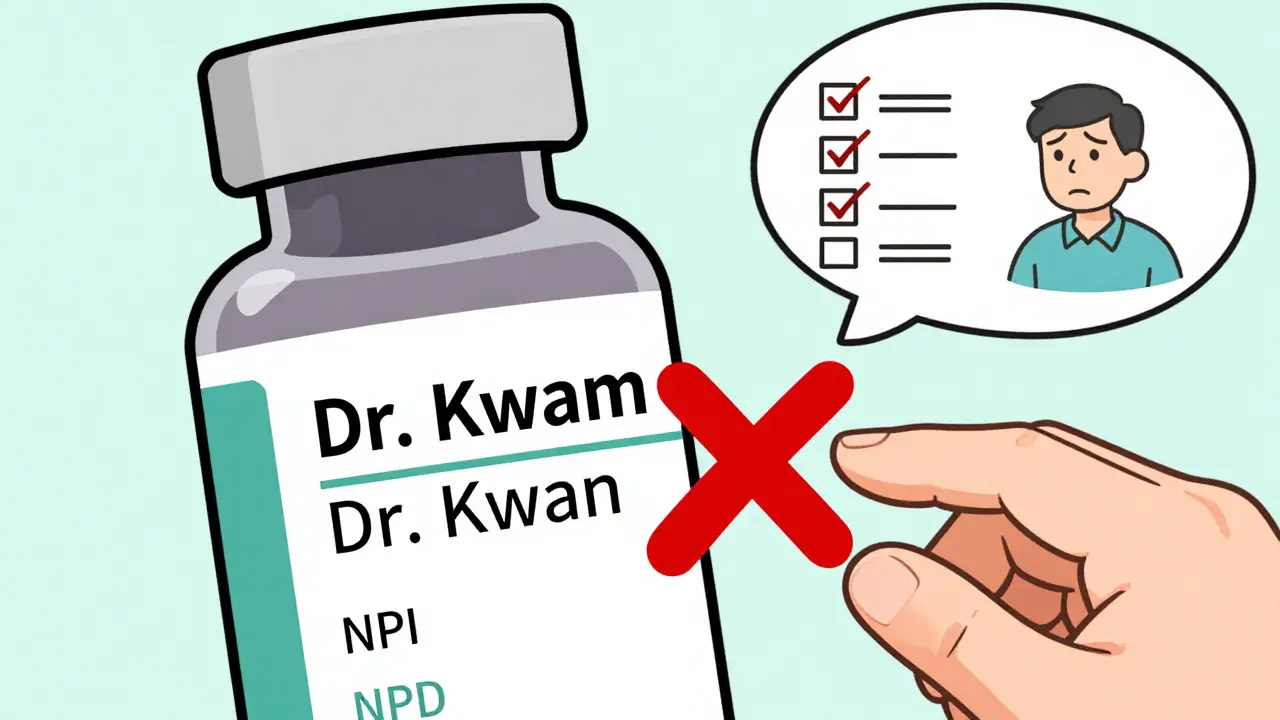
- Prescriber’s full name - This should match exactly who you saw. Not “Dr. J. Smith” if your doctor is “Dr. Jennifer Smith.” Misspellings happen, especially with electronic prescriptions.
- National Provider Identifier (NPI) number - It’s a 10-digit number, usually printed near the prescriber’s name. It’s unique to each healthcare provider. If you’re unsure, call the pharmacy and ask them to confirm the NPI matches your provider’s.
- Prescription number - This is the key to refills. Write it down or save it in your phone. If you call for a refill and they can’t find it, that’s a red flag.
- Pharmacy name and address - Make sure it’s the pharmacy you expect. Did you pick it up at CVS? Then the label should say CVS Pharmacy, not Walgreens or a mail-order service you didn’t order from.
- Pharmacy phone number - This is your lifeline. If something looks off, call this number. Don’t rely on the prescriber’s office. Pharmacists are trained to catch errors.
- Pharmacist’s name - In 42 states, this is required by law. Seeing a name you recognize builds trust. If it’s blank or looks typed in, ask why.
These aren’t suggestions. They’re federal and state requirements. The FDA’s 2023 labeling rules (MAPP 5240.3) and the Medicare Prescription Drug Act of 2003 make this information mandatory. If it’s missing, the pharmacy is out of compliance.
Why This Matters More Than You Think
Medication errors aren’t rare. The FDA says over 1.3 million people are injured every year because of them. About 12% of those errors come from misidentified prescribers or pharmacies. That’s not a glitch. That’s preventable.
One real case from a May 2023 FDA safety alert: a patient received a Schedule II opioid prescribed by a dentist, but the label listed their primary care doctor. The patient didn’t question it-until they started feeling dizzy and confused. Turns out, the pharmacy mixed up two similar-looking electronic prescriptions. The dentist had prescribed oxycodone for tooth pain. The primary care doctor had prescribed a muscle relaxer. The wrong one was filled. The patient could have overdosed.
Another example: a woman in Ohio noticed the prescriber name on her blood thinner didn’t match her cardiologist. She called the pharmacy. They admitted they’d accidentally filled a prescription meant for another patient with the same last name. She was 78. Her cardiologist had just changed her dose. The label had the old dose. She caught it before taking the first pill.
These aren’t outliers. Reddit’s r/pharmacy community had over 1,200 comments in March 2024 from people who caught errors by checking their labels. The top two mistakes? Misspelled prescriber names (42%) and wrong specialty (28%). Like a dermatologist prescribing insulin. Or a chiropractor writing a psychiatric med. Both happened.
Where Errors Happen-and How to Avoid Them
Not all pharmacies are the same. A 2023 NABP audit found community pharmacies like CVS and Walgreens had 98.7% accuracy on prescriber info. Mail-order pharmacies? 96.4%. That gap might seem small, but in a system that fills millions of prescriptions a day, it’s thousands of mistakes.
Electronic prescriptions are the biggest source of errors. When doctors use templates or auto-fill systems, names and NPIs can copy over incorrectly. A 2023 AHRQ report found 18% of verification failures came from e-prescribing glitches. Specialty pharmacies-those handling cancer drugs, rare diseases, or injectables-have a 23% higher error rate than your local pharmacy.
Here’s how to fight back:
- Use a magnifying glass - 37% of people over 65 struggle with small print. Most pharmacies give out free magnifiers. Ask for one.
- Ask the pharmacist to spell the prescriber’s name - If it’s “Dr. Kwan” but looks like “Dr. Kwam,” ask. It’s your right.
- Keep a personal medication record - Write down every drug you take, the prescriber’s name, and the pharmacy. 73% of major chains now offer free digital versions through their apps. Use them.
- Don’t assume - Even if the label looks right, double-check. Dr. Michael Chen from the AMA warns that 14% of accurate-looking labels still have hidden errors patients can’t spot. That’s why you need to talk to your pharmacist.
When to Verify-Three Critical Moments
You shouldn’t check your label just once. Do it at three points:
- When you first get the prescription - This is your baseline. Compare it to what your doctor told you.
- Before you take your first dose - Especially if it’s a new drug. Read the name, the dose, the instructions. If it doesn’t match what you were told, don’t take it.
- When you refill - This is where mistakes slip through. A refill might go to a different pharmacy. Or the system might auto-renew an old prescription. Always check.
Patients who verify at all three points report 27% fewer errors and 31% better adherence, according to PatientPoint’s 2023 survey. That’s not a coincidence. It’s proof that attention saves lives.
What to Do If Something’s Wrong
If the label doesn’t match what you expect, don’t just walk away. Don’t take the medicine. Don’t assume it’s a “typo.”
Call the pharmacy. Use the number on the label. Say: “I’m reviewing my prescription label and noticed the prescriber name doesn’t match my doctor. Can you confirm this is correct?”
If they say, “It’s fine,” ask for the NPI number. Then call your doctor’s office and verify it. Most offices can confirm in under a minute.
If the pharmacy refuses to fix it, file a complaint. Every state has a pharmacy board. You can find yours at nabp.pharmacy. Also report it to the FDA’s MedWatch program. These reports help track patterns and force fixes.
And if you’re ever unsure? Ask for the pharmacist to call your doctor. That’s their job. They’re trained to resolve these issues. You’re not being difficult. You’re being smart.

The Future of Label Verification
Technology is coming. The FDA just started a pilot program with QR codes on labels that link to digital verification tools. Early results show a 19% improvement in accuracy. That’s promising.
But don’t count on apps or QR codes to replace your eyes. A 2023 study in the Journal of the American Pharmacists Association found physical label checks had only a 2.1% error rate. Mobile apps? 7.2%. Why? Because apps can glitch. Screens can be misread. You can’t tap your way out of a wrong name.
For now, the best tool is still you-your eyes, your questions, your willingness to pause and check. The FDA’s 2024-2027 plan wants 75% of U.S. adults verifying their labels by 2027. Right now, it’s 62%. You can help push that number higher.
Final Checklist: Your 60-Second Safety Routine
Before you leave the pharmacy-or before you open that pill bottle-run through this:
- ✅ Prescriber name matches who you saw?
- ✅ NPI number is present and correct?
- ✅ Prescription number matches your records?
- ✅ Pharmacy name and phone number are right?
- ✅ Pharmacist’s name is listed (if required in your state)?
- ✅ Dose and instructions match what your doctor said?
If all five are checked? You’re safe. If one’s off? Stop. Call. Confirm. Don’t take the pill until you know it’s yours.
What if the prescriber name on my label is misspelled?
A misspelled name is a red flag. It could mean the prescription was meant for someone else, or the e-prescribing system auto-filled incorrectly. Don’t ignore it. Call the pharmacy immediately and ask them to confirm the correct prescriber and NPI number. If they can’t fix it, contact your doctor’s office directly. This is not a minor error-it’s a safety issue.
Can I trust the pharmacy’s mobile app instead of the physical label?
No. While apps are helpful for tracking refills and reminders, they’re not as reliable as the physical label. A 2023 study showed mobile apps had a 7.2% error rate in displaying prescriber info, compared to just 2.1% for physical labels. Apps can glitch, sync incorrectly, or show outdated data. Always verify against the printed label before taking any medication.
Why does the pharmacy need to list the pharmacist’s name?
In 42 U.S. states, it’s required by law. The pharmacist’s name holds them accountable. If you have a question or concern, you can ask to speak to that person. It also helps build trust-if you see a familiar name, you know the same professional reviewed your prescription. If the name is missing, ask why. It’s your right to know.
What should I do if I get the wrong prescription from a mail-order pharmacy?
Stop taking the medication immediately. Call the pharmacy using the number on the label and report the error. Then call your doctor to confirm the correct prescription. File a report with the FDA’s MedWatch program and your state pharmacy board. Mail-order pharmacies have higher error rates than local ones, so verification is even more critical. Keep a record of the error for future reference.
Is it normal for my prescription to be filled by a different pharmacy than I usually use?
It can happen, especially with insurance plans that use mail-order services or preferred networks. But you should always be notified in advance. If you didn’t authorize the switch, check the label carefully. Make sure the prescriber name, dosage, and pharmacy details are correct. If anything seems off, call your doctor and your usual pharmacy to confirm. Never assume a change is safe just because it’s automatic.






January 23, 2026 AT 05:55
It’s funny how we’re told to check labels like they’re ancient scrolls. But if you’ve ever waited 45 minutes at CVS just to ask if ‘Dr. Kwan’ is really ‘Dr. Kwam,’ you know the system’s broken. We’re not supposed to be detectives. We’re supposed to be patients.