Managing pain after giving birth doesn’t mean you have to choose between feeling better and keeping your baby safe. Many new mothers worry that taking pain meds while breastfeeding could harm their baby. The truth? Most common pain relievers are perfectly safe - if you know which ones to use and when. The outdated idea of "pump and dump" after every dose or surgery is no longer supported by science. You don’t need to throw away your milk or stop nursing to manage pain. But some medications are dangerous - and using them can put your baby at risk.
What Pain Medications Are Safe While Breastfeeding?
The safest choices for postpartum pain are ibuprofen and acetaminophen. Both are recommended as first-line options by the American College of Obstetricians and Gynecologists (ACOG), the Academy of Breastfeeding Medicine, and the InfantRisk Center. These medications pass into breast milk in tiny amounts - less than 1% of your dose - and have been studied in thousands of nursing mothers over decades.
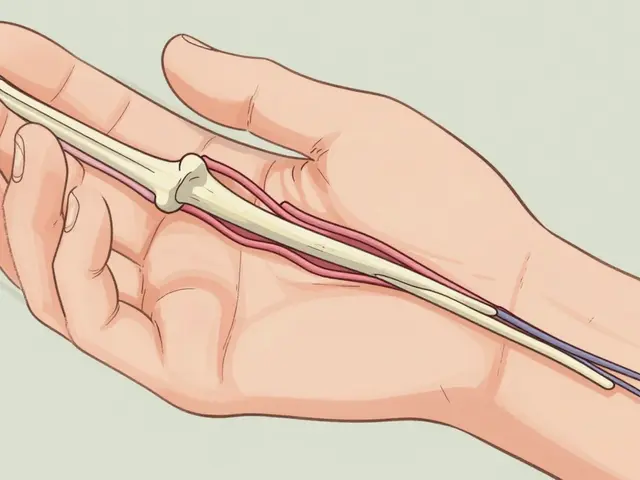
Ibuprofen transfers at about 0.6-0.7% of your dose, peaking in milk 1-2 hours after you take it. Acetaminophen is even lower, at 0.1-1.0%. Neither affects your baby’s digestion, sleep, or breathing. You can take them on a regular schedule without worrying about timing feeds. Many hospitals now give new moms scheduled doses of both every 6-8 hours after a C-section, with no need to pause breastfeeding.
For example, Michigan OPEN’s 2022 protocol suggests replacing the first three oral NSAID doses after a C-section with a short IV dose of Toradol (ketorolac), which also has minimal transfer into milk. This keeps pain under control without overloading your system or your baby’s.
Which Pain Medications Should You Avoid?
Not all pain meds are created equal. Two opioids - codeine and tramadol - are strongly discouraged for breastfeeding mothers. The FDA issued warnings in 2017 and 2018 after multiple infant deaths linked to these drugs. The problem isn’t the dose - it’s your body’s genetics.
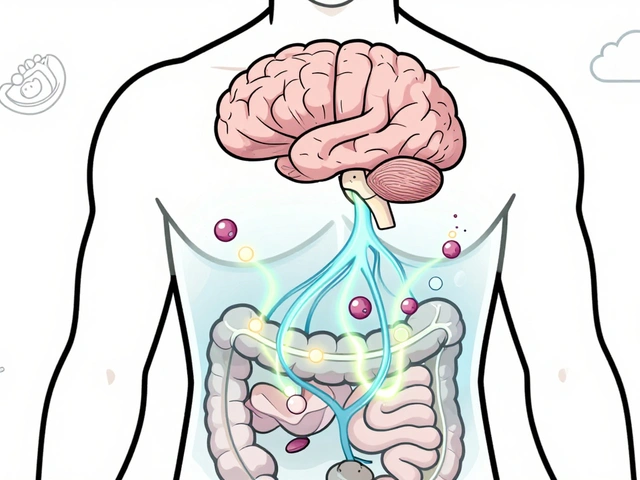
About 1 in 100 Caucasian women are "ultra-rapid metabolizers" of codeine. Their bodies convert it into morphine much faster than normal. That means your breast milk could contain up to 20 times more morphine than expected. Even a single dose can cause your baby to become dangerously sleepy, have trouble latching, or stop breathing. Tramadol works the same way - it turns into an active metabolite (M1) that can build up in your baby’s system. There’s no way to test for this before you take the drug, and the symptoms in babies can be subtle at first.
Other opioids like oxycodone, hydrocodone, and hydromorphone are considered "moderately safe" - but only if used carefully. They transfer into milk at low levels (0.1-0.5%), but they can still make babies drowsy. Morphine is the safest opioid option because babies absorb less than 1% of what’s in your milk. Its poor oral bioavailability means most of it passes right through without being absorbed.
How to Time Your Doses for Maximum Safety
If you need an opioid for breakthrough pain - say, after a difficult delivery or C-section - timing matters. Don’t take it right before nursing. Instead, take it right after a feeding. This gives your body time to process the drug before the next feed.
Peak levels of most opioids in breast milk happen 1-2 hours after you take them. Waiting 3-4 hours before the next feed reduces your baby’s exposure. Intermountain Health’s 2022 guidelines suggest using opioids for no longer than 4-6 days total. After that, switch back to ibuprofen and acetaminophen.
For example: if you take oxycodone at 8 p.m. after nursing, the next feed can be at 1 a.m. - giving you 5 hours between dose and feed. That’s plenty of time for the drug to drop in concentration.
Watch for Signs Your Baby Is Affected
Even with safe medications, keep an eye on your baby. Signs of opioid sedation include:
- Excessive sleepiness - hard to wake for feeds
- Difficulty latching or sucking
- Shallow or irregular breathing
- Constipation or reduced stooling
- Unusual floppiness or limpness
These signs can appear within hours - or be delayed up to 24 hours after a dose. If you notice any of these, stop the medication and call your pediatrician immediately. Don’t wait. Babies under 2 months are especially vulnerable because their livers and kidneys aren’t fully developed yet.
What About Naproxen or Other NSAIDs?
Naproxen and indomethacin are NSAIDs like ibuprofen, but they stay in your system longer. Naproxen reaches 1.5-2.0% of your dose in breast milk after 24 hours, which is higher than ibuprofen’s 0.6%. While occasional use may be okay, these aren’t recommended for daily pain control while breastfeeding, especially with newborns or preemies. Stick with ibuprofen - it clears faster and has better safety data.
Can You Use Natural Remedies Alongside Medications?
Yes - but don’t assume "natural" means safe. Some herbal teas, essential oils, or supplements can interfere with medications or affect milk supply. Turmeric, ginger, and cold packs are fine for mild discomfort. Acupuncture and massage can help with back and pelvic pain. But avoid unregulated supplements like CBD or high-dose vitamins without checking with your provider.
The best natural support? Rest, hydration, and help with baby care. Pain often feels worse when you’re exhausted. Ask for help with feedings, diaper changes, or household tasks so you can recover.

What If You’ve Already Taken a Risky Medication?
If you accidentally took codeine or tramadol once, don’t panic. A single dose is unlikely to cause harm if your baby is healthy and full-term. But watch them closely for the next 24 hours. If they seem unusually sleepy, have trouble feeding, or their breathing seems shallow, go to the emergency room. Don’t wait.
If you’ve been taking these drugs regularly, talk to your doctor about switching immediately. You can still breastfeed safely with other options - you just need to change your plan.
What’s Changing in 2026?
Medical guidelines keep improving. In 2023, Mayo Clinic researchers published a study showing that genetic testing for CYP2D6 metabolism could identify ultra-rapid metabolizers before prescribing codeine. This test isn’t routine yet, but it’s coming. Hospitals in some regions are already starting to screen high-risk patients.
Meanwhile, the LactMed database - maintained by the National Library of Medicine - continues to update its evidence-based ratings for over 15 postpartum pain meds. It’s now the go-to resource for clinicians and mothers alike.
The big shift? We’ve moved from fear to facts. Breastfeeding while taking pain meds isn’t risky - if you know which ones to use. The goal isn’t to avoid all meds. It’s to use the right ones, the right way, and know when to call for help.
Is it safe to take ibuprofen while breastfeeding?
Yes, ibuprofen is one of the safest pain medications for breastfeeding mothers. Only about 0.6-0.7% of your dose passes into breast milk, and it doesn’t affect your baby’s sleep, digestion, or breathing. It’s recommended as a first-line option by ACOG and the Academy of Breastfeeding Medicine. You can take it on a regular schedule without needing to time feeds.
Can I take acetaminophen while breastfeeding?
Yes, acetaminophen is safe and commonly used after childbirth. It transfers into breast milk at very low levels - 0.1-1.0% of your dose - and has no known harmful effects on nursing infants. It’s often combined with ibuprofen for better pain control. Both can be taken together every 3-4 hours if needed.
Why is codeine dangerous while breastfeeding?
Codeine is converted into morphine in your body. Some women are "ultra-rapid metabolizers" - meaning they turn codeine into morphine much faster than others. This can cause dangerously high levels of morphine in breast milk, even with normal doses. Infants exposed to this can become extremely sleepy, have trouble breathing, or even stop breathing. The FDA warns that breastfeeding is not recommended while taking codeine because you can’t predict who will have this reaction.
Is tramadol safe for breastfeeding mothers?
No, tramadol is not safe for breastfeeding mothers. Like codeine, it’s metabolized into an active compound (M1) that can build up in your baby’s system. The FDA has issued multiple safety warnings since 2018 after infants developed life-threatening respiratory depression from tramadol exposure through breast milk. Even standard doses have caused serious harm. Avoid it completely while nursing.
What should I do if my baby seems too sleepy after I take pain meds?
If your baby is unusually sleepy, has trouble latching, or their breathing seems shallow or irregular, stop the medication immediately and contact your pediatrician or go to the ER. These signs can appear within hours - or be delayed up to 24 hours. Don’t wait to see if it gets better. Early intervention can prevent serious complications.
Can I use opioids like oxycodone while breastfeeding?
Oxycodone can be used short-term for breakthrough pain, but only under medical supervision. It transfers into milk at low levels (0.1-0.5%), but it can still cause drowsiness in babies. Take it right after a feeding, wait 3-4 hours before the next one, and limit use to 4-6 days. Morphine is preferred over oxycodone because babies absorb less of it. Never use oxycodone without talking to your doctor first.
Should I pump and dump after taking pain medication?
No, you do not need to pump and dump after taking ibuprofen, acetaminophen, or even most opioids when used correctly. The idea that you must discard milk after anesthesia or pain meds is outdated. Studies show the amount of medication in breast milk is too low to harm your baby. Pumping and dumping doesn’t make you safer - it just reduces your milk supply and adds unnecessary stress. Focus on choosing the right meds and timing doses instead.
What’s the best pain management plan after a C-section?
Start with scheduled doses of ibuprofen and acetaminophen every 6-8 hours. If you need more, add a short-acting opioid like morphine or oxycodone only for breakthrough pain. Avoid codeine and tramadol entirely. The Michigan OPEN protocol suggests replacing the first three oral NSAID doses with IV Toradol if available. Use opioids for no more than 4-6 days. Always take opioids after a feeding, not before. Keep your baby monitored for drowsiness or feeding issues.
Next Steps: What to Do Today
If you’re already taking pain meds, check the label. If it’s codeine or tramadol, call your doctor today. Ask for a safer alternative - ibuprofen, acetaminophen, or morphine if needed.
If you’re planning for delivery, talk to your OB or anesthesiologist before labor. Ask: "What pain medications will you give me after birth, and which ones are safe for breastfeeding?" Don’t wait until you’re in recovery to find out.
Keep a list of safe and unsafe meds handy. Print the LactMed summary or save it on your phone. Share it with your partner or support person so they can help you make safe choices when you’re tired or in pain.
Remember: You don’t have to suffer. And you don’t have to choose between being a good mom and being pain-free. With the right information, you can do both.





January 5, 2026 AT 09:16
Just took my first ibuprofen after my C-section and didn’t pump and dump. Felt like a rebel. My baby slept through the night for the first time. Turns out science actually works.