Choosing the right insulin for diabetes isn’t about picking the most advanced or expensive option-it’s about matching your life, habits, and health goals to a treatment that works consistently without putting you at risk. Millions of people with diabetes rely on insulin daily, but many struggle because their regimen doesn’t fit their real-world routine. The goal isn’t just to lower blood sugar-it’s to do it safely, simply, and sustainably.
Understanding How Insulin Works in Your Body
Your pancreas normally releases insulin in two ways: a steady, low trickle (basal) to manage blood sugar between meals and overnight, and a quick burst (bolus) after eating to handle the sugar from food. Insulin therapy tries to copy this pattern. Without it, blood sugar climbs dangerously high, damaging nerves, kidneys, eyes, and blood vessels over time. The Diabetes Control and Complications Trial showed that keeping A1C below 7% cuts microvascular complications by up to 40%. That’s not a small win-it’s life-changing.
Insulin doesn’t work the same for everyone. Some people need fast-acting doses before every meal. Others do better with one long-acting shot a day. Your age, activity level, eating habits, and risk of low blood sugar all matter. There’s no one-size-fits-all, but there are clear categories based on how quickly they start, when they peak, and how long they last.
The Four Main Types of Insulin
Insulin is grouped by its action profile. Knowing these helps you understand why your doctor might recommend one over another.
- Rapid-acting (e.g., Humalog, NovoLog, Apidra): Starts in 10-15 minutes, peaks in 30-90 minutes, lasts 3-5 hours. Used for meals. Best for people who eat at regular times or want flexibility.
- Short-acting (e.g., Humulin R, Novolin R): Starts in 30 minutes, peaks at 2-3 hours, lasts 5-8 hours. Older, cheaper option. Still used in hospitals or when cost is a major concern.
- Intermediate-acting (e.g., NPH): Starts in 1-2 hours, peaks at 4-12 hours, lasts 12-18 hours. Often used once or twice daily. Higher risk of nighttime lows compared to newer options.
- Long-acting (e.g., Lantus, Levemir, Toujeo): Starts in 1-2 hours, no real peak, lasts 18-36 hours. Designed to mimic basal insulin. Preferred for steady background coverage.
- Ultra-long-acting (e.g., Tresiba): Starts in 6 hours, no peak, lasts over 42 hours. Offers the most stable coverage, with 40% lower risk of severe low blood sugar than older long-acting insulins.
Inhaled insulin (Afrezza) is also available. It works like rapid-acting insulin but is breathed in instead of injected. It’s fast-starts in 12 minutes-but isn’t for smokers or people with lung problems. It’s also expensive and hard to get through insurance.
Common Insulin Regimens: How They Fit Your Life
Regimens are the combinations of insulin types you use each day. The right one depends on your type of diabetes, lifestyle, and willingness to manage multiple injections or devices.
Basal-Bolus (Multiple Daily Injections or MDI)
This is the gold standard for type 1 diabetes and many with advanced type 2. You take one long-acting insulin once or twice daily for background coverage, plus rapid-acting insulin before each meal. It gives you the most control. You can adjust meal doses based on what you eat, your blood sugar, and activity. But it requires more effort: carb counting, frequent testing, and dose adjustments.
People who do well with this regimen often use continuous glucose monitors (CGMs) and smart insulin pens. Studies show MDI users who track their numbers closely can hit A1C targets with fewer lows than those on older regimens.
Basal-Only
Some people with type 2 diabetes start with just a long-acting insulin once a day. It’s simple. You don’t need to count carbs or inject multiple times. But it’s not enough if your blood sugar spikes badly after meals. Many end up adding mealtime insulin later. This approach is common when someone’s A1C is high (over 9%) but they’re not ready for complex regimens.
Premixed Insulin
These are blends, like 75% NPH and 25% regular insulin (Humalog Mix 75/25). You take them twice a day, before breakfast and dinner. They’re convenient-no need to mix different insulins. But they’re inflexible. If you skip a meal or eat more carbs than usual, your blood sugar goes off track. They’re often used in older adults or those who struggle with multiple daily injections.
Insulin Pumps
Pumps deliver rapid-acting insulin continuously through a tiny tube under the skin. You can adjust the flow rate (basal) and give extra doses (bolus) with a button. They’re great for people who want precision and flexibility. The DIAMOND trial found 78% of pump users with type 1 diabetes achieved A1C under 7%. But pumps require daily maintenance, and 62% of users report issues like site infections or dislodged catheters.
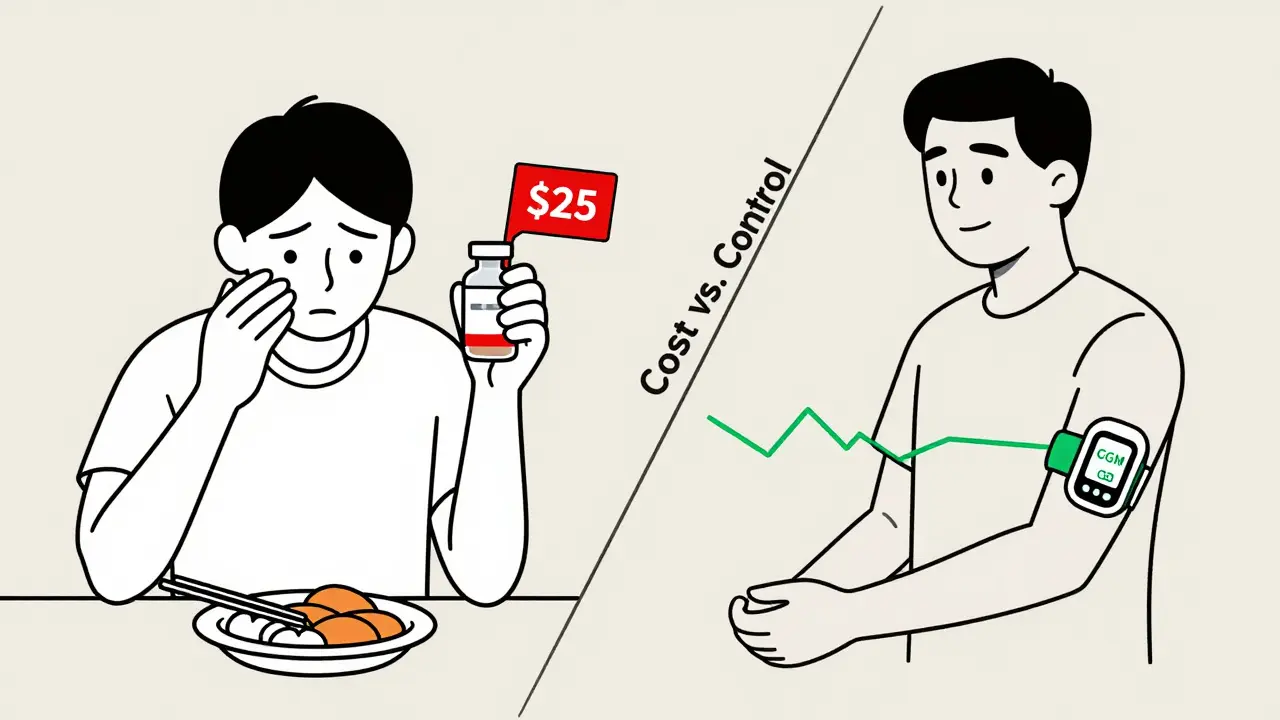
Cost and Access: The Real Barrier
Insulin isn’t just about science-it’s about affordability. Human insulin (like Humulin R) costs $25-$35 at Walmart or ReliOn. Analog insulins? $250-$350 per vial without insurance. That’s why 1 in 4 insulin users still ration their doses, even after the $35 monthly cap for Medicare in 2023. The Inflation Reduction Act expanded that cap to commercial insurance in 2025, which should help millions. But many people still can’t afford CGMs, test strips, or smart pens.
Biosimilars like Semglee (a copy of Lantus) are now available and cost about half as much. They’re just as safe and effective. Ask your doctor if you’re eligible. Switching from a brand-name analog to a biosimilar can save you $200+ per month.
When to Choose Analog Over Human Insulin
Human insulins work. But analogs are better for most people. Why?
- Rapid-acting analogs cause 25% fewer low blood sugar events than regular insulin.
- Long-acting analogs like glargine and degludec reduce nighttime lows by up to 50% compared to NPH.
- Ultra-long-acting degludec cuts severe hypoglycemia risk by 40% over glargine.
That’s not just a statistic-it’s a safety win. If you’ve had a scary low blood sugar episode, or you’re afraid of nighttime lows, analogs are worth the extra cost. For many, the improved quality of life justifies the price. But if you’re on a tight budget and can manage your meals and timing well, human insulin is still a valid, safe option.
What Experts Say About Starting Insulin
Doctors now recommend a different approach for type 2 diabetes than they did 10 years ago. Before insulin, try these first:
- GLP-1 receptor agonists (like semaglutide): Lower A1C, cause weight loss (4-6 kg on average), and protect your heart and kidneys. Often used before insulin in people with heart disease.
- SGLT2 inhibitors (like empagliflozin): Also protect the heart and kidneys, help with weight, but can cause genital infections or rare ketoacidosis.
Insulin is no longer the last resort-it’s a tool. But it’s not always the first. If your A1C is over 9.5%, or you’re losing weight, or you have symptoms like extreme thirst and fatigue, insulin should start sooner. Delaying it can lead to irreversible damage.
For type 1 diabetes, insulin is non-negotiable. You must take it. The question is: how? MDI or pump? Studies show pumps give a 0.5-1.0% better A1C reduction for motivated users. But if you hate needles or can’t handle the tech, MDI with a CGM works just as well.
Practical Tips to Make Insulin Work for You
- Start low, go slow. Basal insulin usually begins at 0.2-0.4 units per kg of body weight. Bolus doses start at 4-6 units per meal. Adjust based on your blood sugar trends-not one reading.
- Use a correction factor. Most people need 1 unit of insulin to lower blood sugar by 30-50 mg/dL. Test this yourself: take 1 unit when your sugar is 200, wait 3 hours, see how much it drops.
- Track your carbs. Learn how many grams of carbs you need 1 unit of insulin for. Most people need 1 unit per 10-15g carbs, but it varies. A certified diabetes educator can help you find your ratio.
- Don’t skip meals. If you’re on rapid-acting insulin, eating less than planned can cause low blood sugar. Always have fast-acting carbs on hand.
- Use a CGM. If you’re on insulin, you should be using a continuous glucose monitor. It shows trends, alerts you to lows, and helps you spot patterns you’d miss with fingersticks.
Many people take 6-12 weeks to feel comfortable with insulin. Structured education programs like DAFNE cut that learning curve by 40%. Ask your clinic if they offer diabetes self-management training. It’s covered by most insurance.
What’s Coming Next
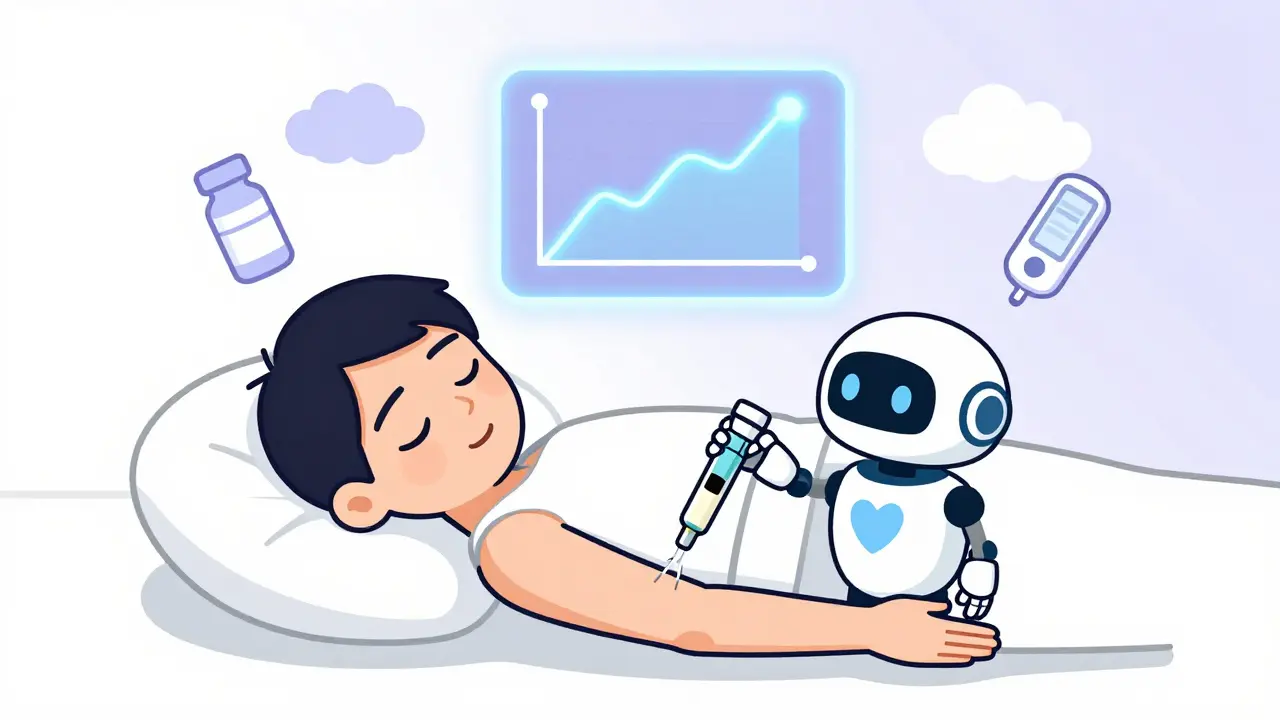
Insulin therapy is evolving fast. In 2024, the FDA approved the first once-weekly insulin (icodec). Early data shows it’s as effective as daily degludec, with slightly better A1C results. No more daily shots. That’s huge for adherence.
Oral insulin is in phase 3 trials. Oramed’s ORMD-0801 reduced A1C by 0.8% in studies. If approved, it could change everything-no needles, no injections. Still years away, but it’s real.
Smart insulin pens and closed-loop systems (artificial pancreas) are growing fast. By 2030, nearly half of type 1 patients may use automated systems. These devices adjust insulin automatically based on your CGM data. They’re not perfect, but they reduce the mental load significantly.
The biggest challenge isn’t technology-it’s access. Even with new options, 1 in 4 people still ration insulin. Until prices drop across the board, even the best regimen won’t help if you can’t afford it.
Final Thoughts: Your Regimen, Your Life
There’s no perfect insulin. Only the one that fits your life. If you’re busy, travel often, or eat at odd hours, rapid-acting insulin with a pump or CGM might be your best bet. If you’re older, have memory issues, or are on a fixed income, a simple basal-only or premixed regimen might be safer and more sustainable.
Don’t let fear of needles or complexity stop you. Insulin isn’t a failure-it’s a tool to live longer, healthier, and freer. Work with your care team. Ask about biosimilars. Use your insurance benefits for education. And remember: your goal isn’t perfection. It’s consistency. One good day at a time.





December 24, 2025 AT 22:14
Man, I wish I'd known all this when I first started insulin. I was terrified of needles and thought I was failing because I needed it. Turns out it's just a tool-like glasses for your pancreas. Started with basal-only, then added bolus after a scary low. Now I use a CGM and a smart pen. Life's way better. No more guessing. Just data. And yeah, biosimilars saved me $200/month. Talk to your doc. Seriously.