Trimethoprim Hyperkalemia Risk Calculator
This calculator assesses your risk of developing hyperkalemia when taking trimethoprim. Based on FDA guidelines and clinical studies, your risk increases significantly when you have multiple risk factors.
When you take an antibiotic like Bactrim or Septra for a urinary tract infection, you probably don’t think about your potassium levels. But that’s exactly what you should be doing. Trimethoprim, one of the two active ingredients in these widely prescribed drugs, doesn’t just kill bacteria-it can quietly disrupt your body’s ability to get rid of potassium. And when potassium builds up, it can lead to something dangerous: hyperkalemia.
What Is Hyperkalemia and Why Does It Matter?
Hyperkalemia means your blood potassium level is too high. Normal levels sit between 3.5 and 5.0 mmol/L. When it climbs above 5.5 mmol/L, your heart’s rhythm can start to wobble. Above 6.5 mmol/L, you’re at risk of cardiac arrest. It doesn’t always cause symptoms until it’s too late. Some people feel nothing. Others get muscle weakness, nausea, or an irregular heartbeat. In older adults, it can strike suddenly-no warning, no pain-just a silent, deadly spike.What makes this even scarier is that trimethoprim doesn’t need to be given in high doses to cause this. Even a single daily tablet of 160/800 mg (the standard dose for UTIs) has been linked to potassium levels shooting up to 7.8 mmol/L in healthy-looking elderly patients. One case report described an 80-year-old woman who had cardiac arrest just three days after starting prophylactic Bactrim. Her kidney function was normal. Her creatinine was fine. But her potassium? It was through the roof.
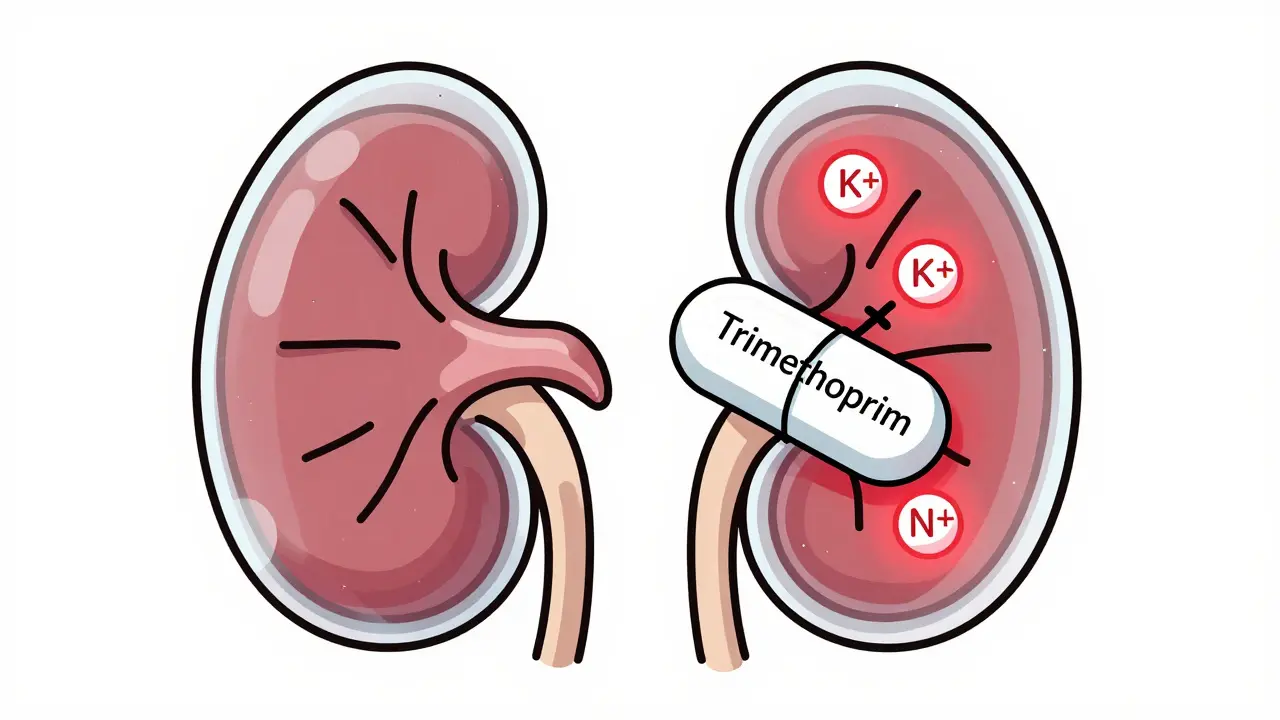
How Trimethoprim Messes With Your Kidneys
Trimethoprim isn’t just an antibiotic. It’s also a sneaky mimic of a drug called amiloride-a potassium-sparing diuretic. When trimethoprim reaches your kidneys, it latches onto tiny sodium channels in the distal tubules. These channels normally help pull sodium back into your blood. But when trimethoprim blocks them, sodium stays in the urine. And that’s where the problem starts.Your kidneys use the movement of sodium to create an electrical pull that pushes potassium out into the urine. No sodium reabsorption? No electrical gradient. No gradient? Potassium can’t leave. It builds up in your blood. This isn’t a slow, gradual effect. Studies show potassium levels can rise by 0.5 to 1.5 mmol/L within 48 to 72 hours of starting trimethoprim. That’s fast. That’s dangerous.
And here’s the kicker: trimethoprim concentrates in your kidneys at levels 10 to 50 times higher than in your bloodstream. So even though you’re only taking a small pill, your kidneys are getting a heavy dose. That’s why the risk isn’t just for people with kidney disease-it’s also for older adults, even those with normal kidney function.
Who’s at the Highest Risk?
Not everyone who takes trimethoprim gets hyperkalemia. But certain people are walking into a minefield without knowing it:- People over 65
- Those taking ACE inhibitors or ARBs (like lisinopril, losartan, or valsartan)
- Patients with chronic kidney disease (eGFR under 60)
- People with diabetes
- Anyone already on potassium supplements or potassium-sparing diuretics (like spironolactone)
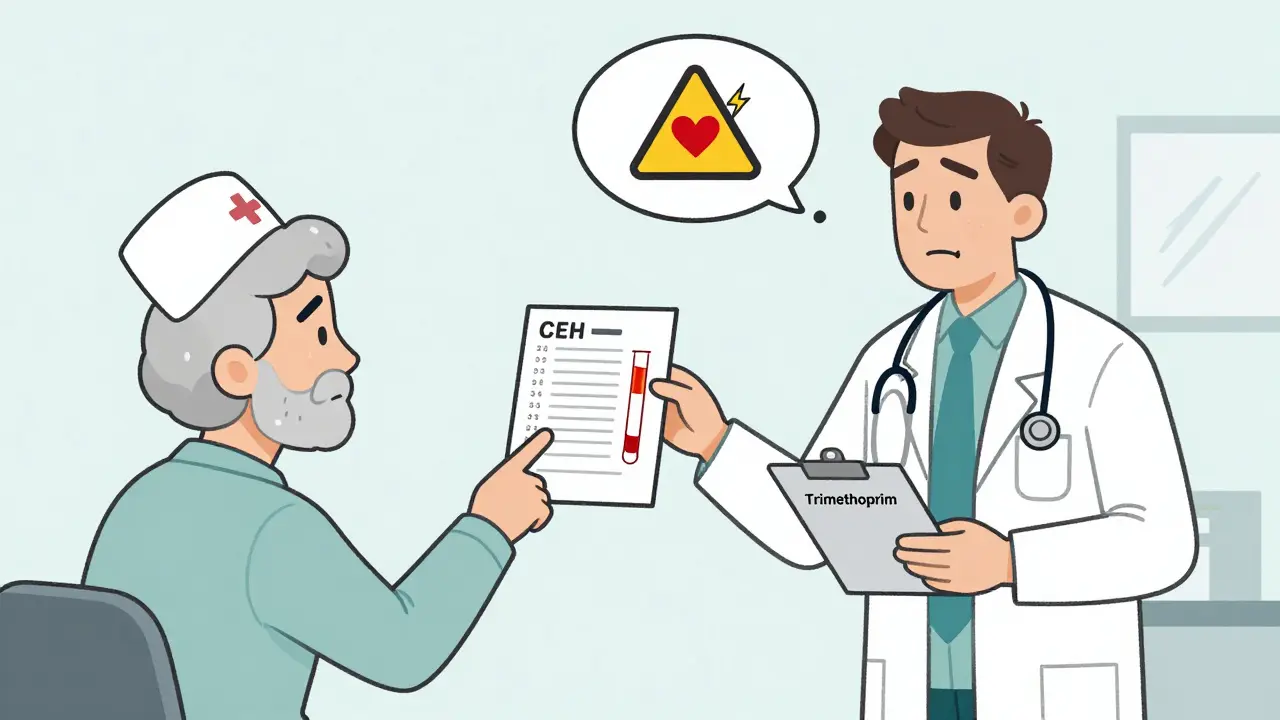
A 2020 study found that if you’re over 65, have diabetes, CKD, and are on an ACE inhibitor? Your chance of developing hyperkalemia on trimethoprim jumps to 32.1%. Compare that to 4.3% in people on other antibiotics. That’s not a small risk-it’s a red flag.
And here’s the truth: many doctors don’t realize how common this is. A 2023 survey showed only 41.7% of primary care doctors check potassium levels before prescribing Bactrim to patients on blood pressure meds. Emergency doctors? Only 32.4%. Meanwhile, nephrologists-doctors who specialize in kidneys-check it nearly 90% of the time.

Why Is This Still Happening?
Trimethoprim-sulfamethoxazole (TMP-SMX) is cheap, effective, and widely used. It’s the go-to for urinary tract infections, sinus infections, and preventing pneumonia in people with weakened immune systems. In 2022, over 14 million prescriptions were written in the U.S. alone. Nearly 30% of those went to people over 65.Even though the FDA added hyperkalemia to its boxed warning for trimethoprim in 2019, many prescribers still treat it like a harmless antibiotic. It’s not. A 2022 analysis of FDA adverse event reports found 1,247 cases of hyperkalemia linked to TMP-SMX between 2010 and 2020. Forty-three of those were fatal. Two-thirds of the deaths were in people over 65.
One doctor on Reddit described a 72-year-old woman on lisinopril who developed a potassium level of 6.8 after three days of Bactrim. She needed emergency dialysis. Another physician said they’d reviewed 200+ prescriptions for Bactrim in patients on ACE inhibitors-and only 15% had potassium over 5.5. That means 85% were fine. But those 15%? They were in serious trouble.
What Should You Do If You’re Prescribed Trimethoprim?
If you’re on an ACE inhibitor, ARB, or have kidney disease or diabetes, ask your doctor this:- Is there a safer alternative? Nitrofurantoin is just as effective for UTIs and doesn’t raise potassium.
- Can we check my potassium level before I start?
- Should I get a repeat test in 48 to 72 hours?
For most people, the answer to #1 is yes. Nitrofurantoin, fosfomycin, or cephalexin are all good options for UTIs. For pneumonia prophylaxis in immunocompromised patients, trimethoprim may still be necessary-but only if potassium is monitored closely.
Guidelines from the American Geriatrics Society and the American Society of Health-System Pharmacists are clear: don’t start trimethoprim in patients with baseline potassium above 5.0 mmol/L or eGFR under 30. And if you’re over 65 and on blood pressure meds? Avoid it unless there’s no other choice.
What If You’re Already Taking It?
If you’re already on trimethoprim and haven’t had your potassium checked:- Call your doctor. Ask for a simple blood test.
- Watch for symptoms: muscle cramps, weakness, irregular heartbeat, fatigue.
- If you feel off, get checked immediately. Don’t wait.
Many cases of hyperkalemia from trimethoprim are reversed quickly once the drug is stopped. But if it’s missed, the consequences can be fatal. Emergency treatments like calcium gluconate, insulin with glucose, or dialysis are often needed when potassium hits 6.0 or higher.
Is There a Better Way Forward?
Yes. Hospitals and clinics that added electronic alerts to their systems saw a 57% drop in hyperkalemia cases linked to trimethoprim. When the system automatically flags a patient on lisinopril who’s about to get Bactrim, and prompts the doctor to check potassium or switch antibiotics, lives are saved.A new risk-scoring tool called the TMP-HyperK Score helps predict who’s most at risk. It looks at four things: age over 65, baseline potassium above 4.5 mmol/L, eGFR under 60, and use of an ACE inhibitor or ARB. If you have three or four of those, your risk is high. That’s not guesswork-that’s science.
Experts agree: trimethoprim isn’t going away. It’s too useful for certain infections. But we need to stop treating it like any other antibiotic. It’s a potassium-sparing diuretic in disguise. And that changes everything.
Bottom Line
Trimethoprim is not harmless. For millions of people, especially older adults and those on common blood pressure meds, it’s a hidden danger. You don’t need to avoid it entirely-but you do need to know your risk. Ask for a potassium test before you start. Ask for alternatives. If your doctor says it’s fine without checking, ask why. Your heart might depend on it.Can trimethoprim cause hyperkalemia even if my kidneys are normal?
Yes. Even people with normal kidney function can develop hyperkalemia from trimethoprim. The drug concentrates in the kidneys and blocks potassium excretion directly. A case report in 2023 described an 80-year-old woman with normal creatinine levels who developed a potassium level of 7.8 mmol/L and cardiac arrest after just 72 hours of standard-dose Bactrim.
How quickly does potassium rise after starting trimethoprim?
Potassium levels typically begin rising within 24 to 48 hours and peak around 72 hours after starting the drug. Studies show the average time to peak potassium is 2.3 days, with most dangerous spikes occurring between day 1 and day 5. This is why guidelines recommend checking potassium at 48 to 72 hours after starting treatment.
What antibiotics are safer alternatives to trimethoprim?
For urinary tract infections, nitrofurantoin and fosfomycin are preferred alternatives because they don’t affect potassium levels. Cephalexin is another safe option. For pneumonia prophylaxis in immunocompromised patients, pentamidine or atovaquone may be used instead of trimethoprim-sulfamethoxazole, though they’re less convenient or more expensive.
Should I stop taking trimethoprim if I’m on lisinopril?
Don’t stop it on your own. Talk to your doctor. The combination of trimethoprim and ACE inhibitors like lisinopril increases hyperkalemia risk by 6.7 times compared to other antibiotics. Your doctor may switch you to a safer antibiotic or order a potassium test before continuing. Never discontinue antibiotics without medical advice unless you’re having symptoms of high potassium.
Is hyperkalemia from trimethoprim reversible?
Yes, in most cases. Stopping trimethoprim usually leads to a drop in potassium within 24 to 48 hours. In severe cases, emergency treatments like IV calcium, insulin with glucose, or dialysis may be needed to stabilize the heart. But if caught early, the condition is fully reversible with no lasting damage.
Do all doctors know about this risk?
No. A 2023 survey found only 41.7% of primary care doctors routinely check potassium before prescribing trimethoprim to patients on blood pressure medications. Nephrologists and infectious disease specialists are much more aware, but many frontline providers still treat it like a routine antibiotic. If your doctor hasn’t mentioned potassium, ask.