Statin Side Effect Calculator for Women
Estimate your risk for statin-related side effects based on the latest research showing how women experience statins differently than men.
Your Side Effect Risk Assessment
Muscle Pain Risk:
Diabetes Risk:
Based on research showing women experience side effects differently than men. You're not imagining your symptoms.
Women take statins at lower rates than men-even when they have the same risk for heart disease. Why? Because the side effects hit differently. Muscle pain, fatigue, increased diabetes risk, and communication gaps aren’t just random complaints. They’re real, documented, and sex-specific. If you’re a woman prescribed a statin and you’ve felt dismissed when you said something felt off, you’re not alone. And you’re not imagining it.
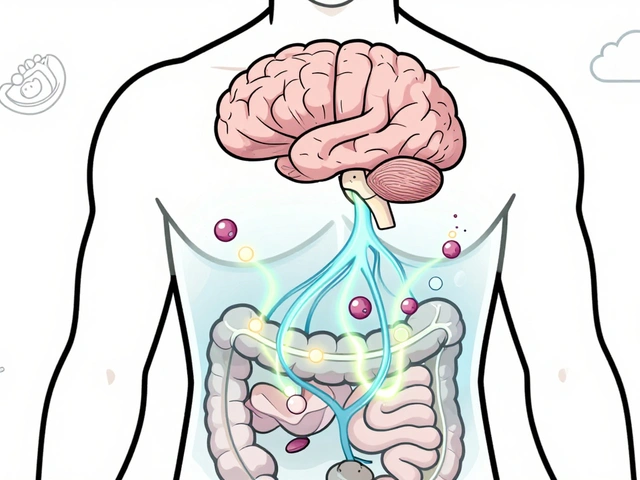
Statins Work the Same, But Your Body Handles Them Differently
Statins have been around since 1987. They lower LDL cholesterol by blocking HMG-CoA reductase, the enzyme your liver uses to make cholesterol. For both men and women, they reduce heart attacks, strokes, and death from cardiovascular disease by about 20-30%. That’s proven. But here’s where it gets personal: your body processes these drugs differently than a man’s.Women generally have lower kidney function after adjusting for body size-about 15-20% lower glomerular filtration rate. They also carry more body fat, on average 25-30% compared to 15-20% in men. That means statins stick around longer in your system. Higher exposure. Higher risk of side effects. Even at the same dose.
That’s why a 20mg dose of atorvastatin might be fine for a man but overwhelming for a woman. It’s not about being “sensitive.” It’s about biology.
Muscle Pain Isn’t Just “In Your Head”
The most common reason women stop statins? Muscle pain. Not just soreness. Real, persistent, sometimes debilitating aches and weakness. The USAGE survey found 31% of women reported new or worsening muscle symptoms compared to 26% of men. And those numbers aren’t small. They’re statistically significant-and they lead to real consequences.Women are 28.7% more likely than men to stop or switch statins because of side effects. For women over 65, the risk of statin-induced myopathy is 1.5 to 2 times higher than in men their age. Why? Lower muscle mass, slower drug clearance, and more medications. Elderly women often take blood pressure pills, blood thinners, or thyroid meds-all of which can interact with statins and boost toxicity.
And here’s the catch: doctors sometimes mistake this for “normal aging.” But muscle pain from statins doesn’t go away with rest. It gets worse with activity. If you’re noticing unexplained weakness in your thighs or shoulders, especially after starting a statin, it’s not just “getting older.” It’s a signal.
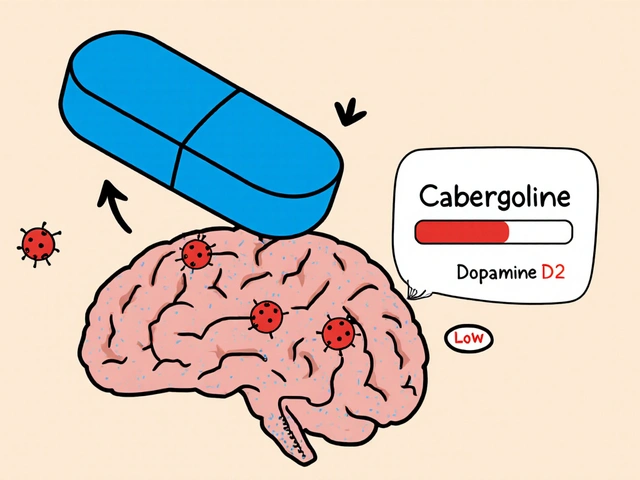
Diabetes Risk Is Real-And Higher in Women
The FDA added a warning to statin labels in 2012: these drugs can raise blood sugar. That’s not a rumor. It’s from large studies like JUPITER, which showed a 27% increase in diabetes risk with rosuvastatin over two years. A 2015 meta-analysis of nearly 96,000 people confirmed a 9% increased risk after four years.But here’s what most women don’t know: the risk appears higher in women than men. One analysis found a 12% increase in diabetes risk for women versus 8% for men. And it’s not dose-dependent. Even low-dose statins can trigger it after three years of use. That’s why post-menopausal women-already at higher risk for type 2 diabetes due to hormonal shifts-need extra vigilance.
That doesn’t mean you shouldn’t take a statin. The heart benefits still outweigh the diabetes risk for most women with high cholesterol or existing heart disease. But you should get your fasting blood sugar checked every 3-6 months after starting treatment. Don’t wait for symptoms like thirst, fatigue, or frequent urination. Prevention starts with monitoring.
Why You’re More Likely to Quit
It’s not just the physical side effects. The system isn’t set up for women.A 2019 study found women were 34% more likely than men to say their doctor never explained how high cholesterol leads to heart disease. Forty-two percent of women reported never getting a clear explanation-compared to just 31% of men. If you don’t understand why you’re taking a pill, you’re more likely to stop when you feel weird.
And when you do complain? You’re more likely to be told it’s “all in your head.” The data says otherwise. Women are 2.3 times more likely to try three or more statins before finding one they can tolerate. Yet, they’re 37% less likely to be offered alternatives like ezetimibe or PCSK9 inhibitors when statins fail.
That’s not just a gap in care. It’s a gap in trust. And it costs lives. In a 2020 study of over 127,000 statin users, women had 18.7% lower adherence at 12 months than men. Cost played a role-29% of women skipped doses because they couldn’t afford the meds, compared to 19% of men. But so did feeling unheard.
Special Cases: Pregnancy, Menopause, and Aging
If you’re a woman of childbearing age, statins are Category X-meaning they can cause birth defects. The FDA requires doctors to confirm you’re using reliable contraception before prescribing. Yet, a 2022 study found 15% of prescriptions to women aged 18-45 had no documented pregnancy prevention plan. That’s unacceptable.During menopause, your risk of heart disease spikes as estrogen drops. But so does your risk of muscle side effects. The Women’s Health Initiative found 41% of post-menopausal women reported muscle symptoms versus 33% of pre-menopausal women. Hormone changes affect how your muscles respond to statins. It’s not coincidence-it’s physiology.
And for women over 75? The risk of hospitalization from statin side effects is 2.1 times higher than in men your age. Why? Polypharmacy. Calcium channel blockers like diltiazem can triple the toxicity of simvastatin. Blood thinners like warfarin can raise bleeding risk by 25%. Your meds stack up. Your body doesn’t clear them as fast. That’s why lower doses and careful reviews are non-negotiable.

What You Can Do: A Practical Plan
You don’t have to suffer through statin side effects. Here’s what works:- Start low, go slow. Begin with the lowest effective dose-like atorvastatin 10mg or rosuvastatin 5mg. Wait 6-8 weeks before increasing. Most women don’t need high doses.
- Track symptoms. Keep a simple log: muscle pain (1-10), fatigue, new joint stiffness, changes in urine color. Bring it to your next visit.
- Ask for blood tests. Request CK (creatine kinase) levels if muscle pain is severe. Check fasting glucose every 3-6 months.
- Request alternatives. If you can’t tolerate statins, ask about ezetimibe, bempedoic acid, or PCSK9 inhibitors. These are not “second choices.” They’re valid, effective tools.
- Get genetic testing if you can. The SLCO1B1 gene variant increases myopathy risk in 23% of women. If you’ve had bad reactions before, a simple blood test can help avoid repeating the same mistake.
- Speak up. If your doctor says, “It’s probably not the statin,” ask for evidence. Show them the data. You’re not being difficult. You’re being informed.
It’s Not About Fear. It’s About Fairness.
Statins save lives. But they’re not one-size-fits-all. Women aren’t just smaller men. We metabolize drugs differently. We experience side effects differently. And we’ve been ignored for too long.The good news? Change is happening. The American Heart Association now recommends gender-specific dosing. New decision aids help women understand their risks and options. Genetic screening is becoming more accessible. Providers are being trained to listen.
But you don’t have to wait for the system to catch up. You have the right to be heard. To be tested. To be offered alternatives. To take control of your heart health without sacrificing your well-being.
Ask the questions. Demand the data. Know your body. Your heart deserves nothing less.
Do statins cause more side effects in women than in men?
Yes. Women report muscle pain, fatigue, and statin intolerance at higher rates than men. Studies show 31% of women experience new muscle symptoms compared to 26% of men. Women over 65 are 1.5 to 2 times more likely to develop statin-induced myopathy due to differences in kidney function, body fat, and drug metabolism.
Can statins cause diabetes in women?
Yes. Statins increase the risk of developing type 2 diabetes by 9-27%, depending on the drug and duration. Research shows this risk may be slightly higher in women-around 12% compared to 8% in men. The effect is seen even with low doses and is independent of statin type. Regular fasting glucose checks every 3-6 months are recommended for women on long-term statin therapy.
Should women start statins at a lower dose?
Yes. Clinical guidelines now recommend starting women on lower doses-like atorvastatin 10mg or rosuvastatin 5mg-especially if they’re older, petite, or taking other medications. The Dutch STATINWISE trial showed that starting low and titrating slowly improved adherence by 32% in women. High doses are rarely needed for women to reach LDL goals.
Are there alternatives to statins for women who can’t tolerate them?
Yes. Ezetimibe, bempedoic acid, and PCSK9 inhibitors are proven alternatives that lower LDL cholesterol without the same muscle-related side effects. Yet, women are 37% less likely to be offered these options. If you can’t tolerate statins, ask specifically about these medications. They’re not second-tier-they’re essential tools for women with statin intolerance.
Is it safe to take statins during menopause?
Statins are safe and often recommended during menopause, when heart disease risk rises sharply. However, muscle side effects become more common-41% of post-menopausal women report them versus 33% of pre-menopausal women. Starting with a low dose and monitoring for symptoms is key. The cardiovascular benefits still outweigh the risks for most women with elevated LDL or existing heart disease.
Why do doctors sometimes dismiss women’s statin side effects?
Historically, women were underrepresented in clinical trials, leading to assumptions that side effects are “atypical.” But data shows women’s complaints are biologically valid. Studies confirm higher rates of muscle symptoms, drug interactions, and metabolic differences. Dismissing them stems from implicit bias, not science. Women should insist on evidence-based evaluations-not assumptions.
Can genetic testing help determine if statins are right for me?
Yes. A gene variant called SLCO1B1 is found in 23% of women (vs. 18% of men) and significantly increases the risk of statin-induced muscle damage. If you’ve had unexplained muscle pain on statins before, genetic testing can help avoid repeating the same reaction. It’s not routine yet, but it’s available and increasingly recommended for women with prior intolerance.
Should women on statins get their blood sugar checked regularly?
Yes. Because statins increase diabetes risk-and that risk appears higher in women-it’s recommended to check fasting blood glucose every 3-6 months after starting treatment. Early detection allows for lifestyle changes or medication adjustments before full-blown diabetes develops. Don’t wait for symptoms like excessive thirst or fatigue.
Is it safe to take statins if I’m planning to get pregnant?
No. All statins are classified as Pregnancy Category X due to confirmed risks of birth defects in animal studies. If you’re of childbearing age and prescribed a statin, your doctor must confirm you’re using reliable contraception. If you’re planning pregnancy, stop statins at least 3 months before trying to conceive and discuss alternative cholesterol management with your provider.
What’s the best way to talk to my doctor about statin side effects?
Be specific. Say: “I started this statin and now I have persistent muscle aches in my thighs and fatigue. I’ve read this is common in women and want to know if it’s related.” Bring a symptom log. Ask: “Is there a lower dose I can try?” or “What are my alternatives?” If you feel dismissed, ask for a referral to a preventive cardiologist or lipid specialist. Your concerns are valid-and there are solutions.



December 17, 2025 AT 13:18
I started statins last year and thought my constant leg pain was just from walking too much. Then I read this and realized-I wasn’t imagining it. My doctor said, 'It’s probably just aging.' But I’m 52, not 82. I stopped the statin and the pain faded in two weeks. I’m not anti-medication-I just want to be heard. This article? Lifesaver.
Also, I got my SLCO1B1 tested. Turns out I’m positive. No wonder I couldn’t tolerate simvastatin. Why isn’t this routine??