Every year, over 120,000 people in the U.S. die from lung cancer. That’s more than colon, breast, and prostate cancers combined. And yet, most cases are still caught too late - when treatment options are limited and survival rates drop to just 6%. But here’s the turning point: if lung cancer is caught early, survival jumps to 59%. The key? Screening. And not just for anyone - for people who smoked.
Who Should Be Screened? The Rules Have Changed
If you smoked a pack a day for 20 years - or two packs a day for 10 years - you’re in the high-risk group. That’s called a 20 pack-year history. It doesn’t matter if you quit 10, 15, or even 25 years ago. The risk doesn’t disappear. A 2022 JAMA Oncology study found former smokers 15 to 30 years after quitting still had 2.5 times higher risk of lung cancer than people who never smoked.
Until recently, guidelines said you had to quit within the last 15 years to qualify for screening. That’s changed. The American Cancer Society updated its rules in March 2023 and removed that cutoff entirely. Now, anyone aged 50 to 80 with a 20+ pack-year history - whether they still smoke or quit decades ago - should be screened annually. The U.S. Preventive Services Task Force (USPSTF) also updated its guidelines in 2021, lowering the starting age from 55 to 50 and reducing the pack-year threshold from 30 to 20. These changes opened the door for millions more people.
But here’s the problem: only 23% of lung cancer cases are found early. And only 18% of eligible people actually get screened. Why? Many don’t know they qualify. Primary care doctors often don’t bring it up. In a 2022 AMA survey, 42% of doctors said they weren’t even aware of the updated guidelines. If your doctor hasn’t mentioned screening, ask. It’s not optional for high-risk people - it’s life-saving.
What Does the Screening Actually Involve?
The test is simple: a low-dose CT scan (LDCT). It’s not a regular chest X-ray. It’s a quick, non-invasive scan that takes less than a minute. You lie on a table, hold your breath for a few seconds, and that’s it. The radiation dose is 70-80% lower than a standard CT scan - about the same as a mammogram.
It’s not perfect. About 96% of positive scans turn out to be false alarms. A small spot on the lung might be a scar, an infection, or just a harmless nodule. But that’s why follow-up is built into the system. If something shows up, you get another scan in 3 to 6 months. If it grows, you move to biopsy. If it doesn’t, you keep screening yearly. The goal isn’t to panic at every shadow - it’s to catch the real ones before they spread.
AI is helping. Since January 2023, the FDA has approved AI tools like LungQ by Riverain Technologies that analyze scans faster and more accurately. These tools reduce unnecessary follow-ups by 15-22%. They don’t replace radiologists - they help them focus on what matters.
Why Screening Isn’t Working for Everyone
Even with better guidelines, access is still unequal. Rural areas have 67% fewer screening centers than cities. Black Americans are 35% less likely to be screened than white Americans. And Medicare only covers screening for people aged 50 to 77 - leaving out those 78 and older, even if they’re healthy and eligible.
Insurance is another hurdle. Some private insurers still follow the old 30 pack-year rule. If you’re told you don’t qualify, ask for a copy of their policy. Often, they’re using outdated standards. The Affordable Care Act requires coverage for services with a USPSTF ‘B’ grade - and lung cancer screening has that. You shouldn’t pay out of pocket.
And then there’s the human factor. Many people don’t get screened because they’re scared. Or they think it’s too late. Or they don’t believe it’ll help. But the data doesn’t lie. The National Lung Screening Trial showed a 20% drop in lung cancer deaths among those who got screened yearly for three years. That’s 6,600 lives saved each year - just from expanding eligibility to age 50 and 20 pack-years, as Dr. David F. Yankelevitz pointed out in JAMA.
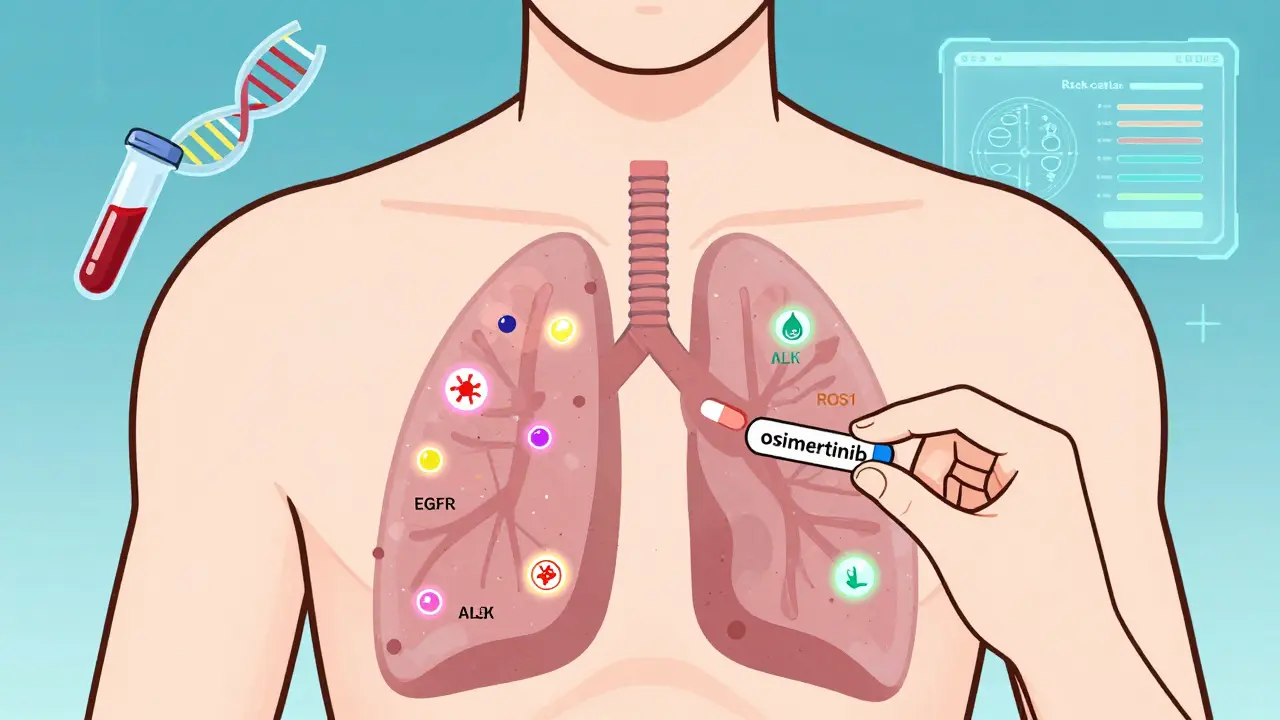
Targeted Therapy: What Happens After a Diagnosis
Screening doesn’t just find cancer early - it finds the right kind of cancer. More than 60% of early-stage lung cancers now have identifiable genetic mutations. These are the ones that respond to targeted therapy.
Before, surgery was the only option for early-stage disease. Now, if you have an EGFR mutation - one of the most common - you can take a drug like osimertinib after surgery. The ADAURA trial in 2021 showed this cut the risk of recurrence or death by 83%. That’s not just survival. That’s long-term remission.
Other mutations matter too. ALK, ROS1, RET, MET, NTRK - each has its own targeted drug. And these aren’t just for advanced cancer anymore. They’re being used in stage IB to IIIA, right after surgery, to wipe out any leftover cancer cells.
The future is even clearer. By 2025, experts predict 70% of early-stage lung cancers found through screening will have an actionable mutation - compared to just 30% in late-stage cases. That’s because tumors caught early haven’t had time to evolve into complex, resistant forms. They’re still predictable. Still treatable.
The Next Frontier: Liquid Biopsies and Risk Prediction
What if you could detect cancer before it shows up on a scan? That’s where liquid biopsies come in. These are blood tests that look for tumor DNA floating in the bloodstream. They’re not ready for prime time yet, but trials like NCT04541082 and NCT04924022 are testing them alongside LDCT scans. The goal? Find molecular signals before a tumor is even visible.
And then there’s the PACIFIC trial - launching in 2024. It’s tracking 10,000 people to see if adding genetic risk scores and environmental factors (like radon exposure or air pollution) can make screening smarter. Instead of just asking, “Did you smoke?” we might soon ask, “What’s your personal risk score?”
Imagine a future where your doctor doesn’t just check your smoking history - they run a simple blood test and a risk calculator, then say, “You have a 7% chance of developing lung cancer in the next five years. Let’s get you on a screening plan.” That’s not science fiction. It’s coming.
What You Can Do Right Now
If you’re between 50 and 80 and have a 20+ pack-year history - even if you quit decades ago - ask your doctor about LDCT screening. Don’t wait for them to bring it up. Bring it up yourself.
If you’re still smoking, get help quitting. Screening doesn’t replace quitting - it complements it. In fact, the best screening programs now bundle in counseling and nicotine replacement. The American Thoracic Society says 70% of current smokers want to quit - but only 30% get any support. That’s unacceptable.
If you’ve been told you’re not eligible - ask why. Check your insurance policy. Compare it to the 2023 ACS and 2021 USPSTF guidelines. You might be eligible and just not know it.
And if you’re a caregiver, a family member, or a friend of someone who smoked - share this. Lung cancer doesn’t care if you’re rich, young, or healthy. It cares if you smoked. And if you did - screening could give you back years you didn’t know you had.
Frequently Asked Questions
Who qualifies for lung cancer screening?
You qualify if you’re between 50 and 80 years old, have a 20+ pack-year smoking history (for example, one pack a day for 20 years, or two packs a day for 10 years), and currently smoke or quit within the last 15 years (or any time if following the 2023 ACS guidelines). No symptoms are required. If you’ve quit smoking more than 15 years ago but still have a 20+ pack-year history, you may still be eligible under the American Cancer Society’s 2023 guidelines.
Is the LDCT scan dangerous because of radiation?
No. A low-dose CT scan uses 70-80% less radiation than a standard CT scan. The dose is similar to what you’d get from natural background radiation over about six months. The benefit of catching cancer early far outweighs the tiny risk from radiation. It’s not a reason to skip screening.
What if the scan finds something? Does that mean I have cancer?
Not at all. Over 96% of positive scans are false positives - meaning they show something unusual that isn’t cancer. It could be a scar, an infection, or a benign nodule. The next step is usually a follow-up scan in 3 to 6 months to see if it changes. Only if it grows or looks suspicious will doctors recommend a biopsy. Most people never need one.
Can I get screened if I’ve never smoked?
Generally, no. Screening is only recommended for people with a significant smoking history. However, non-smokers with a strong family history of lung cancer or exposure to radon, asbestos, or air pollution may be considered for screening in special cases - but this is still under research and not yet standard practice.
Does insurance cover lung cancer screening?
Yes, under the Affordable Care Act, Medicare and most private insurers must cover annual LDCT screening for eligible individuals at no cost to you. Medicare covers people aged 50-77 with a 20+ pack-year history who currently smoke or quit within the past 15 years. Some insurers still use outdated rules - if you’re denied, ask for a copy of their policy and compare it to the 2021 USPSTF or 2023 ACS guidelines.





February 16, 2026 AT 23:57
Man, I never realized how much the guidelines changed until I read this. My dad quit smoking 22 years ago after 2 packs a day for 15 years. His doctor told him he was 'off the hook' last year. That’s wild. We’re talking about a guy who’s lived with the fear of this for decades, and now? He’s eligible. No one told him. No one even asked. It’s like the system forgot half the people it’s supposed to protect.
And the AI tools? Mind blown. LungQ basically does the grunt work so radiologists don’t miss the tiny red flags. That’s not magic-that’s just good engineering. We need more of this. Not just in cancer, but everywhere the system’s drowning in data and under-staffed.
Also, 96% false positives? Yeah, that’s scary-but also kind of beautiful. It means we’re catching things so early that most of them aren’t even cancer. We’re seeing ghosts before they become monsters.