Every year, hospitals, pharmacies, and military depots throw away billions of dollars worth of medicine - not because it’s unsafe, but because the date on the bottle has passed. The U.S. military has been quietly proving for nearly 40 years that many of those drugs are still perfectly good. Their Shelf Life Extension Program (SLEP) isn’t just a cost-saving trick. It’s a scientific revelation about how drugs really behave over time.
What Is the Shelf Life Extension Program?
Started in 1986, the Shelf Life Extension Program is a joint effort between the U.S. Department of Defense and the Food and Drug Administration. Its goal? To test drugs stored in federal stockpiles - like those in the Strategic National Stockpile - and see if they’re still effective long after their labeled expiration dates. If they pass, the FDA extends their usable life. No guesswork. No assumptions. Just hard data. These aren’t random pills pulled from a pharmacy shelf. These are carefully stored, sealed, and tracked medications kept in climate-controlled facilities, often in their original packaging. The program tests everything from antibiotics to antivirals, painkillers, and even epinephrine auto-injectors used in emergencies. The process is strict. Each batch is sampled, tested in FDA labs, and analyzed for potency. To qualify for an extension, the drug must still contain at least 85% of its original active ingredient. That’s not a loose standard. It’s the same bar used to approve new drugs in the first place.How Much Longer Do These Drugs Last?
The numbers are staggering. A 2006 study in the Journal of Pharmaceutical Sciences tested 122 different drugs under SLEP. Eighty-eight percent of them were still effective more than 15 years after their original expiration date. Some lasted over two decades. Take oseltamivir (Tamiflu), a key antiviral used during flu pandemics. In 2019, the Strategic National Stockpile extended its shelf life by three years - preserving 22 million treatment courses. That’s enough to protect millions of people during a crisis without having to manufacture new doses. The Department of Defense reports that, on average, each extension adds 2.8 years to a drug’s usable life. Since 1986, over 2,500 different products have been extended. That’s not just a few bottles. That’s entire warehouses of life-saving medicine kept in reserve.Why Do Commercial Expiration Dates Exist?
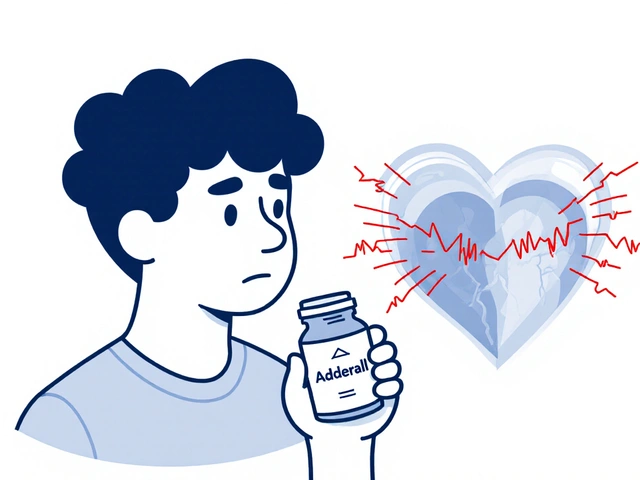
You’ve probably seen the expiration date on your medicine: “Use by 05/2025.” That date isn’t a death sentence for the drug. It’s a conservative estimate set by manufacturers - usually based on two to three years of testing under ideal conditions. Beyond that, they’re not legally required to prove it still works. Pharmaceutical companies don’t test drugs for 10 or 20 years. It’s expensive. And if a drug lasts longer than the label says, it doesn’t help them sell more. So they set a date that’s safe, simple, and profitable. The military doesn’t have that problem. Their job is to keep the nation ready for emergencies. If a drug works after 15 years, they’ll use it. That’s why SLEP exists - not to cut corners, but to make sure nothing goes to waste when lives are on the line.How Much Money Does SLEP Save?
Between 2005 and 2015, SLEP saved the federal government an estimated $2.1 billion. That’s not a rounding error. That’s enough to buy 40 million doses of insulin, or fund a year’s worth of flu vaccines for the entire U.S. population. The savings come from avoiding replacements. A single vial of antibiotics might cost $50. Multiply that by thousands of vials, and you’re talking millions. Now imagine doing that every two years for every drug in the stockpile. Without SLEP, the cost would be unsustainable. A 2019 study in Health Affairs found that the commercial pharmaceutical industry discards about $1.7 billion in usable drugs every year in the U.S. alone. That’s mostly because of expiration dates - not because the drugs are bad. Military treatment facilities that fully follow SLEP protocols cut pharmaceutical waste by 38% compared to those that don’t. That’s $87 million saved annually just in military hospitals.
What’s Different About Military Storage?
This is the key point: SLEP doesn’t prove your medicine cabinet is safe. It proves that drugs stored under perfect conditions - cool, dry, dark, sealed - stay stable far longer than we thought. The military follows strict storage rules outlined in the Materiel Quality Control Storage Standards (MQCSS). Temperature, humidity, light exposure, and packaging are all monitored and documented. A drug stored in a hot garage or a humid bathroom won’t last as long. That’s not SLEP’s fault - that’s common sense. Dr. Michael D. Swartzburg from UCSF warns: “Don’t assume your expired aspirin is safe because the military extended their stock.” He’s right. SLEP’s findings apply only to the exact lot numbers, packaging, and storage conditions tested. You can’t take one data point and apply it to every pill in your medicine cabinet. The FDA makes this clear in its 2021 guidance: shelf-life extensions under SLEP are specific. They’re not a green light for consumers to use expired drugs at home.How Does the Program Work in Practice?
It’s not magic. It’s logistics. Here’s how it works step by step:- A federal agency - like the Army or the Strategic National Stockpile - identifies a drug that’s nearing its expiration date.
- The drug is flagged for testing. Only Type II items (those approved for extension) are eligible.
- The FDA collects samples from sealed, properly stored stockpiles.
- Lab tests measure potency, chemical breakdown, and purity.
- If the drug meets the 85% potency threshold, the FDA approves an extension.
- The extension is added to the DoD Shelf Life Extension System (SLES), a central database.
- Logistics teams update records and redistribute the drug if needed.
What’s Changed Since 2021?
The program has evolved. In 2021, it expanded to include certain biological products - like vaccines and antitoxins - for the first time. These are trickier to store and test because they’re more sensitive to temperature and time. But the results so far show promise. The 2023 National Defense Authorization Act added more medical countermeasures for chemical, biological, and nuclear threats to the program. That’s a big deal. It means the military is preparing for next-generation threats with smarter, more efficient stockpiling. The FDA’s 2022-2026 Strategic Plan is now investing in advanced tools like mass spectrometry and predictive modeling. These technologies could one day forecast how a drug will degrade - without waiting years to test it. That could speed up extensions and expand the program even further.






January 30, 2026 AT 00:43
The Shelf Life Extension Program (SLEP) represents a rare instance where government efficiency aligns with scientific rigor. The 85% potency threshold is not arbitrary-it mirrors the FDA’s original approval criteria, ensuring that extended drugs meet the same safety and efficacy benchmarks as newly manufactured ones. The 2.1 billion in savings between 2005 and 2015 is statistically significant, and when contextualized against the $1.7 billion in commercial waste, it becomes clear that expiration dates are largely a product of liability management rather than pharmacological reality.