What Happens After a Stroke?
When a stroke hits, it doesn’t just stop the brain from working-it shatters routines, independence, and sometimes identity. But the story doesn’t end there. The brain isn’t broken beyond repair. It’s wounded, yes, but it has an incredible ability to heal itself. This is called neuroplasticity. It’s not magic. It’s science. And when paired with the right rehabilitation, it can bring back movement, speech, and even joy.
Recovery isn’t a straight line. It’s messy, slow, and sometimes frustrating. But it’s possible. Most people regain at least some function, especially when therapy starts early. The first 24 to 72 hours after a stroke are critical. Starting rehab within a day can improve mobility outcomes by 35% compared to waiting. That’s not a small difference-it’s the difference between needing full-time help and walking again with a cane.
The Three Phases of Stroke Recovery
Recovery doesn’t happen all at once. It unfolds in stages, each with its own goals and challenges.
Phase One: Recovery and Natural Healing (Days to Weeks)
This is the body’s first response. Swelling goes down. Some movement returns on its own. But don’t mistake this for full recovery. Without intervention, muscles stiffen. Joints lock. Depression creeps in. That’s why therapists start positioning the body correctly within hours-even if the patient is still in bed. Passive range-of-motion exercises, done two to three times a day, keep joints flexible. Preventing contractures (permanent tightening of muscles) is a top priority. Left untreated, contractures affect 30 to 50% of stroke survivors.
Phase Two: Retraining (Weeks to Months)
This is where the real work begins. The brain needs to relearn how to move, speak, and think. This isn’t about brute force. It’s about repetition, precision, and cues. Occupational therapists use visual prompts-like pointing to a wheelchair brake-so the brain starts linking the sight of the brake with the action of stopping. Physical therapists focus on walking. Constraint-induced therapy, where the stronger arm is strapped down for 90% of the day, forces the weaker one to work. Studies show this leads to 30% better motor gains than standard therapy.
Technology is helping too. Robotic exoskeletons like the Lokomat guide legs through walking motions with perfect repetition. Virtual reality games make arm exercises feel like playing tennis or catching falling objects. Functional electrical stimulation sends tiny pulses to paralyzed muscles, helping them fire again. These tools don’t replace therapists-they amplify their work.
Phase Three: Adaptation (Months to Years)
Not every function comes back. And that’s okay. Adaptation isn’t giving up. It’s learning to live well with what remains. Maybe you can’t grip a coffee cup the same way. But with a weighted handle or a built-up grip, you can. Maybe your speech is slower. You learn to pause, to use gestures, to let others know you’re still thinking. This phase is about environment and mindset. Grab bars in the bathroom. Raised kitchen counters. Voice-activated lights. These aren’t luxuries-they’re lifelines.
The Team Behind the Recovery
No single person can do this alone. Stroke rehab is a team sport. And the patient? They’re the captain.
You need a physiatrist (rehab doctor) to oversee everything. A neurologist to monitor brain health. Nurses to manage medications and skin care. Physical therapists for walking and strength. Occupational therapists for dressing, cooking, and bathing. Speech-language pathologists for swallowing and talking. Psychologists to tackle depression-because 30 to 35% of stroke survivors develop it. Social workers help with housing, insurance, and returning to work. Nutritionists make sure diet supports healing, not inflammation.
The most successful programs hold regular team meetings. When everyone talks-when the PT shares that the patient’s balance is improving, and the OT notes they’re now cooking meals again, and the psychologist says their mood has lifted-the whole plan shifts for the better. Facilities with structured team meetings see 22% better outcomes than those without.

How Much Therapy Is Enough?
More isn’t always better-but too little is deadly.
The American Stroke Association says medically stable patients should get three hours of therapy, five days a week, in an inpatient rehab unit. That’s not a suggestion. It’s the minimum standard for real progress. Outpatient therapy? It should still be intense. Two to three times a week, with daily home exercises.
Balance training is non-negotiable. Six in ten stroke survivors struggle with balance. That means falls. Broken hips. Hospital readmissions. A structured balance program-standing on one foot, stepping over lines, using foam pads-cuts fall risk by nearly half.
And timing matters. Waiting two weeks to start therapy? You lose ground. Starting on day three? You gain it back. The brain’s ability to rewire is strongest in the first few months. After six months, progress slows-but it doesn’t stop. Some people keep improving for years.
The Hidden Factors That Make or Break Recovery
It’s not just about how much therapy you get. It’s about who you are.
Research shows nine key factors determine how well someone recovers:
- General health before the stroke
- Range of motion in joints
- Muscle strength
- Bowel and bladder control
- Pre-injury level of independence
- Home and social support
- Ability to learn new things
- Willingness to try
- How you handle stress
Among all these, motivation is the biggest predictor. Studies show it accounts for up to 40% of recovery success. Someone who believes they can get better? They do. Someone who feels hopeless? They plateau-even with perfect therapy.
That’s why family involvement is so powerful. When loved ones join therapy sessions, ask questions, and help with daily exercises, adherence jumps by 37%. A daughter who reminds her dad to do his arm exercises. A spouse who walks with them every morning. These aren’t just nice gestures. They’re medical interventions.
New Frontiers in Recovery
The science is moving fast. What worked five years ago isn’t the best option today.
Transcranial magnetic stimulation (TMS) uses magnets to gently stimulate the brain. When combined with physical therapy, it boosts motor recovery by 15 to 20%. It’s not available everywhere-but it’s in major hospitals across Australia and the U.S.
Artificial intelligence is now analyzing brain scans to predict which therapies will work best for each person. One system in Melbourne tracks hand movement patterns and adjusts virtual reality tasks in real time-making therapy feel like a video game that gets smarter as you do.
And telerehabilitation? It’s no longer a backup. Recent studies show it’s 85% as effective as in-person care for speech, mobility, and strength training. For people in rural areas or those with transportation issues, this is revolutionary.
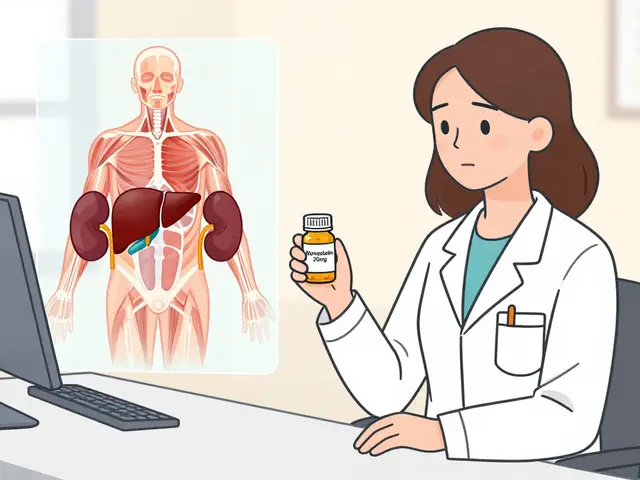
Even medications are being tested. Drugs that boost BDNF (brain-derived neurotrophic factor)-a protein that helps brain cells grow-are showing promise in early trials. They won’t cure stroke, but they might help the brain heal faster.
What to Expect Long-Term
Recovery isn’t a finish line. It’s a new way of living.
Most people don’t go back to exactly how they were before. But many return to meaningful lives. They garden. They drive. They travel. They play with grandkids. They laugh again.
The key is consistency. Even after formal therapy ends, daily movement matters. Walking. Stretching. Using the affected hand to open jars. Talking out loud-even if it’s just to yourself.
And rest? Don’t ignore it. Recovery needs downtime. Aim for 30 to 40% of your day in rest, 40 to 50% in therapy or activity, and 20 to 30% in social connection. Push too hard, and fatigue sets in. Push too little, and progress stalls.
There’s no magic number of weeks to recovery. Some see big gains in three months. Others take two years. What matters is that you keep going. The brain doesn’t give up. You shouldn’t either.
Final Thoughts: Hope Is Built, Not Found
Stroke steals. But rehab rebuilds. It doesn’t promise perfection. But it promises progress. And that’s enough.
Every step, every word, every grip of a spoon-these aren’t small victories. They’re the building blocks of a new life. And they’re possible. Not because of luck. But because of science, persistence, and people who refuse to let a stroke be the end of the story.






December 30, 2025 AT 22:31
I cried reading this. 🥹 My mom had a stroke last year and they told us she’d never walk again. Now she’s gardening again. Neuroplasticity is real. Don’t listen to the naysayers.
Also, the part about weighted utensils? YES. We bought those from Amazon for $12 and it changed everything. She can hold her coffee again. 🫖