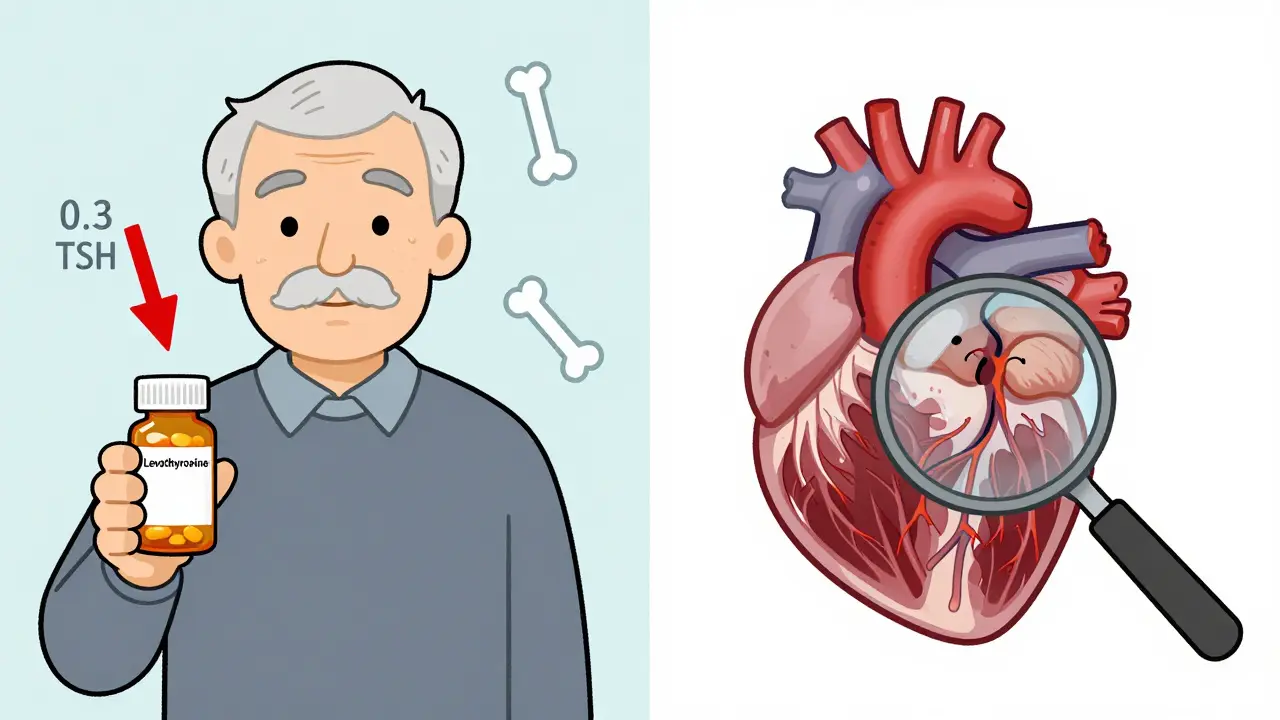
Most people don’t realize their thyroid is quietly affecting their heart-until something goes wrong. Subclinical hyperthyroidism is one of those silent conditions. Your thyroid hormones are normal, but your TSH (thyroid-stimulating hormone) is too low. It doesn’t cause the classic symptoms like weight loss or shaky hands. Yet, for many, especially over 65, this small lab abnormality can quietly raise the risk of heart rhythm problems, heart failure, and even broken bones.
What Exactly Is Subclinical Hyperthyroidism?
Subclinical hyperthyroidism means your TSH is below 0.45 mIU/L, but your free T4 and free T3 levels are still in the normal range. That’s it. No feverish sweats, no racing pulse, no jittery nerves. You might feel perfectly fine. That’s why it’s often found by accident-during a routine blood test for something else.
The condition becomes more common as you age. About 4 to 8% of adults have it. But in people over 75, that number jumps to nearly 1 in 6. It’s often linked to nodules in the thyroid-small lumps that produce extra hormone without causing obvious swelling. It can also happen if someone is taking too much thyroid medication, especially after treatment for hypothyroidism.
The key is persistence. One low TSH reading isn’t enough. Doctors need to see it confirmed over time, usually with two or three tests spaced a few months apart. That’s because stress, illness, or even certain medications can temporarily suppress TSH. Real subclinical hyperthyroidism sticks around.
Why Your Heart Is at Risk
Even if you feel fine, your heart isn’t fooled. Low TSH means your body is being exposed to slightly more thyroid hormone than it needs. That extra push makes your heart work harder.
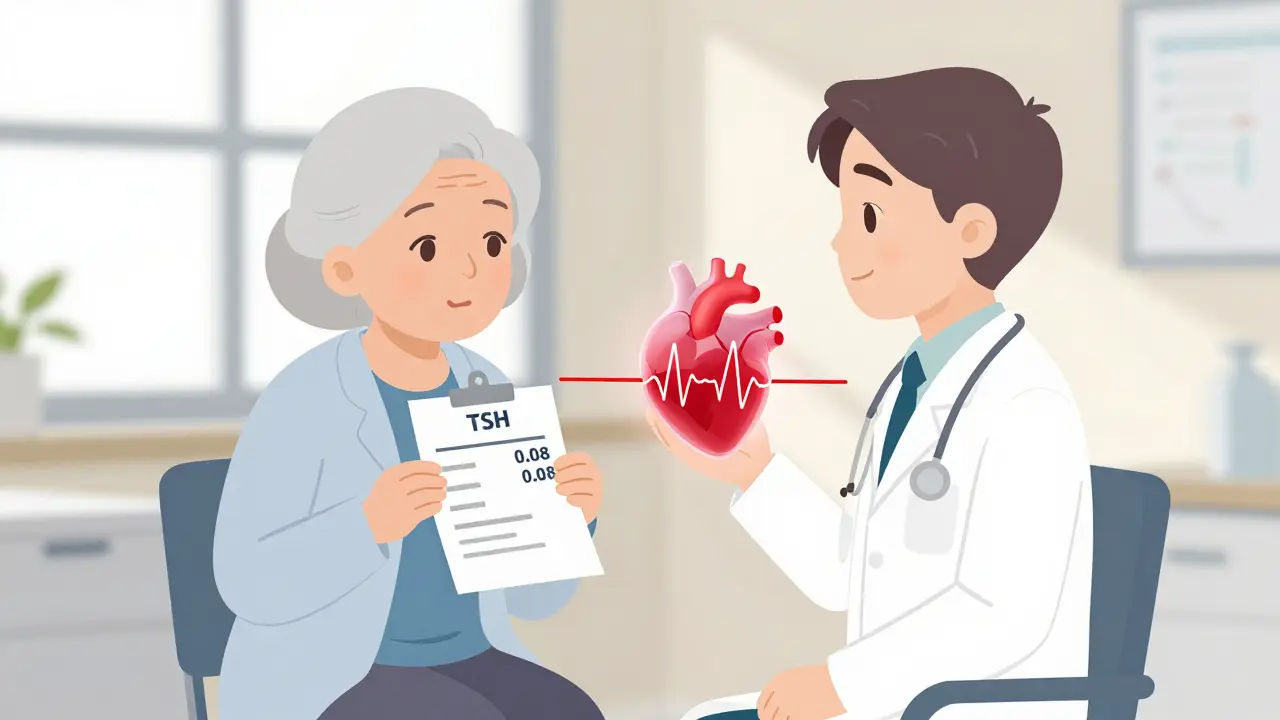
Studies show people with TSH below 0.1 mIU/L have more than double the risk of atrial fibrillation-a chaotic, irregular heartbeat that can lead to stroke. One analysis of nearly 9,000 people found the risk jumped by 154% compared to those with normal TSH. Even those with TSH between 0.1 and 0.44 mIU/L had a 63% higher risk.
Heart failure is another concern. A 10-year study of over 25,000 people found those with TSH below 0.1 had almost double the chance of developing heart failure. The heart muscle thickens, the chambers don’t fill properly, and the rhythm gets unstable. Left ventricular mass increases. Heart rate variability drops. These aren’t just lab numbers-they’re signs your heart is under strain.
And it’s not just older adults. People with existing heart disease-like prior heart attacks, high blood pressure, or valve problems-are especially vulnerable. Even mild TSH suppression can tip the balance. One study found that among patients with heart failure, those with subclinical hyperthyroidism had worse outcomes, regardless of age.
Bones, Brains, and Beyond
The heart isn’t the only system at risk. Bone density takes a hit, too. When TSH drops below 0.1, the body breaks down bone faster than it rebuilds it. One study showed a 2.3 times higher risk of fractures in these patients, especially in the hip and spine. That’s a big deal for older adults, where a single fall can change everything.
Cognitive effects are less clear, but emerging data suggests trouble. A 2016 study in older adults found subtle declines in executive function-things like planning, focusing, and switching tasks. It’s not dementia, but it’s enough to notice. You might find yourself forgetting appointments more often or struggling to follow complex instructions.
Quality of life? Usually fine in mild cases. But once heart symptoms kick in-palpitations, shortness of breath, fatigue-life changes. And that’s when treatment becomes less about numbers and more about how you feel.
When to Treat-It’s Not One-Size-Fits-All
Here’s where things get tricky. Not everyone with low TSH needs treatment. The guidelines are clear: it depends on how low your TSH is, how old you are, and what else is going on with your health.
If your TSH is below 0.1 mIU/L and you’re over 65, treatment is usually recommended. The same goes if you already have heart disease, osteoporosis, or a history of fractures. Even if you feel fine, the long-term risks outweigh the benefits of waiting.
If your TSH is between 0.1 and 0.44 mIU/L, the case is weaker. Treatment isn’t automatic. You need at least one other risk factor: symptoms like palpitations, signs of heart strain on an ECG, or low bone density. If you’re young, healthy, and have no symptoms, many doctors will just watch and retest in 6 to 12 months.
For those on thyroid medication (like levothyroxine), the fix is often simple: lower the dose. Many people with subclinical hyperthyroidism are overmedicated. A small reduction can bring TSH back into range without triggering hypothyroidism.
For endogenous causes-like a toxic nodule-options include radioactive iodine or surgery. Radioactive iodine is common in the U.S. It destroys the overactive tissue. But it often leads to permanent hypothyroidism, which means lifelong medication. That’s a trade-off. For some, it’s worth it to remove the heart risk. For others, especially those with multiple health problems, the risks of treatment may be higher than the condition itself.
What Treatment Actually Looks Like
First-line treatment isn’t always about fixing the thyroid. Often, it’s about protecting the heart. Beta-blockers like metoprolol or atenolol are used to slow the heart rate, reduce palpitations, and lower blood pressure. They don’t fix the thyroid problem, but they ease the strain on the heart. Many patients feel better within weeks.
For those needing to treat the thyroid itself, radioactive iodine is the most common choice for toxic nodules. It’s non-surgical, outpatient, and effective. But it’s permanent. You’ll likely become hypothyroid afterward. That’s not a failure-it’s a planned outcome. The goal isn’t to keep you in a gray zone. It’s to get you to stable, normal thyroid function.
Surgery is less common, usually reserved for very large nodules or when there’s suspicion of cancer. It carries more immediate risks but avoids radiation.
There’s no magic pill that fixes subclinical hyperthyroidism without consequences. That’s why decisions are so personal. A 72-year-old with atrial fibrillation and osteoporosis? Treat. A 55-year-old runner with TSH at 0.3 and no symptoms? Monitor.
Monitoring: The Most Important Tool
For many, treatment isn’t the answer-monitoring is. That means regular TSH checks. If your TSH is below 0.1, get tested every 3 to 6 months. If it’s between 0.1 and 0.44 and you’re low-risk, once a year is enough.
But don’t stop at TSH. If you’re being watched, you also need:
- An ECG every 6 to 12 months to check for atrial fibrillation
- Bone density scans every 1 to 2 years if you’re over 65 or have other risk factors
- Heart ultrasound (echocardiogram) if your doctor suspects structural changes
And if you’re on thyroid medication, your doctor should check your dose every 6 months-no matter how stable you feel. Doses that were right five years ago may be too high now.
The Big Debate: Treat Early or Wait?
There’s no global agreement. European guidelines say: treat everyone with TSH below 0.1. American guidelines say: treat selectively. Why the difference?
It comes down to risk tolerance. European experts see the data: high risk of heart problems, high risk of fractures. They act early. American experts worry about overtreatment. Creating hypothyroidism can bring its own problems-fatigue, weight gain, higher cholesterol, even increased heart disease risk in some cases.
Dr. Jacqueline Jonklaas, who helped write the U.S. guidelines, puts it simply: "We treat based on clinical judgment, not just a number." That means your age, your heart, your bones, your lifestyle-all of it matters.
And new studies are coming. The THAMES trial and the DEPOSIT study are tracking thousands of older adults over the next few years. They’ll tell us whether treating mild cases actually prevents heart attacks and strokes. Until then, we work with what we have: solid evidence that TSH below 0.1 is dangerous. TSH between 0.1 and 0.44? It’s a gray zone-and your doctor should help you navigate it.
What You Can Do Right Now
If you’ve been told you have subclinical hyperthyroidism:
- Don’t panic. This isn’t an emergency.
- Ask for your exact TSH number. Is it below 0.1? Between 0.1 and 0.44?
- Find out if you have any heart issues, bone loss, or symptoms like palpitations.
- Ask whether your thyroid medication dose might be too high.
- Request an ECG and bone density scan if you’re over 65.
- Set a reminder to get your TSH checked again in 3 to 12 months.
Subclinical hyperthyroidism isn’t something you cure. It’s something you manage-with awareness, monitoring, and smart choices. Your thyroid may be quiet, but your heart is listening. Make sure you’re listening, too.
Can subclinical hyperthyroidism cause weight loss?
Not usually. Unlike overt hyperthyroidism, where weight loss, heat intolerance, and tremors are common, subclinical hyperthyroidism typically doesn’t cause noticeable symptoms. Weight loss is rare unless TSH is very low (below 0.1) and the condition has progressed. Most people with this diagnosis feel fine, which is why it’s often found by accident during routine blood tests.
Is subclinical hyperthyroidism dangerous if I feel fine?
Yes, it can be-even if you feel fine. Studies show that people with TSH below 0.1 mIU/L have a significantly higher risk of atrial fibrillation and heart failure over time. The damage builds silently. Feeling well doesn’t mean your heart or bones are safe. That’s why monitoring and targeted treatment are critical, especially for those over 65 or with existing heart disease.
Should I get treated if my TSH is 0.3?
Not automatically. A TSH of 0.3 falls in the mild range (0.1-0.44). Treatment isn’t usually recommended unless you have symptoms like palpitations, an irregular heartbeat, osteoporosis, or are over 65. If you’re young and healthy with no other risks, your doctor will likely just monitor you with annual blood tests. But if you have heart disease or a history of fractures, treatment may still be advised.
Can thyroid medication cause subclinical hyperthyroidism?
Yes, it’s one of the most common causes. People taking levothyroxine for hypothyroidism can accidentally take too much, especially as they age or if their metabolism changes. This is called exogenous subclinical hyperthyroidism. If your TSH is low and you’re on thyroid medication, your dose may need to be lowered. Always check with your doctor before making any changes.
How often should I get my TSH checked?
If your TSH is below 0.1, get tested every 3 to 6 months. If it’s between 0.1 and 0.44 and you have no symptoms or risk factors, once a year is usually enough. If you’re on thyroid medication, check every 6 months regardless. Regular monitoring is the best way to catch changes early and avoid complications.
What Comes Next?
If you’re being monitored for subclinical hyperthyroidism, your next step is simple: stay consistent. Keep your appointments. Track your symptoms-even small ones like a faster heartbeat after climbing stairs. Bring your latest lab results to every visit. Ask if you need an ECG or bone scan.
If you’ve been told to wait, don’t ignore it. Set a calendar reminder. Don’t assume everything’s fine just because you feel okay. This condition doesn’t announce itself with a bang-it creeps in. And by the time symptoms show up, the damage might already be done.
And if you’re considering treatment-whether it’s adjusting your medication, taking a beta-blocker, or going for radioactive iodine-talk through the trade-offs. What are you gaining? What are you risking? There’s no perfect answer. But there’s a right one for you.




January 26, 2026 AT 12:31
Man i just found out my TSH was 0.28 last year and i thought i was fine 😅
Turns out i was on a little too much levothyroxine from my hypothyroid treatment
My doc lowered my dose and now i feel like a new person no more heart flutters at 3am
Thyroid stuff is wild because you feel normal but your body is screaming in the background