Antibiotics in COPD — When and Which to Use
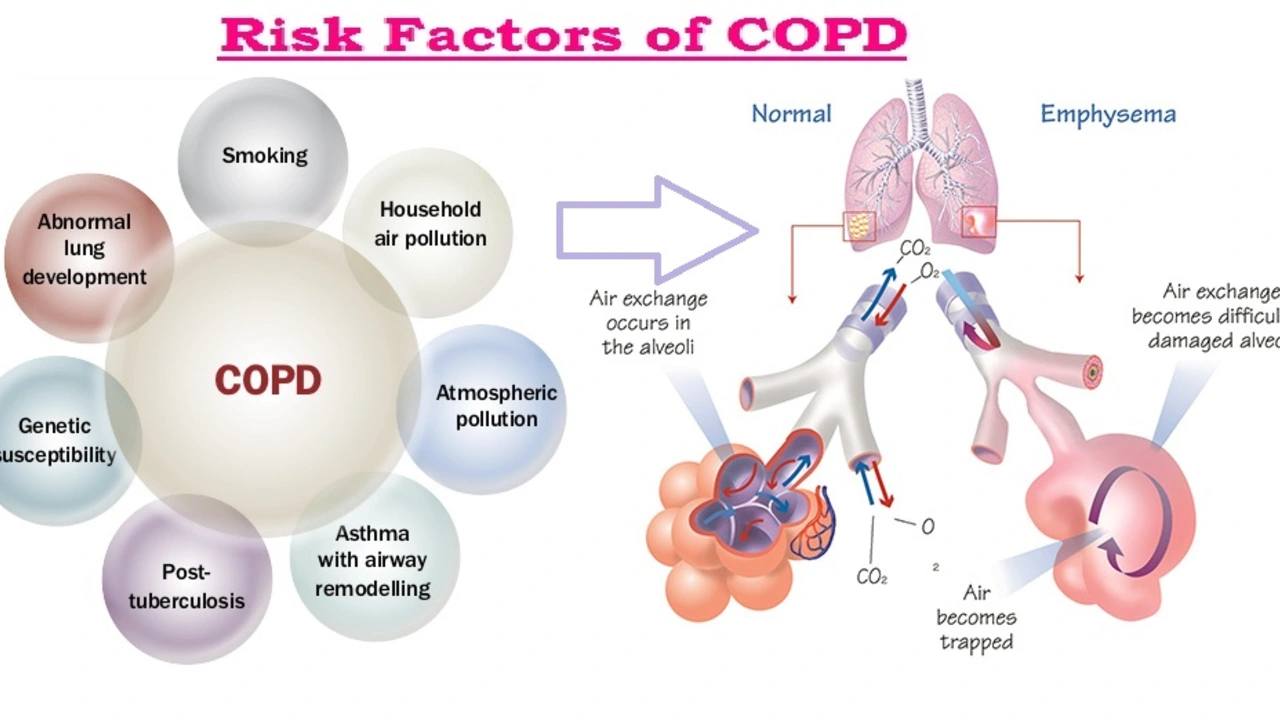
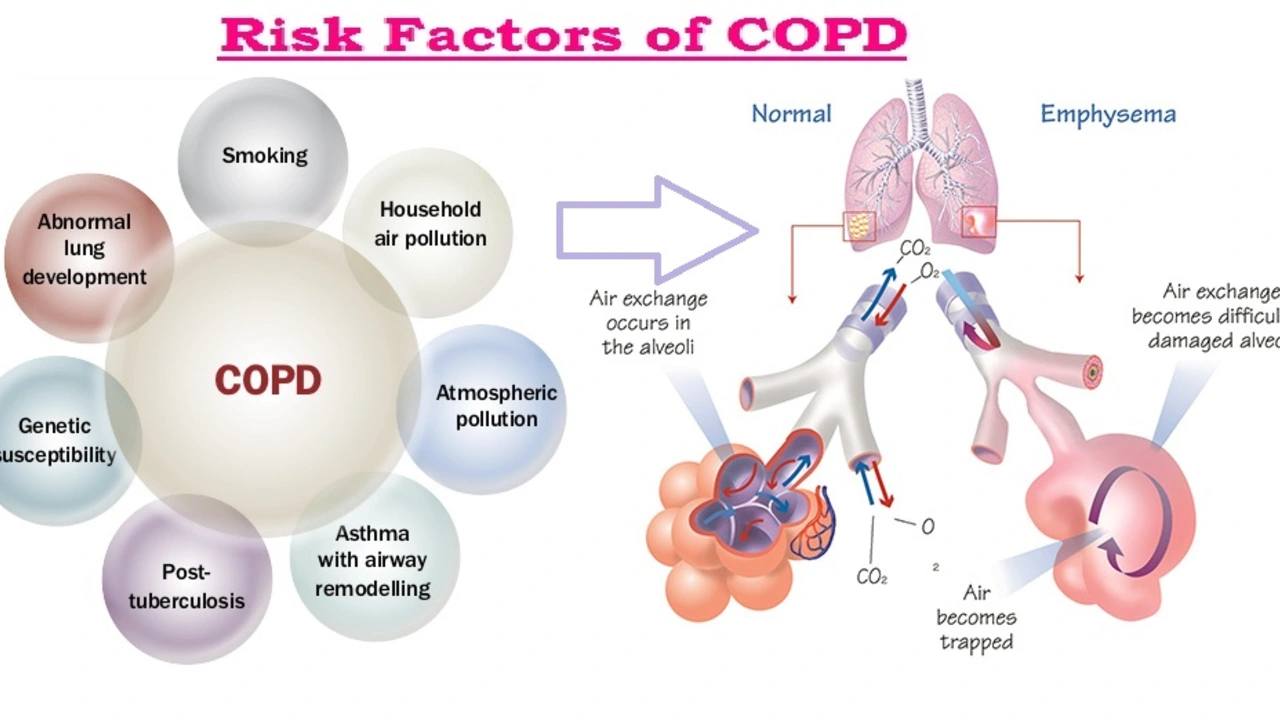
Having COPD means your lungs can flare up. Not every flare needs antibiotics. This page helps you decide when antibiotics make sense, which drugs doctors commonly use, and what to watch for.
Antibiotics are for bacterial exacerbations. Doctors look for increased breathlessness, more sputum, and a change in sputum color — the classic signs. Many clinicians use the Anthonisen criteria: if sputum purulence is present with either increased volume or worsening breathlessness, antibiotics are likely helpful. Mild viral or non-infectious flares usually do not need them.
For mild outpatient exacerbations, common choices include amoxicillin (or amoxicillin-clavulanate), doxycycline, or a macrolide like azithromycin. These cover typical bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Most courses last 5 to 7 days. Short courses often work as well as longer ones and lower side effects.
When to cover Pseudomonas and other resistant bugs
People with severe COPD, recent hospital stays, frequent antibiotics, or bronchiectasis may need broader coverage. Pseudomonas risk is higher in patients with very low FEV1, multiple exacerbations, or prior culture showing Pseudomonas. In those cases, doctors order sputum cultures and choose drugs active against gram-negative organisms. Hospitalized patients or those needing ICU care often get IV antibiotics tailored to cultures.
Macrolides have another role: long-term low-dose azithromycin can cut exacerbation frequency in selected patients. But long-term use brings risks: antibiotic resistance, hearing loss, and heart rhythm changes. Your doctor will weigh benefits and monitor you if this is an option.
Practical tips and safety
Get a sputum culture if you have severe disease, frequent flares, or recent antibiotic use. Finish the prescribed course unless your doctor tells you otherwise. Watch for side effects: diarrhea, yeast infections, tendon pain with some drugs, or dizziness. If you have heart disease, certain antibiotics can affect heart rhythm — mention this to your clinician.
Antibiotic stewardship matters. Overuse drives resistance and makes future infections harder to treat. That’s why doctors try to be selective: use antibiotics when signs point to bacterial infection, pick the narrowest effective drug, and limit duration. Vaccines, inhaled therapies, and pulmonary rehab reduce flare risk and lower antibiotic need.
If symptoms rapidly worsen, you have high fever, confusion, or you can't speak full sentences, seek urgent care. For routine flares, call your clinician early — starting appropriate treatment quickly often prevents hospitalization. Clear communication with your healthcare team and keeping records of previous sputum cultures help guide the best antibiotic choice.
Tell your doctor about other medicines, liver or kidney problems, and allergies before taking antibiotics. Some drugs interact — macrolides and fluoroquinolones can affect heart rhythm or boost side effects when mixed with certain heart or cholesterol drugs. Fluoroquinolones also raise tendon injury risk, especially in older adults. Simple self-care helps too: use your inhalers correctly, stay hydrated, rest, and avoid smoking. Keep a written list of past antibiotic responses to show your clinician; it speeds up the right choice next time. Ask questions if you're unsure about treatment.
Hello there. Today, we'll be discussing the use of Lincomycin in managing Chronic Obstructive Pulmonary Disease (COPD). It's a fascinating subject as this antibiotic brings new perspectives in managing this lung condition. We'll cover how this medication works, what the recent studies are saying, and how it could be a game-changer in COPD management. This is critical information for COPD patients and healthcare providers alike. I hope you find this useful and insightful!