Biosimilars vs Generics: What’s the Real Difference?
When you hear biosimilars, highly similar versions of complex biologic drugs that are made from living cells and generics, exact copies of simple, chemically-made brand-name drugs, it’s easy to think they’re just two names for the same thing. But they’re not. Biologic drugs, medications made from living organisms like proteins or antibodies — think insulin, rheumatoid arthritis treatments, or cancer therapies — are too complex to copy exactly. That’s why biosimilars aren’t called generics. They’re designed to be highly similar, with no meaningful difference in safety or effect, but they’re not identical. Generics, on the other hand, are exact chemical duplicates of small-molecule drugs like metformin or lisinopril. The difference isn’t just technical — it’s about how they’re made, tested, and approved.
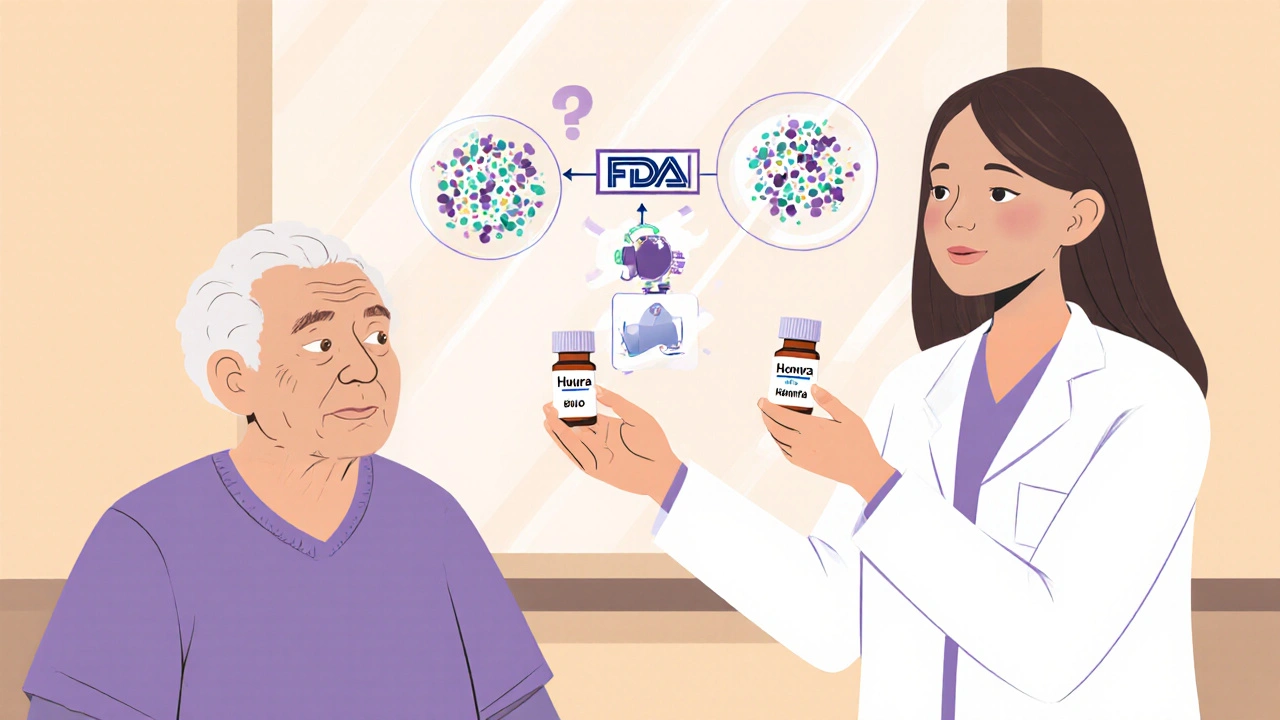
Here’s why it matters: if you’re on a biologic for something like Crohn’s disease or psoriasis, switching to a biosimilar isn’t like switching from brand-name Advil to generic ibuprofen. Biosimilars require way more testing than generics. While generics just need to prove they release the same amount of active ingredient into the bloodstream (bioequivalence), biosimilars must show they behave almost identically in the body — including how they bind to targets, how long they last, and how your immune system reacts. That’s why the FDA requires clinical trials for biosimilars, but not for generics. You can’t just swap one for the other without understanding the science behind it. And that’s where posts like Partial AUC: Advanced Bioequivalence Measurements Explained come in — they break down the exact methods used to prove these drugs work the same way, even when traditional measures fall short.
What you’ll find below is a collection of real, practical guides that connect the dots between drug approval, safety, and patient outcomes. You’ll see how bioequivalence testing works in the real world, how drug labels change when you switch from brand to copy, and why some patients need extra monitoring when moving to a biosimilar. These aren’t theory pieces — they’re written for people who need to make smart choices about their meds, whether they’re a patient, caregiver, or healthcare worker. From how pharmacists handle prescription transfers to how kidney function is tracked with supplements like creatine, the posts here show you the hidden rules behind drug safety. You’ll learn what’s truly interchangeable, what’s not, and why the difference between a biosimilar and a generic can change your treatment plan.
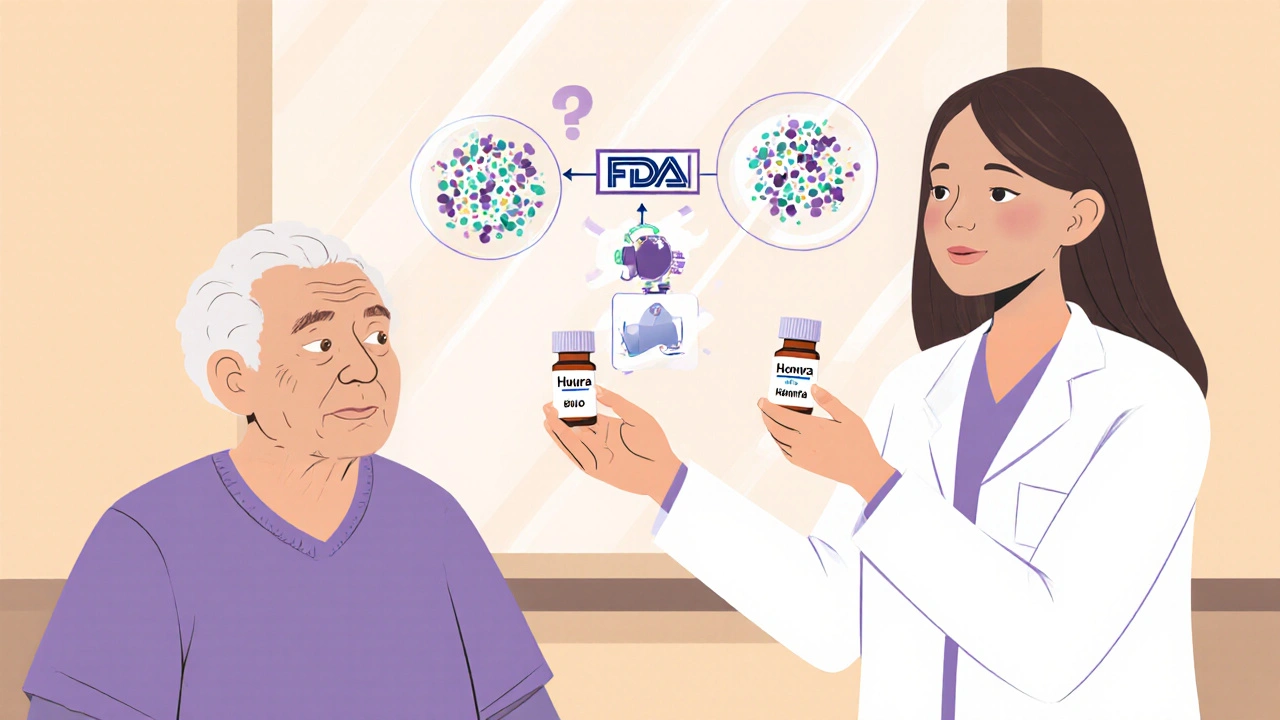
Pharmacists play a vital role in biosimilar adoption by counseling patients, ensuring safe substitution, and overcoming prescriber resistance. Unlike generics, biosimilars require specialized knowledge and careful communication to build trust and improve access to affordable biologic treatments.