Chemotherapy Drugs: How They Work, Side Effects, and What to Expect
When you hear chemotherapy drugs, powerful medications designed to kill rapidly dividing cancer cells. Also known as cytotoxic drugs, they’re one of the most common tools doctors use to treat cancer—but they don’t just target tumors. These drugs affect healthy cells too, which is why side effects like fatigue, nausea, and hair loss are so common. Not all chemotherapy is the same. Some are given alone, others in combinations, and sometimes they’re paired with radiation or immunotherapy. The goal isn’t always to cure—it’s often to shrink tumors, slow growth, or make other treatments work better.
One key concept you’ll see across many cancer treatments is combination therapy, using lower doses of multiple drugs to improve results while reducing harm. This approach shows up in chemotherapy drugs too. Instead of hitting the body with one high-dose drug, doctors often mix two or three with different mechanisms. That way, cancer cells have a harder time resisting treatment. It’s why you’ll hear about regimens like FOLFOX or CHOP—they’re not random lists, they’re carefully balanced formulas. And because these drugs can damage bone marrow, kidneys, or nerves, monitoring is part of the process. Blood counts, liver tests, and even hearing checks might be part of your routine.
Side effects aren’t the same for everyone. Some people feel fine for weeks; others struggle with vomiting or numb hands after just one cycle. Why? It depends on the drug, your age, your overall health, and how your body breaks down the medication. For example, some chemotherapy drugs, like those metabolized by the CYP450 enzyme system. can interact with grapefruit, certain antibiotics, or even over-the-counter painkillers. That’s why it’s so important to tell your oncologist everything you’re taking—even supplements or herbal teas. A drug interaction might not just make you feel worse—it could lower the drug’s effectiveness or increase toxicity.
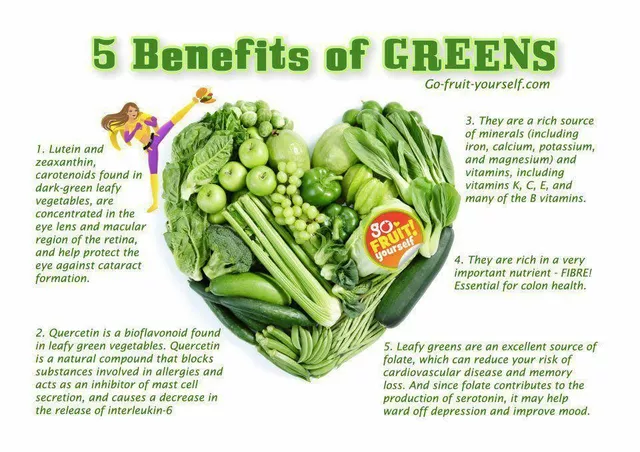
There’s also growing focus on what comes after chemotherapy. Many patients wonder if there are alternatives. While chemo remains a backbone of cancer care, newer options like targeted therapies and immunotherapies are changing the game. They’re not replacements for everyone, but they often come with fewer side effects. Some patients even use supportive care strategies—like managing nausea with proven remedies or protecting nerves with specific supplements—to make treatment more tolerable. It’s not about avoiding chemo, but about making it work better for you.
What you’ll find in the posts below isn’t just a list of drugs. It’s real-world insight into how these treatments affect daily life. From how to handle diarrhea after chemo, to why some people can’t tolerate certain drugs, to how dose adjustments can make a difference—you’ll see how people navigate the messy, complicated reality of cancer treatment. These aren’t textbook definitions. They’re stories from patients and doctors who’ve been there. And they might help you ask the right questions next time you sit down with your care team.
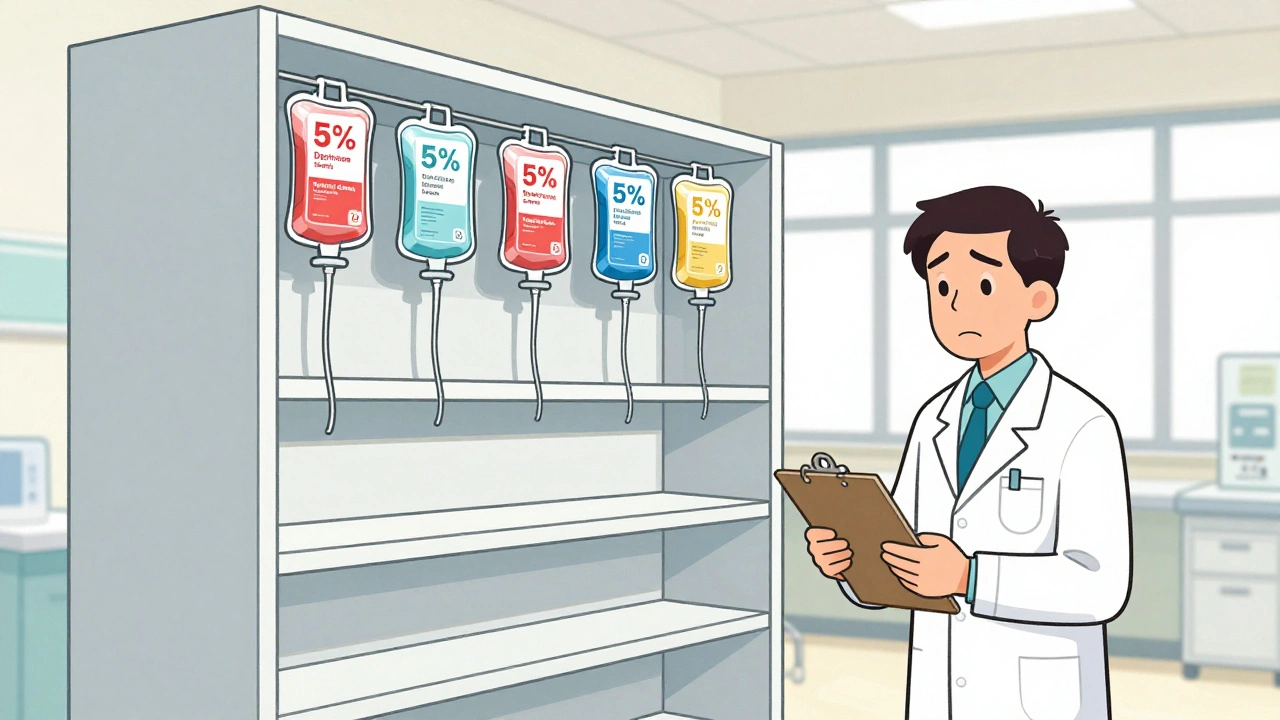
As of 2025, over 270 medications remain in short supply in the U.S., including critical chemotherapy drugs, IV fluids, and antibiotics. Learn which drugs are hardest to find, why shortages persist, and how patients and providers are coping.