COPD management: practical steps to breathe easier
COPD can feel overwhelming, but small, consistent actions make a big difference. This page gives clear, usable steps you can use today: how medicines help, what to do during flare-ups, daily habits that help your lungs, and when to ask for medical help.
Quick medication guide
Bronchodilators are the backbone of COPD treatment. Short-acting inhalers (like albuterol or ipratropium) relieve sudden breathlessness. Long-acting bronchodilators (LABA or LAMA such as salmeterol or tiotropium) reduce daily symptoms and cut flare-ups. Some people also need an inhaled steroid (ICS) added to a LABA for frequent exacerbations. Use the inhaler technique your clinician shows you — poor technique makes even the best drug useless. If you have a spacer, clean it regularly and replace as advised.
Keep a rescue inhaler within reach and refill prescriptions before they run out. If you’re starting or stopping any COPD drug, talk to your doctor about side effects and drug interactions — especially if you take medicines for heart disease or anxiety.
Daily habits and lifestyle that help
Quit smoking. It’s the single best move for slowing lung decline. Ask your doctor about nicotine replacement, varenicline, or bupropion — all increase your chance of success. Vaccines matter: get a yearly flu shot and follow advice on pneumococcal vaccines.
Pulmonary rehab helps more than you expect. It combines exercise, breathing training (pursed-lip and diaphragm breathing), education, and support. Even a short program improves walking distance, reduces breathlessness, and lifts mood. Keep a balanced diet — aim for enough protein and calories if you’re losing weight, or a plan to move safely if you’re carrying extra pounds.
Track symptoms. Note any increase in breathlessness, change in sputum color or amount, new fever, or swelling in legs. These are early warning signs of an exacerbation. Have a simple action plan written with your clinician: which inhalers to use, when to start steroids or antibiotics, and when to call for urgent care.
Home oxygen helps those with low oxygen levels. If your resting SpO2 is often below 88% or blood tests show low oxygen, your doctor may refer you for long-term oxygen therapy. Practice oxygen safety: no smoking near equipment and proper storage of tanks.
Know when to seek help. Go to the emergency room if you can’t speak in full sentences, your lips or face turn blue, you feel dizzy or faint, or breathing gets rapidly worse. Call your healthcare team for increased cough, fever, or sputum changes — early treatment often prevents hospital stays.
Work with your team. Regular spirometry, medication reviews, and a written action plan keep COPD stable. Small daily changes add up: correct inhaler use, staying active, avoiding infections, and quick action for flare-ups will help you breathe easier and stay out of hospital.
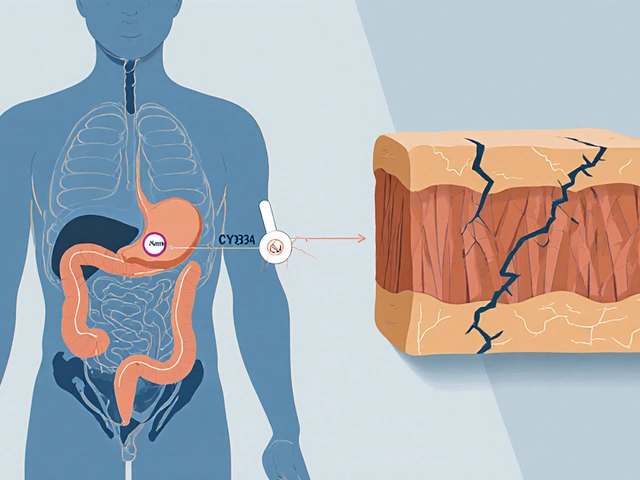
Hello there. Today, we'll be discussing the use of Lincomycin in managing Chronic Obstructive Pulmonary Disease (COPD). It's a fascinating subject as this antibiotic brings new perspectives in managing this lung condition. We'll cover how this medication works, what the recent studies are saying, and how it could be a game-changer in COPD management. This is critical information for COPD patients and healthcare providers alike. I hope you find this useful and insightful!