IBS: Practical Ways to Manage Irritable Bowel Syndrome
IBS can feel unpredictable: one day you're fine, the next day you’re doubled over or running to the bathroom. You don’t need a miracle—small, consistent changes often cut symptoms a lot. Here are straightforward steps you can try today to feel better and take control.
What to watch for and quick self-help steps
Know your pattern. IBS usually shows up as abdominal pain with changes in bowel habits: diarrhea (IBS-D), constipation (IBS-C), or both (IBS-M). Start a simple food and symptom diary for 2–4 weeks—note what you eat, stress level, and symptoms. That tells you which foods or situations trigger flares.
Try small habits first: eat regular meals, chew slowly, drink enough water, and move a bit each day. Avoid large meals, smoking, and excess caffeine or alcohol. For constipation, add fiber gradually (psyllium is gentle). For diarrhea, avoid high-fat meals and limit caffeine and sugar alcohols like sorbitol and xylitol.
Diet, supplements, and useful treatments
Low FODMAP diet helps many people with IBS. It’s a three-step approach: restrict high-FODMAP foods, reintroduce them one at a time, then personalize your long-term diet. Work with a dietitian if you can—this prevents unnecessary restrictions.
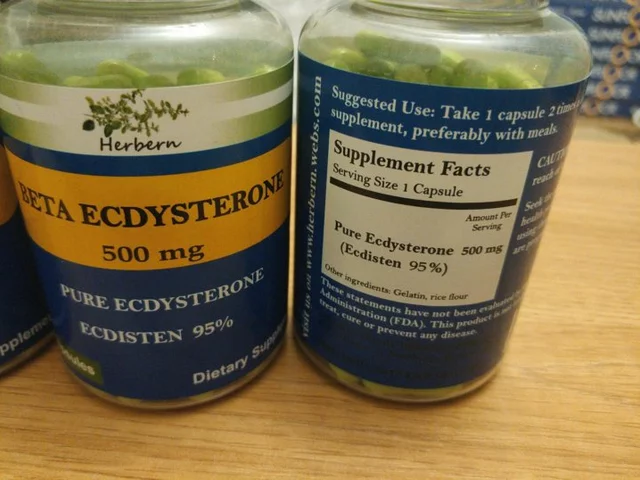
Probiotics can help, but effects vary. Look for products with Bifidobacterium or Lactobacillus strains and try one for 4–8 weeks to judge benefit. For bloating, peppermint oil capsules (enteric-coated) often reduce cramps and gas.
Medications have a role when lifestyle changes aren’t enough. Over-the-counter loperamide can control diarrhea; osmotic laxatives or polyethylene glycol help constipation. Your doctor may prescribe antispasmodics for cramping, low-dose tricyclic antidepressants for pain, or newer options like rifaximin for IBS-D. Always check with a clinician before starting meds.
Mood matters. Stress, anxiety, and sleep issues make IBS worse. Gut-directed therapies—CBT, mindfulness, and hypnotherapy—show real benefit for many people. Even simple tools like a short daily walk, breathing exercises, or a sleep routine help.
When to see a doctor
Talk to a clinician if you have unintentional weight loss, blood in stool, fever, persistent severe pain, or new symptoms after age 50. These are red flags that need tests to rule out other conditions. Also see a doctor if your symptoms stop you from working or living normally—there are effective treatments beyond self-care.
IBS is common and manageable. Track your triggers, try a low-FODMAP approach with guidance, consider targeted supplements or meds, and address stress. Small, steady steps usually pay off. If things don’t improve, get medical help—there are treatments that can really reduce symptoms and get you back to normal life.

In my recent investigations into Irritable Bowel Syndrome (IBS) treatments, I discovered an interesting role that Ranitidine might play. Apparently, this medication, typically used to reduce stomach acid, has the potential to alleviate some IBS symptoms. While it's not a cure-all, it could provide some much-needed relief for those grappling with this chronic condition. However, more research is necessary to fully understand this connection. Always consult with a healthcare provider before starting any new treatment.