Living with chronic pain isn’t just about hurting every day-it’s about learning how to live anyway. For 50 million Americans, pain doesn’t go away after an injury heals. It sticks around, reshaping sleep, work, relationships, and even identity. The old model-pop a pill, hope it works, repeat-has failed too many people. Today’s science says something different: chronic pain management isn’t about erasing pain. It’s about rebuilding your life around it.
Why Pain Stays Long After the Injury Heals
Pain isn’t just a signal from your body. It’s a complex experience shaped by your nervous system, emotions, stress levels, and even your environment. When pain lasts longer than three months, your brain and nerves can get stuck in a loop. The original injury might be gone, but your body keeps sounding the alarm. This isn’t in your head-it’s in your nerves. And it’s real.That’s why treating chronic pain like an acute injury doesn’t work. You can’t just give someone more opioids and expect them to get better. Studies show that after six months, opioids stop helping much. The risk of dependence, overdose, and side effects keeps climbing, but the pain relief doesn’t. The CDC’s 2022 guidelines made this clear: opioids should be a last resort, not the first step.
The New Standard: Non-Drug Treatments First
The most effective approach today starts with what doesn’t involve pills. The World Health Organization’s 2023 guidelines put it bluntly: drug-free approaches are front and center.Structured exercise is the most proven starting point. Not just walking. Not just stretching. But programs designed specifically for chronic pain: aerobic training, strength work, water-based exercises, tai chi, and yoga. These aren’t optional hobbies-they’re medical treatments. A 12-week program done two to three times a week can reduce pain by 15-30% and improve daily function by 20-40%. People who stick with it report being able to play with their kids, go back to part-time work, or simply get out of bed without dreading the day.
Cognitive Behavioral Therapy (CBT) is another cornerstone. It doesn’t mean “thinking positive.” It means learning how your thoughts, emotions, and behaviors feed into your pain experience. In 8 to 12 weekly sessions, patients learn to recognize pain triggers, manage catastrophizing thoughts (“I’ll never get better”), and pace their activity to avoid flare-ups. Studies show CBT cuts pain intensity by 25-40%, reduces disability by 30%, and cuts pain-related anxiety by nearly half. One veteran went from taking 120 mg of morphine equivalents daily to just 30 mg-while doing more, not less.
When You Need More Than One Approach
For many, one treatment isn’t enough. That’s where multidisciplinary pain rehabilitation comes in. These programs-like the one at Mayo Clinic-bring together doctors, psychologists, physical therapists, occupational therapists, and pharmacists. Over three intense weeks, patients learn how to move without fear, manage stress, regulate sleep, and use biofeedback to calm their nervous system.The results? Sixty to seventy-five percent of participants see major improvements in daily function. Half to two-thirds reduce or stop using opioids. And 85% say the program was “very helpful” or “extremely helpful.” This isn’t magic. It’s coordinated care. But here’s the catch: only 15-20% of people who need these programs can actually get them. They’re expensive-$15,000 to $20,000 per patient-and mostly located in big cities. Insurance often won’t cover them, even though the guidelines say they should.

What Medications Actually Work (And What Don’t)
Medications still have a role-but only after non-drug options have been tried. And not all painkillers are created equal.Acetaminophen and NSAIDs like ibuprofen or naproxen are first-line for many. But they’re not for everyone. People with kidney issues, stomach ulcers, or heart disease need to be careful. Then there are co-analgesics-drugs not originally designed for pain but proven to help. Duloxetine (60-120 mg/day) and pregabalin (150-600 mg/day) are commonly used for nerve pain, fibromyalgia, and chronic back pain. They don’t eliminate pain, but they make it more manageable.
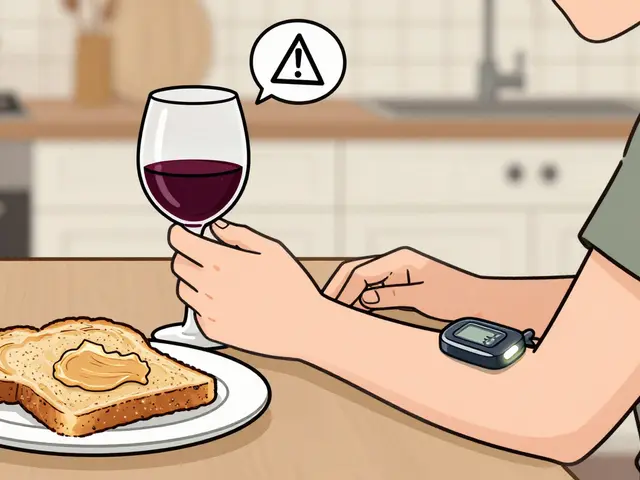
Opioids? They’re not banned. But they’re tightly controlled. The CDC says if you use them, start low (under 50 morphine milligram equivalents per day), monitor monthly, and only use them if other treatments failed. Even then, the benefits fade after six months. The risk doesn’t. A dose over 50 MME/day increases overdose risk by 40%. And once you’re on them, getting off is hard.
Barriers No One Talks About
Here’s the uncomfortable truth: the best treatments aren’t available to most people.Two-thirds of chronic pain patients say they can’t find providers who know how to deliver non-opioid care. One Reddit user wrote: “My doctor only offered opioids or nothing.” A 2022 study found only 35% of primary care doctors had received proper training in evidence-based pain management. Meanwhile, insurance companies routinely deny coverage for CBT, physical therapy, or acupuncture-even when guidelines say they’re first-line.
Financial and racial disparities are stark. Black patients are 40% less likely to receive recommended non-drug treatments, even when their pain levels are the same as white patients. Rural areas are worse off: 65% of counties have no pain specialist at all. And for people on fixed incomes, a $100-per-session therapy or a $200 yoga class isn’t an option.

What’s Changing-and What’s Not
There’s progress. Medicare now covers more non-drug treatments. The VA has built out multidisciplinary programs in 92% of its facilities. The NIH has poured $1.8 billion into developing non-addictive pain treatments, with 37 new non-opioid drugs in clinical trials. Digital tools like FDA-cleared apps and wearable nerve stimulators are showing promise, with 30-40% pain reduction in trials.But the gap between what we know works and what people actually get is still huge. A 2019 federal report found that 60-70% of chronic pain patients never receive guideline-concordant care. The problem isn’t lack of science. It’s lack of access, lack of training, and lack of will.
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Start here:- Track your pain-use the Brief Pain Inventory or a simple journal. Note what makes it better or worse.
- Move gently, consistently-start with 10 minutes of walking or water aerobics three times a week. Don’t wait for pain to disappear to start.
- Ask for CBT-tell your doctor you want a referral to a psychologist trained in chronic pain. It’s not “mental health treatment”-it’s pain treatment.
- Challenge opioid prescriptions-if you’ve been on them for more than three months, ask: “Is this still helping me function?”
- Find your people-online communities like r/ChronicPain or local support groups help you feel less alone. You’re not broken. You’re adapting.
Chronic pain doesn’t have to be your whole story. It can be one part of your life-not the only part. The goal isn’t to be pain-free. It’s to be alive, active, and in control-even when the pain is there.
Is chronic pain just in my head?
No. Chronic pain is a real physical change in your nervous system. It’s not imaginary, but it’s also not just a signal from your body. Your brain learns to interpret normal sensations as painful, even when there’s no tissue damage. This is called central sensitization. It’s measurable in brain scans and responds to treatments like CBT and exercise-not just pills.
Can I ever stop taking pain meds?
Many people can. Studies show that with structured exercise, CBT, and pain education, up to 65% of patients reduce or eliminate opioid use. It’s not about quitting cold turkey-it’s about building new skills so you don’t need them. Work with a pain specialist to taper safely. The goal isn’t to be medication-free at all costs. It’s to be functional with the least risk.
Why won’t my insurance cover CBT or physical therapy?
Insurance companies often see these as “alternative” or “optional,” even though guidelines from the CDC, WHO, and American College of Physicians say they’re first-line. Many policies still treat pain like an acute issue, not a chronic condition. Appeal denials with copies of the guidelines. Ask your doctor to write a letter of medical necessity. Some states now require coverage for these services-check your state’s health department website.
What’s the best exercise for chronic pain?
There’s no single “best” exercise-it’s about what you can do consistently. Water-based exercise (aquatic therapy) is great for joint pain. Tai chi and yoga improve balance and reduce stress. Strength training builds muscle to support sore joints. Walking is simple and effective. The key is consistency, not intensity. Start slow. Do it three times a week. Even 10 minutes helps. A physical therapist trained in chronic pain can design a program that fits your limits.
How do I find a good pain specialist?
Look for someone who practices multidisciplinary care-meaning they work with psychologists, PTs, and occupational therapists. Avoid providers who only offer injections or prescribe opioids. Check if they’re certified by the American Board of Pain Medicine. Ask if they use tools like the Brief Pain Inventory and follow CDC or WHO guidelines. The American Chronic Pain Association and the VA’s pain program locator can help you find qualified providers near you.
Is acupuncture worth trying?
It can be. For conditions like osteoarthritis of the knee or chronic low back pain, acupuncture shows 20-30% better pain relief than fake treatments. But it doesn’t work well for nerve pain like diabetic neuropathy. It’s not a cure, but it can be a useful tool when combined with exercise and CBT. Make sure your acupuncturist is licensed. Most insurance still won’t cover it, but some plans are starting to.
Can chronic pain ever go away completely?
For some, yes-but not always. For most, the goal isn’t total elimination. It’s reducing pain enough to live fully. Many people learn to manage pain so well they forget it’s there most of the time. They return to work, travel, or play with grandchildren. That’s success. Focusing only on pain elimination often leads to frustration. Focusing on function-moving, sleeping, connecting-leads to real improvement.






December 2, 2025 AT 22:47
Chronic pain ain't just a symptom-it's a full-time job you never applied for. The nervous system gets rewired like a faulty circuit board and suddenly your body's screaming at you for no reason. I've been on the other side of this and yeah, opioids helped at first but then they just made me feel like a zombie with a side of constipation. CBT? Surprisingly life-changing. Learned to separate the pain from the panic. Not cured, but now I can play with my niece without dreading the next 48 hours.