What Psoriasis Really Is - And Why It’s More Than Just a Skin Problem
Psoriasis isn’t just flaky, red patches on your skin. It’s a full-body immune disorder. Your body’s immune system mistakenly attacks healthy skin cells, causing them to multiply too fast. Instead of shedding naturally over weeks, they pile up in days, forming thick plaques. This isn’t contagious. It’s not caused by poor hygiene. It’s genetic, triggered by stress, infections, or even certain medications. And it doesn’t stop at the skin.
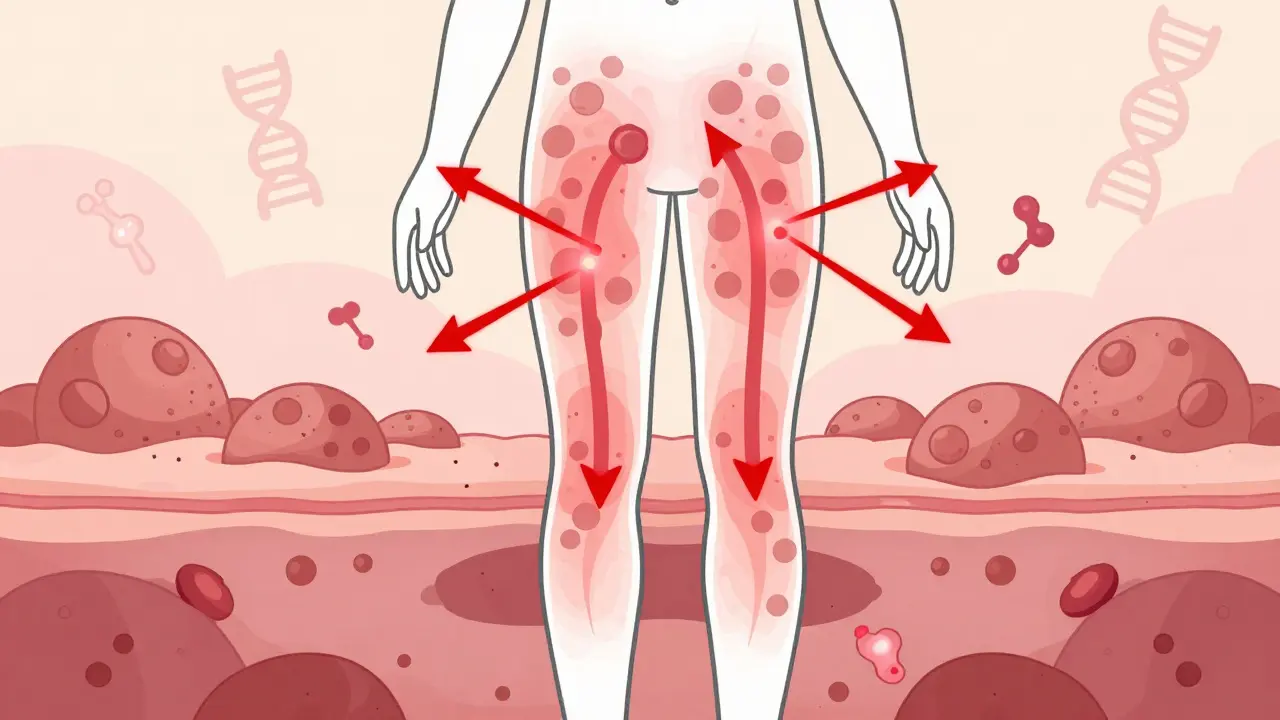
Up to 30% of people with psoriasis develop psoriatic arthritis - joint pain, stiffness, swelling. Nearly half have metabolic syndrome. Heart disease risk jumps by 26%. This isn’t cosmetic. It’s systemic. And for many, it’s been misunderstood for decades.
Plaque Psoriasis: The Most Common Form - And How to Treat It
Eight out of ten people with psoriasis have plaque psoriasis. Thick, silvery scales on elbows, knees, scalp, lower back. It’s the version most people picture. But treating it isn’t one-size-fits-all.
For mild cases - less than 5% of body surface - topical treatments still work well. Corticosteroid creams reduce inflammation fast. But long-term use can thin the skin. That’s why doctors pair them with calcipotriol, a vitamin D analog that slows skin cell growth. Together, they clear plaques in 35-40% of people within eight weeks.
Newer topicals like tapinarof cream (1%) are changing the game. In clinical trials, it cleared 35% of plaques at 12 weeks with fewer side effects than steroids. It’s applied once daily. No burning. No thinning. Just steady improvement.
But if plaques cover more than 10% of your body, or they’re on your face, hands, or genitals? Topicals alone won’t cut it. That’s when you move to systemic treatments.
Guttate Psoriasis: Sudden Outbreaks After Infections
Guttate psoriasis hits fast. Small, teardrop-shaped red spots all over the torso, arms, legs. It often follows strep throat - especially in kids and young adults. It can look like a rash, but it’s psoriasis. And it’s often triggered by an infection you thought was already gone.
Unlike plaque psoriasis, guttate doesn’t always stick around. For many, it clears on its own within weeks. But if it doesn’t? Treatment is similar to mild plaque psoriasis. Light therapy (narrowband UVB) works well here. So do gentle topicals. Antibiotics won’t help unless you still have an active strep infection.
But here’s the catch: if guttate doesn’t resolve, it can turn into chronic plaque psoriasis. That’s why early intervention matters. If you’ve had a bad sore throat and then your skin starts breaking out, see a dermatologist - don’t wait.
Systemic Treatments: When Topicals Aren’t Enough
If your psoriasis covers more than 10% of your skin, or it’s affecting your quality of life - sleep, work, relationships - it’s time to consider systemic therapy. These aren’t creams. They’re pills or injections that work inside your body.
Methotrexate has been used for decades. Taken once a week, it suppresses immune activity. About half of users get 75% skin clearance in 16 weeks. But it can affect the liver. Regular blood tests are mandatory.
Cyclosporine works faster - often in 4-8 weeks. It’s great for quick control, like before a big event. But it’s not for long-term use. Kidney damage is a real risk after six months.
Apremilast is an oral pill that’s easier on the body. Taken twice daily, it reduces inflammation without suppressing the whole immune system. About one-third of users hit PASI 75. It’s safe for people with liver or kidney issues, but nausea and diarrhea can be annoying at first.
Deucravacitinib is newer. A once-daily pill that targets a specific enzyme (TYK2). In trials, nearly 60% of users cleared 75% of their skin in four months. It’s becoming a go-to for people who want oral treatment without the side effects of older drugs.
Biologics: The Game-Changers in Psoriasis Care
Biologics are precision medicines. They don’t just dampen your immune system - they target specific parts of it. Think of them as sniper rifles instead of shotguns.
TNF inhibitors like adalimumab were the first biologics. They work well - about 78% of users hit 75% clearance. But they’re not the strongest anymore. And they increase infection risk, including tuberculosis.
IL-17 inhibitors like secukinumab are faster and stronger. They clear 80% of plaques in 16 weeks. Many patients report near-complete clearance. But they’re not ideal if you have Crohn’s disease or other bowel issues - they can make it worse.
IL-23 inhibitors - guselkumab, risankizumab, tildrakizumab - are now the gold standard. They target the root cause earlier in the inflammation chain. In trials, 84-90% of users achieved 90% skin clearance. That’s not just improvement. That’s near-total clearance. And they’re dosed every 8-12 weeks. Less frequent shots. Better adherence.
Real-world data from 31,521 patients shows risankizumab has the highest persistence rate - 78% of people stayed on it after a year. Guselkumab isn’t far behind. These aren’t just drugs. They’re life-changing.
Choosing the Right Treatment: It’s Personal
There’s no single best treatment. Your choice depends on your body, your life, and your goals.
If you want quick results and have no bowel disease? IL-17 inhibitors might be right. If you want long-term control with fewer shots? Go IL-23. If you hate needles? Deucravacitinib or apremilast could be your best bet.
Doctors now use tools like PASI (Psoriasis Area and Severity Index) and DLQI (Dermatology Life Quality Index) to measure how bad your psoriasis is - not just by looks, but by how it affects your daily life. If your DLQI is above 10, you’re a candidate for biologics. No need to suffer through ineffective topicals for months.
And here’s something most people don’t know: if you don’t respond to one biologic, it doesn’t mean they all won’t work. Your psoriasis might be driven by a different immune pathway. Some patients have a type I interferon signature - not the usual Th17 pathway. Those patients respond better to different drugs. Testing for this is still emerging, but it’s changing how we treat.
Cost, Access, and Real-World Challenges
Biologics cost a lot. Guselkumab runs about $34,200 a year. Adalimumab is $28,500. But here’s the reality: 85% of insured patients pay $0-$150 a month thanks to manufacturer assistance programs. Don’t assume you can’t afford it. Talk to your dermatologist’s office. They have specialists who help navigate this.
Insurance approval can take 4-6 weeks. That’s frustrating when you’re in pain. Many clinics now use electronic prior authorization systems - approval time dropped from two weeks to under a week. Ask your provider if they use one.
For people without insurance, patient assistance programs often provide free medication. Some pharmacies offer discount cards. And new oral drugs like deucravacitinib are becoming more affordable faster than injectables.
What’s Next? The Future of Psoriasis Treatment
The next wave is oral biologics - pills that work like injections. Early results from selective IL-23 receptor antagonists show 82% skin clearance. No needles. No weekly shots. Just a daily pill.
There’s also emerging hope for treatment cessation. In the GUIDE trial, patients who achieved complete clearance with guselkumab were taken off treatment. A third stayed clear for over a year. This isn’t a cure - but it might be a functional one. Imagine going years without treatment after just one year of therapy.
And for nail psoriasis? Intralesional steroid injections - tiny shots right into the nail bed - clear pitting and discoloration in 75% of cases. For scalp psoriasis? Foam formulations of calcipotriol and steroid mixtures work better than lotions. And for genital areas? Low-potency steroids with moisturizers are safer and just as effective.
What to Do If Your Treatment Stops Working
It happens. Maybe you started with methotrexate. Then adalimumab. Now nothing seems to work. Don’t give up. Don’t assume you’re treatment-resistant.
What you might need is a shift in strategy. If you failed a TNF inhibitor, try an IL-23 blocker. If you failed an IL-17 drug, try a TYK2 inhibitor like deucravacitinib. And if you’re not responding at all? Ask about endotype testing - it’s not mainstream yet, but it’s coming fast.
Also, check your lifestyle. Weight loss improves response to biologics. Smoking reduces effectiveness. Alcohol interferes with methotrexate. Stress triggers flares. Treating psoriasis isn’t just about drugs. It’s about your whole life.
Support and Resources You Can Use Today
You’re not alone. The National Psoriasis Foundation’s Biologics Navigator tool helps match you with treatments based on your profile. It’s free. It’s trusted. And it’s used by 87% of patients who try it.
Online communities like Reddit’s r/psoriasis have over 12,500 members sharing real experiences - what worked, what didn’t, how to handle insurance, how to talk to your doctor. Don’t underestimate peer support.
And if you’re struggling with the emotional toll - depression, shame, anxiety - ask for help. Psoriasis is linked to higher rates of depression. Your dermatologist can refer you to a counselor who understands chronic skin disease.




December 18, 2025 AT 17:45
This is the kind of article that makes me want to hug a dermatologist. 🤗 Finally, someone broke it down without the corporate fluff. Biologics aren't magic, but they're the closest thing we've got to turning psoriasis from a life-sentence into a manageable glitch. I went from hiding my arms in summer to wearing tank tops. No regrets.