When you hear about someone joining a cancer clinical trial, it’s easy to think it’s just about being sick and willing to try something new. But behind every trial is a strict, science-driven filter - one that’s changed dramatically in the last decade. Today, eligibility isn’t just about age, stage, or prior treatments. It’s about biomarkers. These are measurable signs in your body - like a gene mutation, protein level, or immune cell count - that tell doctors whether a drug is even likely to work for you. If you don’t have the right biomarker, you won’t qualify. And that’s not a flaw. It’s the future of cancer care.
What Exactly Are Biomarkers in Clinical Trials?
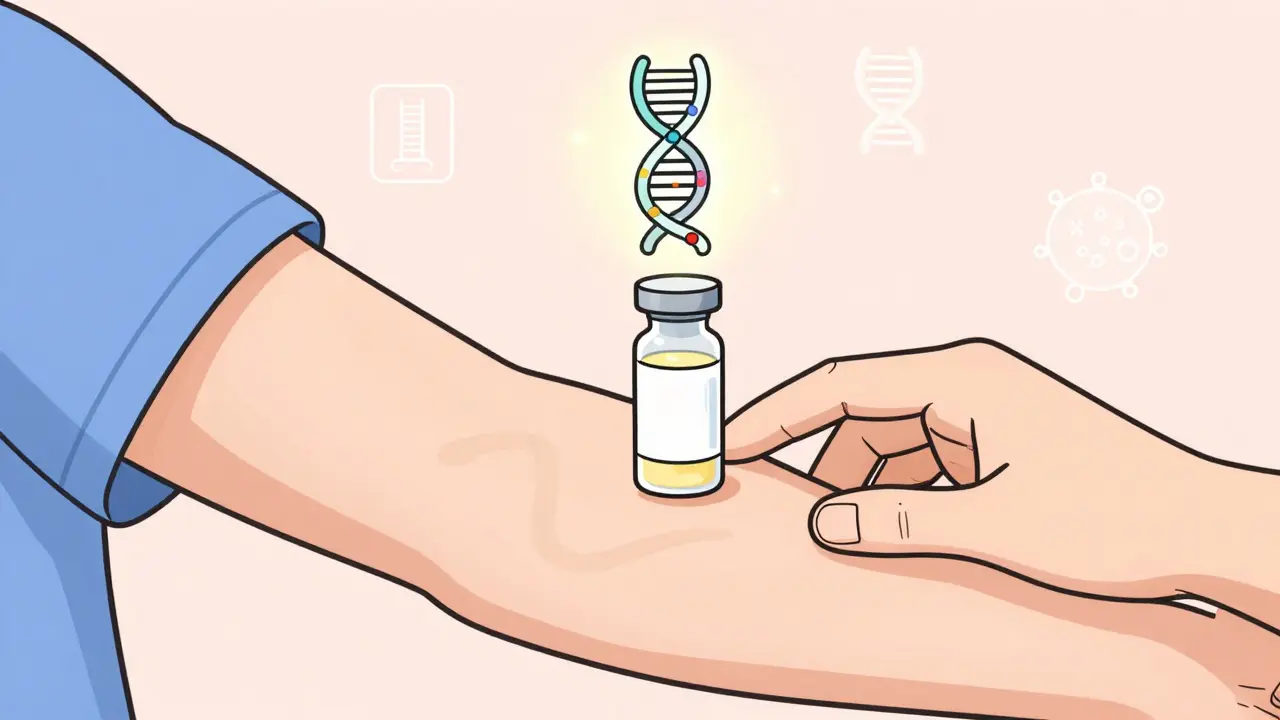
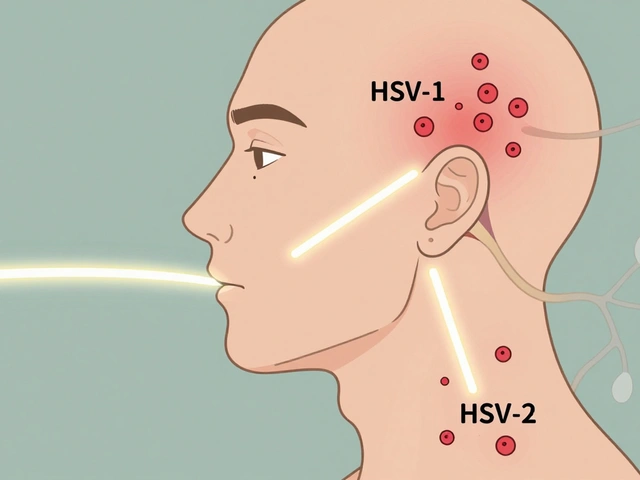
Biomarkers aren’t magic. They’re objective, testable signals from your body. The National Institutes of Health defined them back in 1998 as characteristics you can measure to show if something’s happening inside you - whether it’s disease, your body’s response to treatment, or your risk of developing cancer. Today, the FDA breaks them into seven types: diagnostic, prognostic, predictive, safety, and more. But for cancer trials, the most important one is the predictive biomarker. This tells you if a drug will work for you.
Take HER2 in breast cancer. Back in the 1990s, doctors gave chemotherapy to everyone with advanced breast cancer. Response rates? Around 12%. Then they found that patients with high HER2 levels responded dramatically better to drugs like trastuzumab. Today, if you don’t test positive for HER2, you won’t even be offered that drug in a trial. That’s the power of biomarkers: they turn guesswork into precision.
Now, nearly 73% of all oncology trials launched in 2022 used biomarkers to decide who could join. That’s up from just 41% in 2017. It’s not a trend - it’s the new standard.
How Biomarkers Change Who Gets Into a Trial
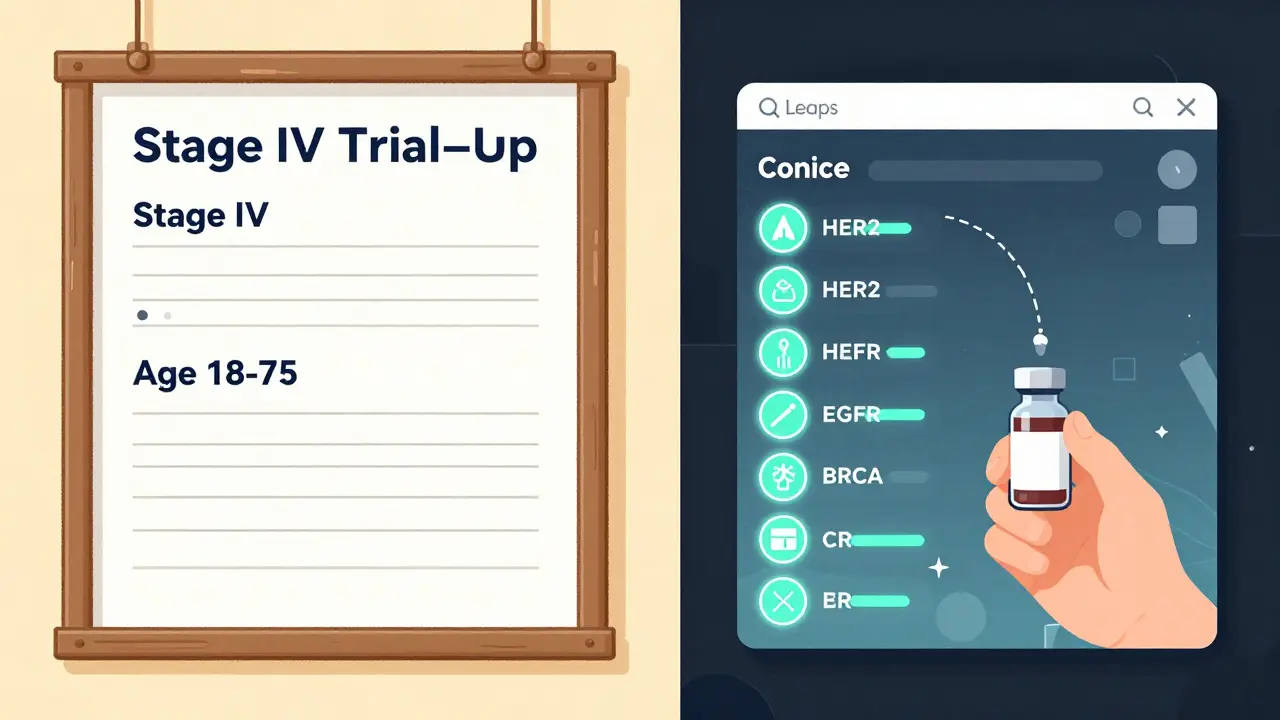
Traditional clinical trials used broad criteria: "Stage IV lung cancer, no prior chemo, age 18-75." But that meant throwing a wide net. Many patients got the drug, but it didn’t work - not because the drug was bad, but because their cancer didn’t match the target.
Biomarker-driven trials flip that. They say: "Only patients with EGFR exon 19 deletion get this drug." That sounds restrictive. But here’s the catch: it works better. A 2021 analysis of over 9,700 trials found that trials using biomarkers to select patients had a 49.8% success rate in Phase 2 - almost double the 26.9% of trials that didn’t use them. Why? Because you’re testing the drug on people who are biologically likely to respond. No more guessing.
Take the example of neratinib for HER2-mutant breast cancer. In unselected patients, response rates were 12%. In those selected by HER2 mutation? Jumped to 32%. That’s not a small gain. That’s life-changing.
But it’s not just about single genes. New trials now look at combinations - like having both a BRCA mutation and high tumor mutational burden. Or using a blood test to detect circulating tumor DNA. These are multi-layered filters, and they’re getting smarter every year.
The Hidden Challenges of Using Biomarkers
It sounds perfect, right? But there’s a downside. Getting a biomarker test isn’t like a routine blood draw. It often requires tissue from a biopsy - and not all hospitals can handle it. Some tests need special equipment, trained pathologists, or even shipping samples to a central lab. In one survey, 68% of clinical trial sites reported delays of 7 to 14 days just waiting for biomarker results. That means patients wait. And sometimes, their cancer progresses while they’re waiting.
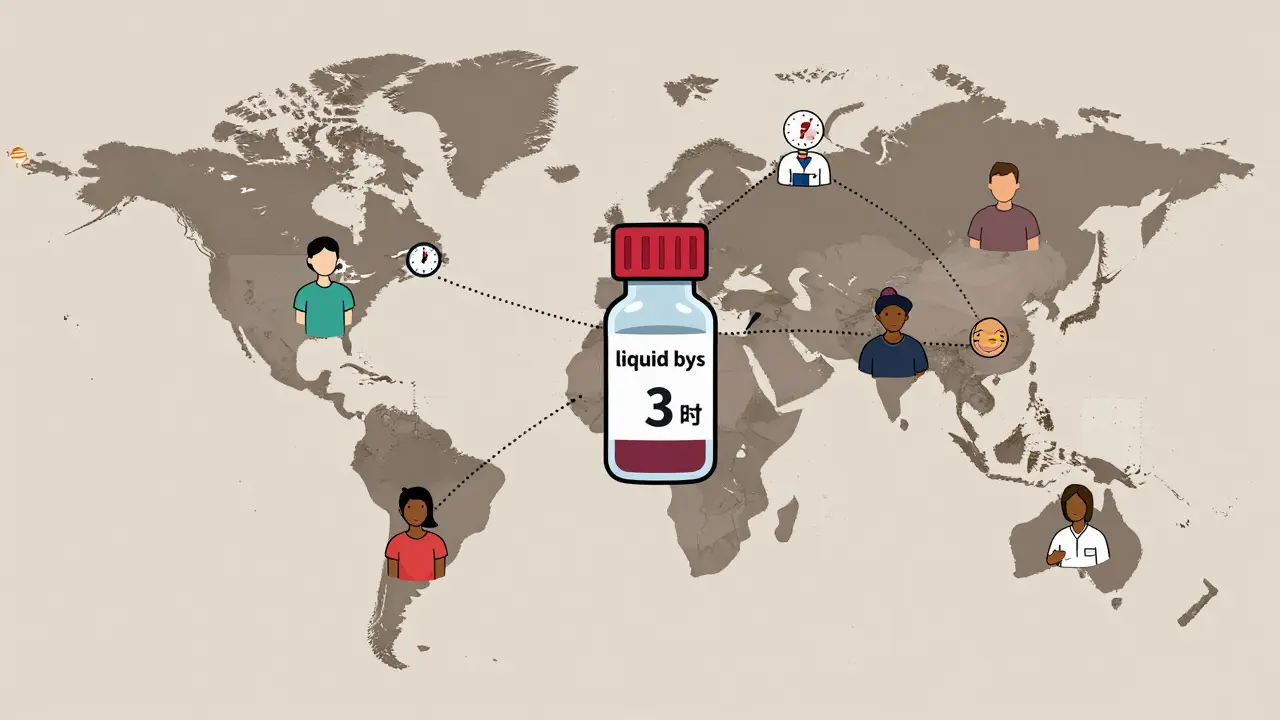
Then there’s geography. A biomarker common in Europe might be rare in Australia or parts of Asia. For example, the HLA-A*02:01 marker - critical for some cell therapies - shows up in over 50% of Europeans but under 20% in some Asian populations. That means a trial designed in the U.S. might fail to enroll enough patients in Southeast Asia. Sites have to adjust. Some now run separate eligibility criteria by region. Others use centralized testing labs to standardize results.
And training? Huge gap. A 2022 survey found 76% of research coordinators felt undertrained on how to collect and handle biomarker samples. One wrong step - like leaving a blood tube in a warm room too long - can ruin the test. You can have the perfect biomarker, but if the sample is degraded, you’re out of the trial.
How Trials Are Solving These Problems
Industry isn’t ignoring these issues. The smartest trials now build solutions into their design.
- Centralized testing labs - used in 63% of Phase 3 trials - ensure every sample is processed the same way, no matter where it comes from.
- Standardized kits - 78% of sponsors now provide pre-packaged collection kits with clear instructions, temperature controls, and shipping labels.
- Real-time data dashboards - 55% of big pharma companies monitor biomarker results live, so they can spot delays before they derail enrollment.
- Liquid biopsies - blood tests that detect tumor DNA - are now used in 31% of Phase 2+ cancer trials. That cuts out invasive biopsies and speeds up results to just 3-5 days.
Even the FDA has stepped in. In 2023, they streamlined their biomarker qualification process, cutting review times from 24 months to 18. They’re also pushing for "Context of Use" statements - clear documents that say exactly how a biomarker will be used in a trial, what data supports it, and how it’s measured. No more ambiguity.
What This Means for Patients
If you’re considering a clinical trial today, here’s what you need to know:
- You will likely be asked for a biopsy or blood sample for biomarker testing - even if you’ve had one before. Tumor biology changes over time.
- Don’t assume your old test results are enough. Many trials require testing done within 90 days of screening.
- Ask: "What biomarker are you testing for?" and "What happens if I don’t have it?" Some trials now offer alternative arms for patients without the target biomarker.
- Ask about access. If your local hospital can’t run the test, will the trial help you get it done elsewhere?
The goal isn’t to exclude. It’s to include the right people - the ones who will benefit most. And for many, that means a better chance at survival.
The Future: AI, Multi-Omic Panels, and Real-World Data
We’re not done evolving. The next wave is even more powerful.
AI is now helping design eligibility criteria. Top pharmaceutical companies use machine learning to scan thousands of patient records and find hidden patterns - like a combination of gene mutations and immune markers that predict response better than any single biomarker.
By 2025, 65% of new trials are expected to use multi-omic panels - combining DNA, RNA, protein, and immune data into one profile. Think of it as a full-body scan for cancer biology.
And real-world data? That’s the game-changer. Instead of waiting years to validate a biomarker in a trial, companies are now using data from electronic health records, cancer registries, and even patient-reported outcomes. By 2026, 82% of companies plan to use this to refine eligibility rules. It’s faster. More diverse. More accurate.
Decentralized testing - where patients collect blood samples at home and mail them in - is already in pilot with 12 companies. If it scales, it could remove one of the biggest barriers: travel.
Why This Matters Beyond the Lab
This isn’t just about science. It’s about equity. Biomarker-driven trials are more effective - but only if everyone can access the tests. Right now, a patient in rural Australia might wait months for a biopsy. Someone in Melbourne might get results in a week. That gap isn’t fair. And it’s not just a health issue - it’s a justice issue.
Regulators know this. The FDA and EMA are now pushing for biomarker access as part of trial approval. If a trial uses a biomarker, it must also show how it will ensure equitable testing across different populations.
The message is clear: the future of cancer care isn’t one-size-fits-all. It’s personalized. And that starts with knowing what’s inside you - not just what stage your cancer is in.
What happens if my biomarker test comes back negative?
If your biomarker test is negative, you won’t qualify for that specific trial. But that doesn’t mean you’re out of options. Many trials now offer "basket" or "umbrella" designs - meaning if you don’t match one biomarker, you might still qualify for another arm of the same study. Always ask if there are alternative eligibility paths. Some trials also have companion studies for patients without the target biomarker, testing different drugs or combinations.
Can I get biomarker testing done before I even consider a trial?
Yes - and it’s strongly recommended. Many hospitals now offer comprehensive tumor profiling as part of standard care, especially for advanced cancers. Tests like FoundationOne CDx or Tempus xT can screen for dozens of biomarkers at once. Having this data ready can save weeks when you’re ready to join a trial. Ask your oncologist if your tumor has been profiled and request a copy of the report.
Are biomarker tests covered by insurance?
In Australia, many biomarker tests for cancer are covered under Medicare if they’re clinically indicated and ordered by a specialist. In the U.S., most private insurers cover FDA-approved companion diagnostics. But some newer or exploratory biomarkers may not be covered. Always check with your insurer and the trial sponsor - many trials cover testing costs for participants. Don’t assume it’s too expensive; ask first.
How long does biomarker testing usually take?
It varies. Simple tests like IHC for HER2 can take 5-7 days. Complex genomic panels may take 10-21 days, especially if samples need to be shipped internationally. Liquid biopsies are faster - often 3-7 days. If you’re in a hurry, ask the trial team if they use a centralized lab with expedited processing. Some sites offer rush services for patients with rapidly progressing disease.
Why do some trials require a new biopsy even if I had one last year?
Cancer evolves. A biopsy from a year ago may not reflect your current tumor biology. Tumors can develop new mutations, lose target proteins, or change their immune environment. Trials require recent tissue - usually within 90 days - to ensure the biomarker status is accurate at the time of enrollment. This isn’t bureaucracy; it’s science. Using outdated data risks giving you a drug that won’t work.
Biomarker-based eligibility isn’t perfect. It’s complex, costly, and sometimes slow. But it’s also the most effective way we’ve ever had to match patients with the right cancer drugs. What used to be a trial of last resort is now a targeted, science-backed pathway to better outcomes. And for those who qualify? It’s not just hope - it’s a measurable advantage.



February 8, 2026 AT 01:39
My aunt went through this last year. Got her biopsy, waited three weeks, then found out she didn’t have the magic marker. They told her "sorry, next trial." She cried in the parking lot. I cried with her. This system feels like a lottery where only some get to play. Why can’t they just try the drug on everyone and see what happens? I know science says no, but I still feel like it’s cruel.