More than half of all new cancer drugs approved in the last five years are taken by mouth. That’s not a trend-it’s a shift. For many people with cancer, swallowing a pill at home has replaced long clinic visits for IV infusions. It sounds easier. But oral chemotherapy isn’t just convenient. It’s complex. And getting it wrong can mean the difference between treatment working and failing.
Why Oral Chemotherapy Is Different
Oral chemotherapy works the same way as IV chemo: it kills fast-growing cancer cells. But how it gets into your body changes everything. Tablets, capsules, or liquids are absorbed through your gut, processed by your liver, and delivered to tumors. That means your body’s own systems-digestion, metabolism, even what you eat-can change how well the drug works. Traditional chemo drugs like cyclophosphamide and newer targeted ones like capecitabine or dasatinib each have their own rules. Alkylating agents attack DNA directly. Antimetabolites trick cells into using fake building blocks. Targeted drugs block specific proteins cancer needs to grow. Each class has different side effects, different interactions, and different ways your body handles them. The big advantage? Less time in hospitals. Patients save an average of 3.7 hours per treatment cycle. But that convenience comes with hidden risks. You’re now responsible for giving yourself a powerful drug. No nurse is watching. No IV pump is controlling the dose. If you forget, skip, or take it with the wrong food, the treatment can fail-or harm you.How Oral Chemotherapy Affects Your Body
Side effects vary wildly depending on the drug. But some patterns are clear. Alkylating agents like cyclophosphamide often cause severe nausea, hair loss, and low blood counts. About 65% of people on cyclophosphamide experience myelosuppression-meaning their bone marrow slows down production of red cells, white cells, and platelets. That raises infection risk and causes fatigue. Antimetabolites like capecitabine are notorious for hand-foot syndrome. Your palms and soles turn red, feel burning, peel, or crack. Up to 53% of patients get it, even at mild levels. Diarrhea hits 45%, and mouth sores (mucositis) affect 30%. These aren’t just uncomfortable-they can force you to stop treatment. Targeted drugs bring their own problems. Dasatinib and lenalidomide can drop blood counts fast-78% and 62% of patients, respectively-within the first six weeks. That means weekly blood tests aren’t optional. Liver damage is another silent threat: 15-25% of people on oral chemo show elevated liver enzymes. Without regular checks, it can progress unnoticed. Some drugs cause unique issues. VEGF inhibitors like sunitinib raise blood pressure in 25-35% of patients. EGFR inhibitors like erlotinib lead to severe skin rashes in 75-90% of users. These aren’t side effects you can ignore. They’re signals your body is reacting-and sometimes, they mean the drug is working.Safety Risks You Can’t Afford to Ignore
The biggest danger with oral chemotherapy isn’t the drug itself. It’s how you take it. A 2023 study from Dana-Farber found that 42% of serious problems with oral chemo came from mistakes in administration-not the drug’s toxicity. That’s staggering. You’re not just taking medicine. You’re managing a high-risk process. Drug interactions are a major threat. Many oral chemo drugs are broken down by the CYP3A4 enzyme in your liver. If you take something that boosts this enzyme-like the antibiotic rifampin-your drug levels can crash. Dasatinib levels drop by 80% with rifampin. That’s like taking a quarter of your dose. On the flip side, inhibitors like ketoconazole (an antifungal) can make your drug levels spike. Lapatinib levels jump 325% with ketoconazole. That’s not just risky-it’s dangerous. Toxicity can hit fast. Antacids and proton pump inhibitors (PPIs) are another trap. Capecitabine needs an acidic stomach to absorb properly. If you take an antacid two hours before or after your dose, absorption drops by 30-50%. That means less drug reaches your cancer. Timing matters. You can’t just pop a pill whenever you feel heartburn. Storage and disposal matter too. Most oral chemo drugs need to be kept at room temperature (20-25°C). Don’t leave them in a hot car or a damp bathroom. Used pills go in FDA-approved disposal bags-not the toilet or trash. These aren’t suggestions. They’re safety rules.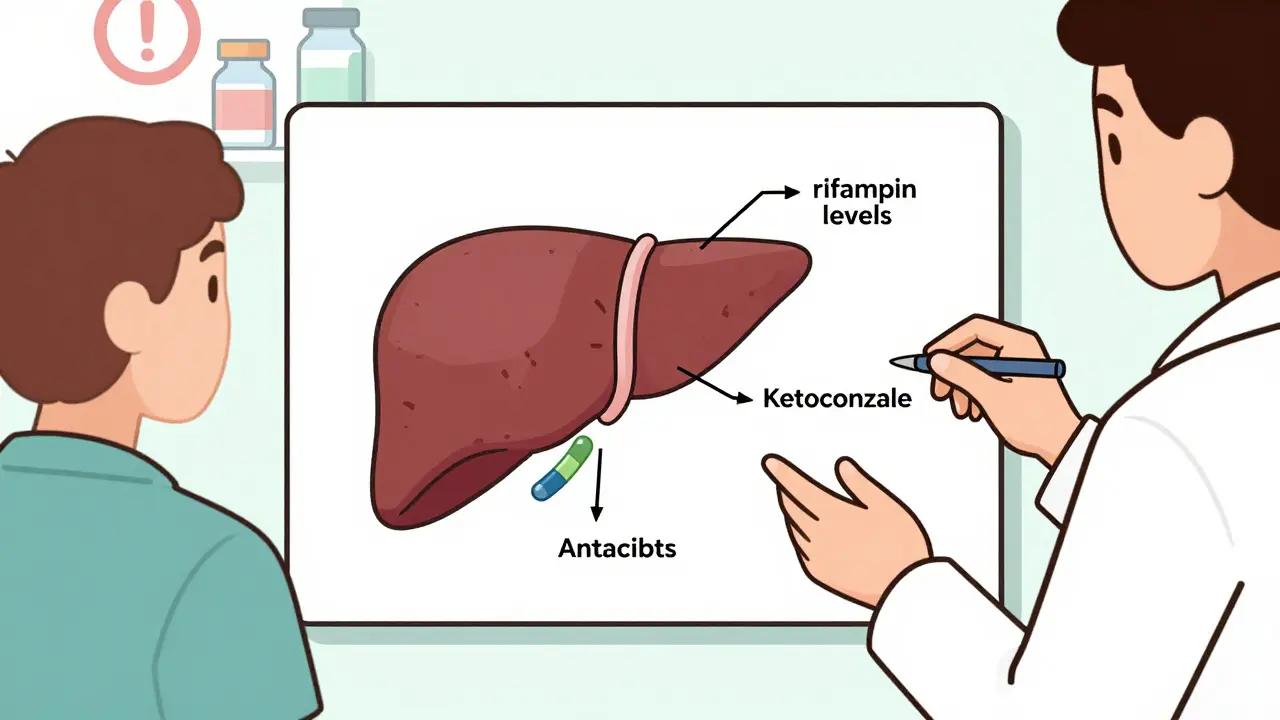
Why Adherence Is the Biggest Challenge
Only 55-75% of patients take oral chemotherapy exactly as prescribed. That’s far lower than the 85-95% adherence seen with IV chemo, where a nurse hands you the drug. Why? Because it’s hard. Some regimens require twice-daily dosing for 14 days, then a full week off. Miss one dose? You’re not just behind-you’re risking resistance. Take an extra dose? You could overdose. Dietary rules add another layer. Nilotinib must be taken on an empty stomach. You can’t eat for two hours before or after. That’s not easy if you’re nauseous, tired, or juggling family meals. Side effects make adherence worse. If your hands hurt from hand-foot syndrome, you might skip doses. If you’re too tired to swallow pills, you might delay them. Some patients even cut doses in half to feel better. That’s not bravery. It’s dangerous. The data shows the cost. A 2021 JAMA Oncology study called non-adherence “the equivalent of leaving one out of every three patients untreated.” That’s not a statistic. It’s a tragedy.How to Get It Right
Success with oral chemotherapy isn’t luck. It’s a system. First, education. You need at least 45 minutes of one-on-one time with a trained nurse or pharmacist. They don’t just hand you a pamphlet. They ask you to repeat back what you’ve learned. “Teach-back” is the gold standard. If you can’t explain how to take your meds, you’re not ready to go home. Second, tools. Pill organizers with labeled compartments help. Digital calendars with alarms work better than paper lists. Some pharmacies now offer blister packs with daily doses pre-sorted. These aren’t luxuries-they’re lifelines. Third, follow-up. The best programs call you on day 3, day 7, and day 14 after you start. They ask: Are you having side effects? Are you taking the pills? Did you miss any? They don’t wait for you to call. They reach out. Fourth, support. Pharmacists monitor refill patterns. If you don’t refill on time, they call. If you’re struggling with side effects, they connect you with a nurse or social worker. You’re not alone. There’s a team behind you. A 2022 study in the Journal of Oncology Practice showed that with this full support system, adherence jumped from 58% to 82%. That’s not a small gain. It’s life-changing.New Tools Making a Difference
Innovation is catching up. The FDA approved the Proteus Discover system in 2021-a tiny sensor inside the pill that sends a signal to a patch on your skin when you swallow it. Your care team gets a real-time alert if you missed a dose. Smart pill bottles with Bluetooth are in phase 3 trials. They track when you open the cap, and if you haven’t opened it in 24 hours, they text you. Early results show 92% accuracy in predicting adherence. Genetic testing is now standard before some drugs. DPYD testing before giving fluoropyrimidines like capecitabine cuts severe toxicity by 72%. That’s not science fiction. It’s routine in major cancer centers. Fixed-dose combinations are simplifying regimens. VerzenioPlus combines two drugs in one pill. Fewer pills. Fewer chances to mess up.
What You Need to Do
If you’re on oral chemotherapy:- Know your drug’s name, dose, and schedule. Write it down.
- Ask: “What foods, supplements, or other meds should I avoid?”
- Use a pill organizer. Set phone alarms.
- Don’t skip doses-even if you feel fine.
- Report side effects immediately. Don’t wait for your next appointment.
- Ask for a pharmacist consult. They’re experts in drug interactions.
- Keep your meds at room temperature. Store them out of reach of kids or pets.
- Dispose of used pills properly. Never flush them.
What Your Care Team Needs to Do
Cancer centers are now required by the National Comprehensive Cancer Network to have formal oral chemotherapy programs. That means:- Every patient gets a structured education session before leaving the clinic.
- Follow-up calls are scheduled-not optional.
- Pharmacy refill data is monitored.
- Side effect management is built into the plan.
Final Thought
Oral chemotherapy isn’t the future. It’s here. And it’s not simpler. It’s more demanding. But with the right support, it can be just as effective as IV chemo-and far more comfortable. The goal isn’t just to survive cancer. It’s to live well while fighting it. That means taking your pills exactly as prescribed, managing side effects before they take over, and never feeling like you’re on your own. You’re not just a patient. You’re a partner in your care. And with the right tools and team, you can win.Can I take oral chemotherapy with other medications?
Not without checking. Many oral chemotherapy drugs interact with common medications like antacids, antibiotics, antifungals, and even over-the-counter pain relievers. For example, rifampin can reduce dasatinib levels by 80%, while ketoconazole can increase lapatinib levels by 325%. Always give your pharmacist and oncologist a full list of everything you take-including vitamins and herbal supplements.
What should I do if I miss a dose of oral chemotherapy?
Don’t double up. Call your care team immediately. The action depends on the drug and how long you’ve missed. For some, you skip the missed dose and resume your next scheduled dose. For others, you may need to adjust your schedule. Never guess. Your oncology team has specific protocols for each medication.
Why do I need to avoid food before and after taking some oral chemo drugs?
Food can block absorption. Drugs like nilotinib and dasatinib need an empty stomach to work properly. Eating even a snack can reduce how much of the drug enters your bloodstream. For capecitabine, antacids or PPIs can cut absorption by 30-50%. Always follow the exact timing instructions: usually 2 hours before and after food or other meds.
How do I know if my oral chemotherapy is working?
You won’t feel it the way you might with IV chemo. Blood tests, scans, and tumor markers are the real indicators. Your care team will monitor your blood counts, liver function, and imaging over time. Side effects like rashes or high blood pressure can sometimes signal the drug is active-but they’re not reliable proof. Always rely on clinical tests, not how you feel.
Are there tests to predict how I’ll respond to oral chemotherapy?
Yes. For drugs like capecitabine or fluorouracil, a DPYD gene test is now standard before starting. People with certain gene variants are at high risk for life-threatening toxicity. Testing reduces severe side effects by 72%. Other tests look at liver enzymes or drug metabolism genes. Ask your oncologist if genetic testing is right for your drug.
Can I drink alcohol while on oral chemotherapy?
It’s best to avoid alcohol. Many oral chemo drugs are processed by the liver, and alcohol adds stress to an already overworked organ. It can worsen liver toxicity, increase nausea, and interfere with sleep and healing. Even moderate drinking can reduce treatment effectiveness. Always ask your care team about your specific drug.
What should I do if I have severe side effects?
Don’t wait. Contact your oncology team immediately. Severe diarrhea, high fever, uncontrolled vomiting, chest pain, or signs of infection (like chills or low blood pressure) require urgent attention. Many centers have 24/7 on-call nurses for patients on oral chemo. Keep their number handy. Delaying care can turn a manageable side effect into a life-threatening emergency.






December 18, 2025 AT 18:43
this is just another way for big pharma to make us do all the work while they cash in. no nurse watching? yeah right, they just want you to mess up so they can sell you more drugs.