Side Effect Reduction Calculator
How This Tool Works
Based on research from the article, combination therapy with lower doses of multiple medications can significantly reduce side effects while maintaining treatment effectiveness. Enter values below to calculate potential side effect reduction.
Side Effect Reduction
Based on your inputs, this combination therapy could reduce side effects by 0% compared to single high-dose treatment.
For example:
Hypertension: 9.8% cough reduction to 2.3% with combination therapy = 75% reduction
For years, doctors reached for higher doses of a single drug when a patient’s condition didn’t improve. But what if the real problem wasn’t the drug-it was the dose? In recent years, a quieter revolution has taken hold in medicine: using combination therapy-lower doses of two or more medications together-to get better results with fewer side effects. This isn’t experimental. It’s now standard care for high-blood pressure, type 2 diabetes, and certain cancers. And for many patients, it’s the difference between feeling okay and feeling like themselves again.
Why Higher Doses Don’t Always Mean Better Results
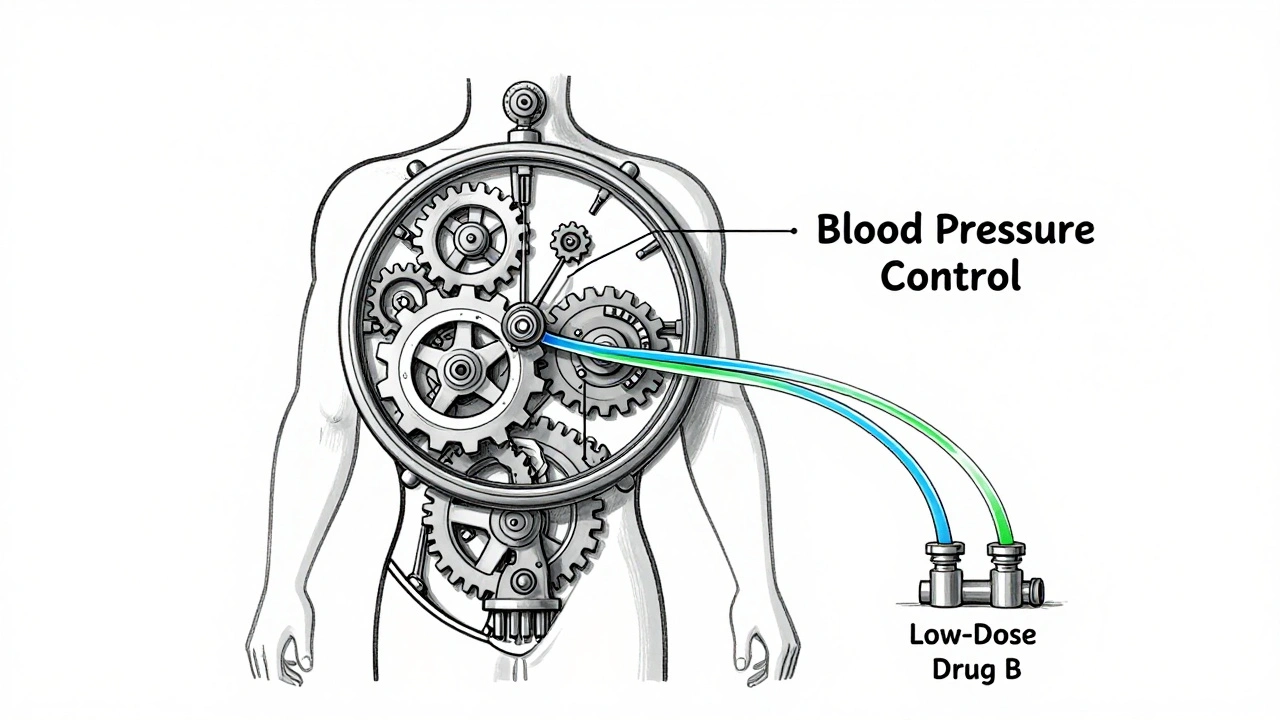
Think of your body like a machine with many moving parts. A drug that targets one part-say, a blood pressure medication that relaxes blood vessels-can cause unintended side effects when pushed too hard. High doses of ACE inhibitors, for example, can trigger a dry, hacking cough in nearly 10% of users. Increase the dose even more, and the cough doesn’t get better-it just gets louder. Meanwhile, the blood pressure might barely budge. The solution? Add a second drug that works differently. Instead of pushing one drug to its limit, you use half the dose of two drugs that complement each other. In hypertension, combining a low-dose ACE inhibitor with a low-dose calcium channel blocker doesn’t just add up-it multiplies. Studies show this combo lowers systolic blood pressure by nearly 9 mmHg more than the highest dose of either drug alone. And the side effects? Cough drops from 9.8% to 2.3%. Ankle swelling? Falls from 14.3% to 4.1%. This isn’t magic. It’s pharmacology. Different drugs hit different targets. When you combine them at lower doses, you get broader control without overwhelming any one system.Real-World Success Stories Across Conditions
In diabetes, metformin has long been the first-line drug. But at full dose (2000 mg/day), up to 26% of patients get nausea, diarrhea, or bloating so bad they quit. What if you cut the metformin in half-1000 mg-and add a low dose of an SGLT2 inhibitor like empagliflozin (10 mg)? The result? Just as good HbA1c control (around 1.3% drop), but gastrointestinal side effects cut in half-to 11.7%. And you avoid the rare but dangerous risk of lactic acidosis, which drops from 0.03 to 0.01 cases per 1000 patients per year. In cancer, the story is even more striking. A high dose of anthracycline (90 mg/m²) might shrink a tumor, but it also damages the heart in 7.3% of patients over five years. Now, combine it with a lower dose of cyclophosphamide (600 mg/m² instead of 900 mg/m²). Tumor response stays the same-but heart damage drops to 2.1%. Neutropenia (dangerously low white blood cells) falls from 38.7% to 19.2%. That’s not just safer-it’s life-saving. And then there’s the polypill. In a landmark 2021 trial published in The Lancet, researchers gave 12,200 people without heart disease a single pill containing four low-dose drugs: aspirin, simvastatin, lisinopril, and atenolol-all at 50-75% of standard doses. Over five years, those taking the polypill had 53% fewer heart attacks, 51% fewer strokes, and 49% lower risk of dying from heart disease. No one was on high doses. No one was on five separate pills. Just one pill, with each component dialed down.The Hidden Benefit: Adherence
Taking one pill a day is easy. Taking four? Not so much. A 2023 American Heart Association survey of over 8,400 patients found that 68% of people stuck with a single-pill combination for high blood pressure. But when they were on multiple separate pills, adherence dropped to 52%. Why? Simple: memory. Complexity. The fear of missing one. One patient in a case study from the American College of Cardiology had tried three different single drugs for hypertension over ten years. Each one made her dizzy or swollen. When her doctor switched her to a fixed-dose combo of telmisartan 20 mg and amlodipine 2.5 mg, her blood pressure dropped to target in four weeks. She told her doctor, “For the first time in 10 years, I don’t have dizziness or ankle swelling.” But it’s not all smooth sailing. A 2024 Diabetes Care survey of nearly 13,000 patients found that 31% stopped their combination therapy within a year-not because it didn’t work, but because they felt overwhelmed by “too many medications.” Online forums like Reddit’s r/Diabetes are full of posts like: “I’m taking five pills a day. My husband says I look like a pharmacy.” That’s why fixed-dose combinations (FDCs)-where two or more drugs are baked into one pill-are becoming the gold standard. They reduce pill burden, cut costs, and improve compliance. In fact, studies show FDCs improve adherence by 24% compared to taking the same drugs as separate pills.
When Combination Therapy Can Backfire
This isn’t a cure-all. There are clear risks. A 2022 New England Journal of Medicine study found that triple-combination therapy in adults over 75 with poor kidney function (eGFR under 45) increased the risk of acute kidney injury by 1.8 times. In oncology, a 2023 Cell study reanalyzed 15 FDA-approved drug combos and found that 38% showed no real synergy-meaning patients got the side effects of two drugs without the benefit of better tumor control. That’s not treatment. That’s gamble. And then there’s cost. A combination therapy regimen averages $4,217 per year, compared to $2,864 for a single drug. But here’s the catch: those extra costs are often offset. In diabetes, the American Diabetes Association found that combination therapy saves $7,842 per patient per year in avoided complications-hospitalizations, dialysis, amputations. So while the pill costs more, the overall burden on the system-and the patient’s life-goes down. The biggest hidden risk? Drug interactions. In patients over 65 managing five or more medications, nearly half of all combination therapy complications reported to the FDA in 2023 were due to unexpected interactions. A blood thinner plus a certain antibiotic. A statin plus grapefruit juice. These aren’t rare. They’re common.Who Benefits Most-and Who Should Be Cautious
Combination therapy works best for people with moderate to high risk of complications. That means:- Stage 2 hypertension (systolic over 140 or diastolic over 90)
- Type 2 diabetes with HbA1c above 7.5% at diagnosis
- High-risk cardiovascular patients (smokers, diabetics, those with family history)
- Patients who’ve failed on at least one monotherapy
- Older adults with poor kidney function
- People already taking five or more medications (risk of pill burden)
- Those with complex liver disease or unstable mental health

What’s Next: The Future of Personalized Combination Therapy
The next frontier isn’t just combining drugs-it’s combining them smartly. The POLYDELPHI trial, currently recruiting 15,000 people, is testing a five-drug combo at ultra-low doses (each at 20-30% of normal). The goal? To cut cardiovascular risk by 70% without triggering side effects. Meanwhile, Harvard researchers are developing “response-adaptive sequencing”-a system where your body’s reaction to one drug determines the next. If your blood pressure drops too fast? The system reduces the next dose. If your glucose stays high? It adds a different agent. No more guesswork. And the market is responding. The global combination therapy market is projected to hit nearly $300 billion by 2028. In India, polypill use jumped from 5% to nearly 19% in just three years. The FDA approved 47 new combination drugs in 2023-up from 32 the year before. The message is clear: medicine is moving away from brute-force dosing toward precision stacking. Lower doses. Fewer side effects. Better outcomes. And for many, a return to normal life.What You Can Do If You’re on Combination Therapy
If you’re taking multiple medications:- Ask your doctor: “Is there a fixed-dose combo version of what I’m taking?”
- Keep a list of every pill, including over-the-counter and supplements.
- Use a pill organizer with alarms-especially if you’re on more than three drugs.
- Get your kidney and liver function checked every 3-6 months if you’re over 65.
- Report any new symptoms-even if you think they’re “normal.”
Final Thought: It’s Not About More Drugs. It’s About Smarter Dosing.
Combination therapy isn’t about throwing more chemicals at a problem. It’s about working with the body’s complexity, not against it. Lower doses mean less strain. Fewer side effects mean better quality of life. And single-pill combinations mean people actually stick with their treatment. The goal isn’t to take the most pills. It’s to take the right ones-just enough, at the right time, with the least harm. That’s not just medicine. That’s better living.Is combination therapy safe for older adults?
It can be, but only with careful monitoring. Older adults, especially those over 75 with reduced kidney function, face higher risks of acute kidney injury and drug interactions. Doctors typically start with lower doses and check kidney and electrolyte levels every 4-6 weeks. Fixed-dose combinations are preferred over multiple separate pills to reduce confusion and improve safety.
Can combination therapy reduce my pill burden?
Yes-especially if your medications are available as a fixed-dose combination (FDC). For example, instead of taking three separate pills for blood pressure, you might take one pill containing two or three drugs at lower doses. This cuts the number of pills you take daily, which improves adherence and reduces the chance of missing doses.
Do combination therapies cost more than single drugs?
Yes, the upfront cost is often higher-around $4,200 per year versus $2,800 for a single drug. But many combination therapies reduce long-term costs by preventing hospitalizations, strokes, and other complications. In diabetes, for example, the extra cost of combination therapy is offset by $7,800 in avoided care costs per patient annually. Generic FDCs are now widely available and can be as affordable as single generics.
What if I’m already on multiple medications? Can I still switch to combination therapy?
Possibly, but it requires a careful review. If you’re taking five or more medications, adding more increases the risk of interactions and confusion. Your doctor may first simplify your regimen-eliminating duplicates or unnecessary drugs-before introducing a combination therapy. Always consult your pharmacist or prescriber before making changes.
Are there any side effects I should watch for with combination therapy?
Yes. While side effects are generally lower than with high-dose monotherapy, new combinations can cause unexpected reactions. Watch for dizziness, swelling, unusual fatigue, changes in urination, or muscle pain. In cancer treatment, watch for fever or signs of infection. If you notice anything new or worsening, contact your doctor. Drug interactions are more common in people taking multiple medications, so always disclose everything you’re using-including vitamins and herbal supplements.





December 9, 2025 AT 11:16
So basically we're finally admitting that more isn't better? Took long enough. I've been on three different blood pressure pills and one of them made me feel like a zombie. Switched to the combo pill? Now I can actually jog without wanting to nap. 🙌