GLP-1 Gallbladder Symptom Checker
Assess Your Symptoms
This tool helps identify potential gallbladder issues related to GLP-1 agonist medications. Do NOT use this as medical advice. If you experience these symptoms, contact your healthcare provider immediately.
Key Warning Signs from Research
89% of patients with acute cholecystitis on GLP-1 agonists experienced persistent right upper pain lasting >30 minutes.
75% required emergency surgery when symptoms weren't addressed early.
Patients who sought help within 24 hours were 5 times less likely to need emergency surgery than those who waited longer.
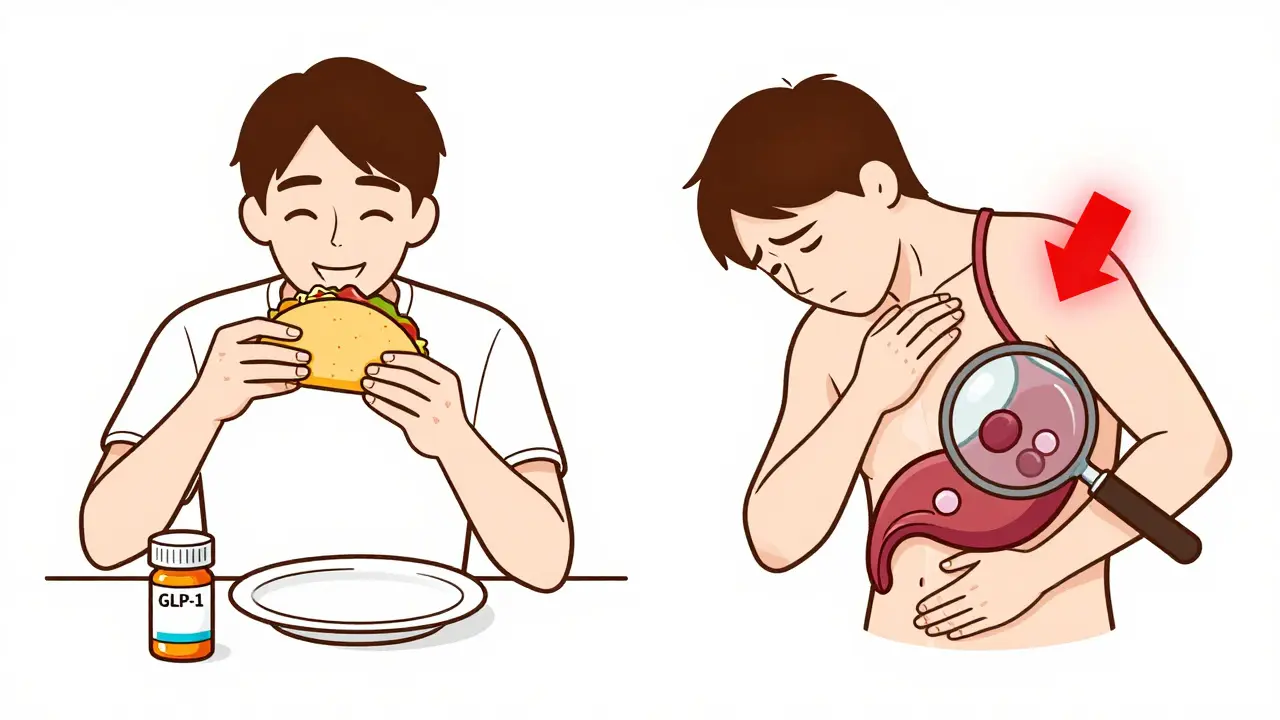
When you start a GLP-1 agonist like Ozempic or Wegovy for weight loss or diabetes, the goal is clear: lose weight, feel better, lower your blood sugar. But what if the very medication helping you lose pounds starts causing pain in your upper right abdomen? That’s not a coincidence. It’s a warning sign many patients - and even some doctors - are missing.
Why GLP-1 Agonists Can Trigger Gallbladder Problems
GLP-1 agonists work by mimicking a hormone your body naturally makes after eating. This hormone slows digestion, reduces appetite, and helps your pancreas release insulin. But it also does something else: it shuts down the gallbladder’s ability to contract properly. Your gallbladder stores bile - the fluid your liver makes to digest fats. When you eat something fatty, your body releases a chemical called cholecystokinin. That tells your gallbladder to squeeze and dump bile into your small intestine. GLP-1 agonists block this signal. Without that squeeze, bile sits still. And when bile sits still, it thickens. Over time, it can form sludge. Then stones. Then infection. This isn’t theoretical. A major 2022 analysis of 56,000 people across 76 clinical trials found that those on GLP-1 agonists had a 37% higher risk of gallbladder disease than those not taking them. The risk was highest in people using higher doses for weight loss - like Wegovy (2.4 mg semaglutide) or Saxenda (3.0 mg liraglutide). In those groups, about 1 in 100 people developed gallstones. That’s rare overall, but when you’re talking about millions of users, that’s thousands of people needing surgery.The Real Red Flags: Pain That Can’t Be Ignored
Not all stomach pain is the same. If you’re on a GLP-1 agonist and you feel pain, don’t assume it’s just bloating or a side effect of slower digestion. Here’s what real gallbladder trouble looks like:- Right upper quadrant pain - that’s the area just under your ribs on the right side. Not a dull ache. A sharp, steady pain that lasts more than 30 minutes.
- Pain that radiates to your right shoulder - this happens because the nerves connecting your gallbladder and shoulder get confused. It’s a classic sign.
- Pain after eating fatty food - tacos, cheese, fried chicken, buttered toast. If your pain starts 30 to 90 minutes after eating these, it’s a strong clue.
- Nausea or vomiting with the pain - not just feeling queasy. Actual vomiting. This raises the chance of cholecystitis (gallbladder infection) by nearly 4 times.
- Pain that comes on suddenly and gets worse - not something that fades after a few hours. If it’s still there the next morning, or if you’re running a fever, you need help now.
Who’s at Highest Risk?
This isn’t a risk that hits everyone equally. Certain people are far more likely to develop complications:- Women over 40 - hormonal changes make them more prone to gallstones, even without medication.
- People with obesity (BMI over 30) - fat tissue increases cholesterol in bile, making stones more likely.
- Those losing weight rapidly - losing more than 1.5 kg (3.3 lbs) per week is a major trigger. The gallbladder doesn’t have time to adjust.
- Anyone with prior gallstones - even if they were silent before, GLP-1 agonists can make them move and get stuck.
- People taking liraglutide or semaglutide at weight-loss doses - these carry the highest risk. Liraglutide 3.0 mg has the strongest link to abdominal pain among all GLP-1 drugs.
What Happens When You Ignore the Pain?
Some patients think, “I’m losing weight - this pain must be worth it.” That’s dangerous thinking. In the 2022 case series published in JAMA Internal Medicine, 75% of patients who developed acute cholecystitis on GLP-1 agonists ended up needing their gallbladder removed. That’s not a minor procedure. It’s major surgery. Recovery takes weeks. You’ll need to change how you eat - no more heavy meals, no fried foods, no butter. Some people develop diarrhea or bloating for months after surgery. And it’s not just about surgery. If a stone blocks the bile duct, you can get pancreatitis - a life-threatening inflammation of the pancreas. Or a severe infection that spreads to your bloodstream. Both require ICU care. The average time from starting a GLP-1 agonist to developing symptoms? About six months. That’s why so many patients don’t connect the dots. They think, “I’ve been on this for months - it’s fine.” But the risk peaks in the first year. After that, it drops. But not enough to ignore early signs.What to Do If You Have Pain
Don’t wait. Don’t take antacids and hope it goes away. Don’t assume it’s “just gas.”- Stop the medication - if you suspect gallbladder trouble, pause the drug immediately. Don’t wait for your doctor’s appointment.
- Get an ultrasound - this is the first test doctors use. It’s quick, painless, and shows stones, sludge, or swelling.
- Don’t eat fatty foods - this won’t fix the problem, but it can stop the pain from getting worse.
- Call your doctor or go to urgent care - if you have fever, vomiting, or pain lasting more than 6 hours, go to the ER.

What About People Who Already Had Their Gallbladder Removed?
Good news: if you’ve had a cholecystectomy, your risk drops dramatically. Without a gallbladder, there’s no place for stones to form. You might still get some bile duct irritation, but the chance of infection or blockage is very low. That doesn’t mean you’re completely safe. A tiny number of people still have leftover stones in the bile ducts. But the risk is minimal - less than 1 in 500. If you’ve had your gallbladder out and you’re considering a GLP-1 agonist, talk to your doctor. You’re likely a good candidate.Is There a Way to Prevent This?
Researchers are testing ways to reduce the risk. One promising option is ursodeoxycholic acid (UDCA), a bile acid that helps dissolve stones. A phase 2 trial at Mayo Clinic is currently studying whether taking UDCA alongside GLP-1 agonists can prevent gallstones in high-risk patients. In the meantime, there are two practical steps you can take:- Slow down your weight loss. Aim for 0.5 to 1 kg (1-2 lbs) per week. Rapid loss is the biggest trigger.
- Eat smaller, low-fat meals. Even if you’re on a GLP-1 agonist, your body still needs to digest food. Avoid heavy oils, butter, fried foods, and creamy sauces.
The Bigger Picture: Why This Isn’t Going Away
GLP-1 agonists are one of the biggest medical breakthroughs in decades. They’re changing how we treat obesity and diabetes. But like any powerful tool, they come with trade-offs. In 2023, over 45 million prescriptions for these drugs were written in the U.S. alone. Gallbladder events are still rare - about 1 in 200 people. But with that many users, that’s still over 200,000 people who might need surgery. The FDA has updated labels. Doctors are learning. But many primary care providers still don’t know the connection. Patients aren’t warned. And the pain? It’s often dismissed as “normal side effects.” This isn’t about scaring people off GLP-1 agonists. It’s about using them safely. You can still lose weight. You can still improve your health. But you need to know the signs - and act fast.If you’re on one of these drugs and you feel pain in your upper right side - especially after eating - don’t ignore it. Don’t wait. Don’t hope it goes away. Get checked. Your gallbladder might be silent now. But it won’t stay that way forever.
Can GLP-1 agonists cause gallstones even if I’ve never had them before?
Yes. GLP-1 agonists slow gallbladder emptying, which causes bile to thicken and form stones over time. This can happen even in people with no prior history. The risk is highest in those on higher doses for weight loss, women over 40, and people losing weight rapidly.
How long after starting a GLP-1 agonist do gallbladder symptoms usually appear?
Most cases show up between 3 and 9 months after starting the medication. The median time is around 180 days. But symptoms can begin as early as 6 weeks or as late as 18 months. The highest risk window is the first year.
Should I stop taking my GLP-1 agonist if I have abdominal pain?
If you experience right upper quadrant pain lasting more than 30 minutes, especially with nausea or after eating fatty food, stop the medication and contact your doctor immediately. Continuing the drug can worsen inflammation and lead to infection or pancreatitis. Do not wait for your next appointment.
Are all GLP-1 agonists equally risky for gallbladder problems?
No. Liraglutide (Saxenda) has the highest relative risk, followed by semaglutide (Ozempic, Wegovy). Exenatide (Byetta) shows a much lower risk. The risk correlates with dose and weight loss effect - higher doses for obesity carry more risk than lower doses for diabetes.
Can I still take a GLP-1 agonist if I’ve had gallstones in the past?
Use extreme caution. If you’ve had gallstones, even if they were asymptomatic, starting a GLP-1 agonist can cause them to move and block ducts, leading to emergency surgery. Talk to a gastroenterologist first. An ultrasound before starting is strongly recommended. In many cases, doctors will advise against it unless the benefits clearly outweigh the risks.
Does removing the gallbladder eliminate all risk from GLP-1 agonists?
Almost. Without a gallbladder, you can’t form new gallstones. The risk of infection or blockage drops by over 90%. There’s still a tiny chance of residual stones in the bile ducts causing issues, but this is very rare. If you’ve had your gallbladder removed, you’re generally considered low-risk for GLP-1 agonist-related complications.






December 24, 2025 AT 11:30
Let me get this straight - you’re telling me that after spending months on Ozempic to finally fit into my jeans, I now have to worry about my gallbladder staging a coup? And the worst part? No one warned me. This isn’t medicine, it’s a bait-and-switch with a prescription pad.
They market these drugs like miracle weight-loss wands, then bury the fine print in a 40-page appendix written in Latin. I’m not a doctor, but even I can see the hypocrisy. Lose weight? Sure. But if you develop gallstones? That’s your problem now.
And don’t even get me started on the fact that the FDA only updated the label after thousands of ER visits. That’s not regulation - that’s damage control with a corporate smile.
My cousin got her gallbladder out last year. She’s 42, lost 60 lbs on Wegovy, and now she can’t eat avocado toast without crying. No one told her the trade-off was permanent dietary exile.
This isn’t a side effect. It’s a silent epidemic masked as progress. And the people who profit? They’re still selling it like it’s the next iPhone.