Most people don’t know their arteries are silently clogging up years before they feel any symptoms. A simple, quick CT scan can show you exactly how much plaque is building up in your heart’s arteries - and whether you’re at higher risk for a heart attack, even if you feel fine. This isn’t science fiction. It’s called a coronary calcium score, and it’s one of the most powerful tools we have to catch heart disease before it’s too late.
What Exactly Is a Coronary Calcium Score?
A coronary calcium score comes from a special type of CT scan that looks for calcium deposits in the coronary arteries - the blood vessels that feed your heart muscle. These deposits aren’t just random mineral buildup. They’re a sign of atherosclerosis, the process where fatty plaque builds up inside artery walls. Over time, this plaque hardens with calcium, making it visible on a CT scan.
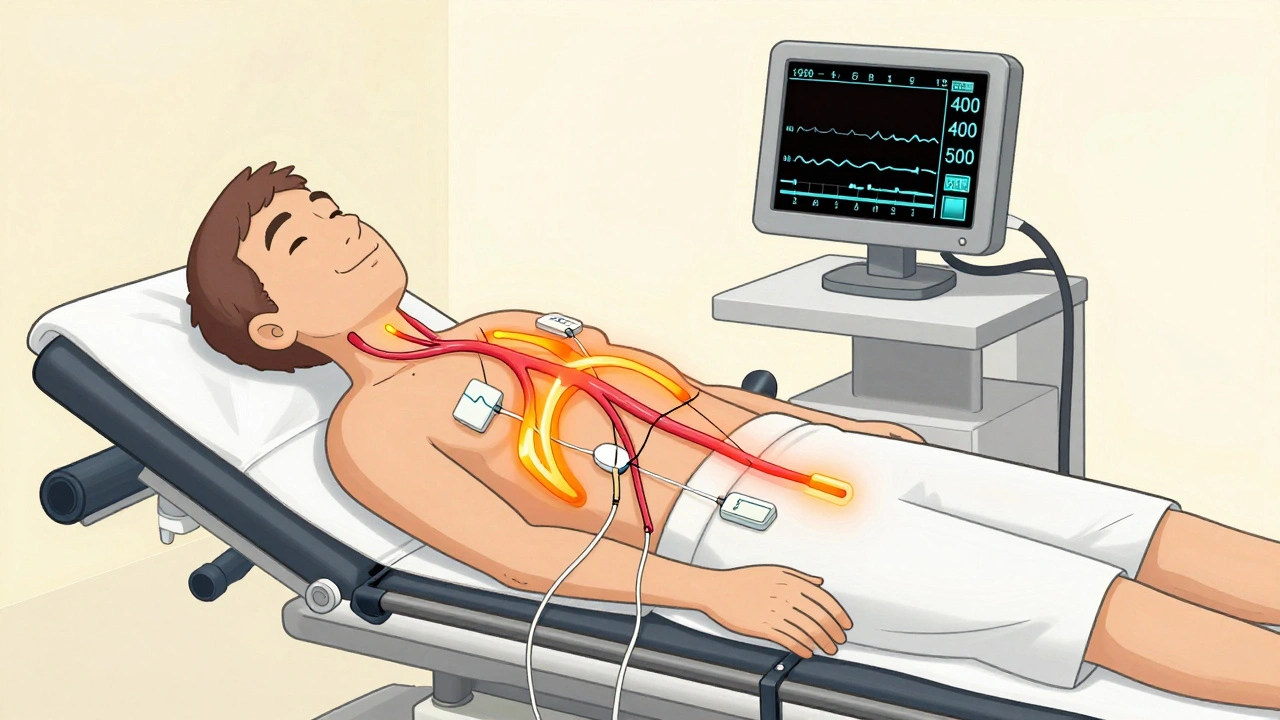
The scan doesn’t need contrast dye, needles, or stress tests. You lie on a table, EKG leads are stuck to your chest to track your heartbeat, and you hold your breath for 10 to 15 seconds while the machine takes hundreds of images. The whole thing takes under five minutes. No pain. No recovery. No fasting beyond avoiding caffeine and smoking for a few hours beforehand.
The result? A number - your calcium score. That number tells you how much calcified plaque is in your arteries right now. It’s not a guess. It’s a direct count.
What Do the Numbers Mean?
Your calcium score is measured using the Agatston method, developed in the 1990s and still the gold standard today. It doesn’t just count spots of calcium - it weights them by how dense they are. A score of zero means no detectable calcium. That’s good. But it doesn’t mean zero risk. Non-calcified plaque - softer, more dangerous plaque - can still be present.
Here’s what the numbers actually mean in real terms:
- 0: No detectable plaque. Low risk, but not zero risk.
- 1-10: Minimal plaque. Still low risk, but a signal to pay attention to lifestyle.
- 11-100: Mild plaque. You have early signs of artery disease. Risk is elevated.
- 101-400: Moderate plaque. Your risk of a heart attack is 75% higher than someone with no calcium.
- 401+: Extensive plaque. High risk. This level often means you’re in the top 10% for your age group.
But here’s the key: your score isn’t just a number. It’s compared to others your age, sex, and ethnicity. A score of 150 might be normal for a 65-year-old man but alarmingly high for a 45-year-old woman. That’s why reports include a percentile - showing how you stack up against peers.
Why This Test Beats Traditional Risk Calculators
Doctors have used tools like the Pooled Cohort Equations for years to estimate heart disease risk. These calculators look at cholesterol, blood pressure, smoking, diabetes, and age. But they’re wrong about one in every four people.
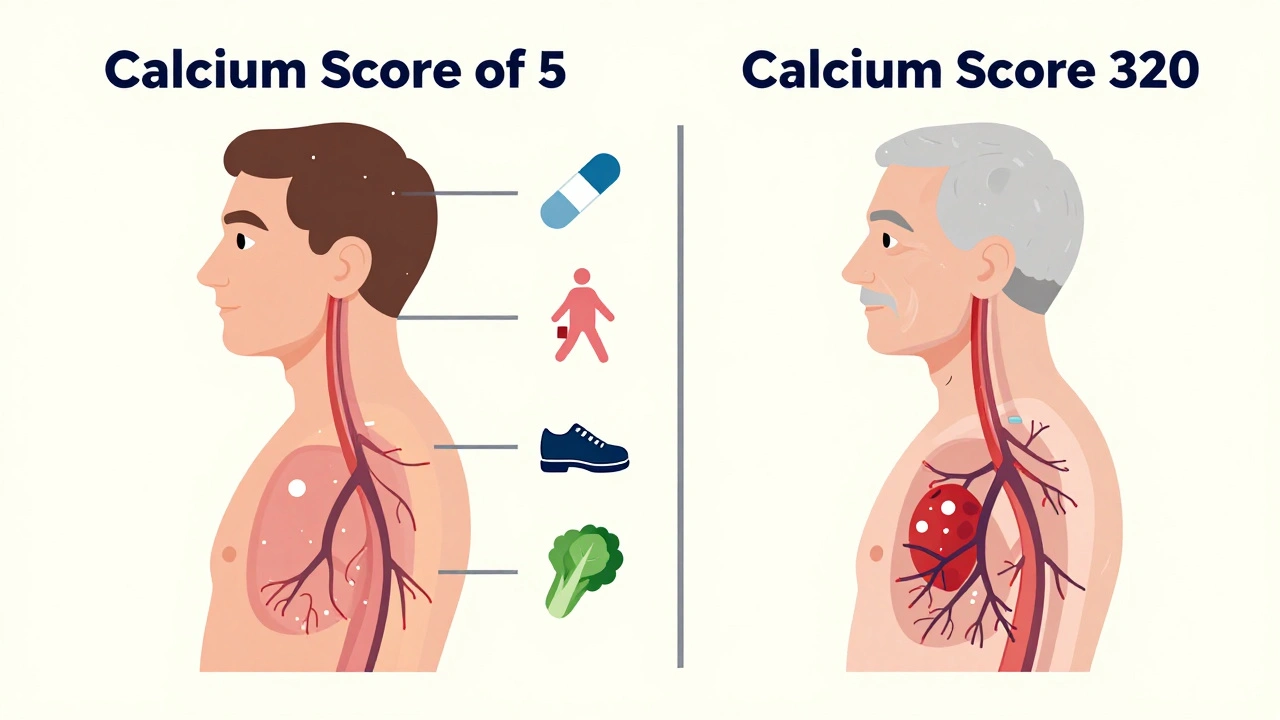
Here’s the problem: someone might have perfect cholesterol and normal blood pressure, but still have a calcium score of 320. That person is at high risk - but the calculator would tell them they’re low risk. That’s dangerous.
Studies show coronary calcium scoring reclassifies risk in 40-50% of people labeled as “intermediate risk” by traditional tools. That means a lot of people who were told they didn’t need statins actually do. And a lot of people who were told to take them might not need to.
One major study found adding calcium scoring to traditional risk factors improved accuracy from 73% to 81% in predicting heart events over 10 years. That’s a huge jump.
Who Should Get Tested?
This isn’t for everyone. You don’t need it if you’re young and healthy with no risk factors. But if you’re between 40 and 75 and have even one of these:
- High LDL (“bad”) cholesterol (160 mg/dL or more)
- Family history of early heart disease (before age 55 for men, 65 for women)
- High blood pressure
- Smoking history
- Diabetes or prediabetes
- Overweight or sedentary lifestyle
…then this test is worth considering. The American College of Cardiology and American Heart Association now give it a Class I recommendation - meaning it’s strongly supported - for people in this group.
It’s especially useful if your doctor is unsure whether to start you on a statin. A high calcium score can be the deciding factor.
What It Can’t Tell You
It’s important to know the limits. This scan only sees calcified plaque. About 20-30% of plaque is soft, fatty, and doesn’t show up on a calcium scan. That’s why a high score means high risk - but a low score doesn’t mean zero risk.
It also doesn’t show blockages. You can have a lot of calcium and still have open arteries. Or you can have a small blockage with no calcium. That’s why this test isn’t a replacement for a full cardiac workup if you have symptoms like chest pain or shortness of breath.
And if you have chronic kidney disease, your arteries may calcify for reasons unrelated to heart disease. That can make your score misleadingly high.
What Happens After the Score?
A score of zero? Keep doing what you’re doing - but stay vigilant. Get your numbers checked yearly.
A score of 100-300? This is the zone where most people benefit from a moderate-intensity statin, even if their cholesterol looks fine. Lifestyle changes become non-negotiable: daily walking, cutting sugar, eating more vegetables, quitting smoking if you haven’t already.
A score above 300? This is a red flag. High-intensity statins are usually recommended, along with blood pressure control and possibly aspirin. Many people at this level are advised to see a cardiologist for further testing.
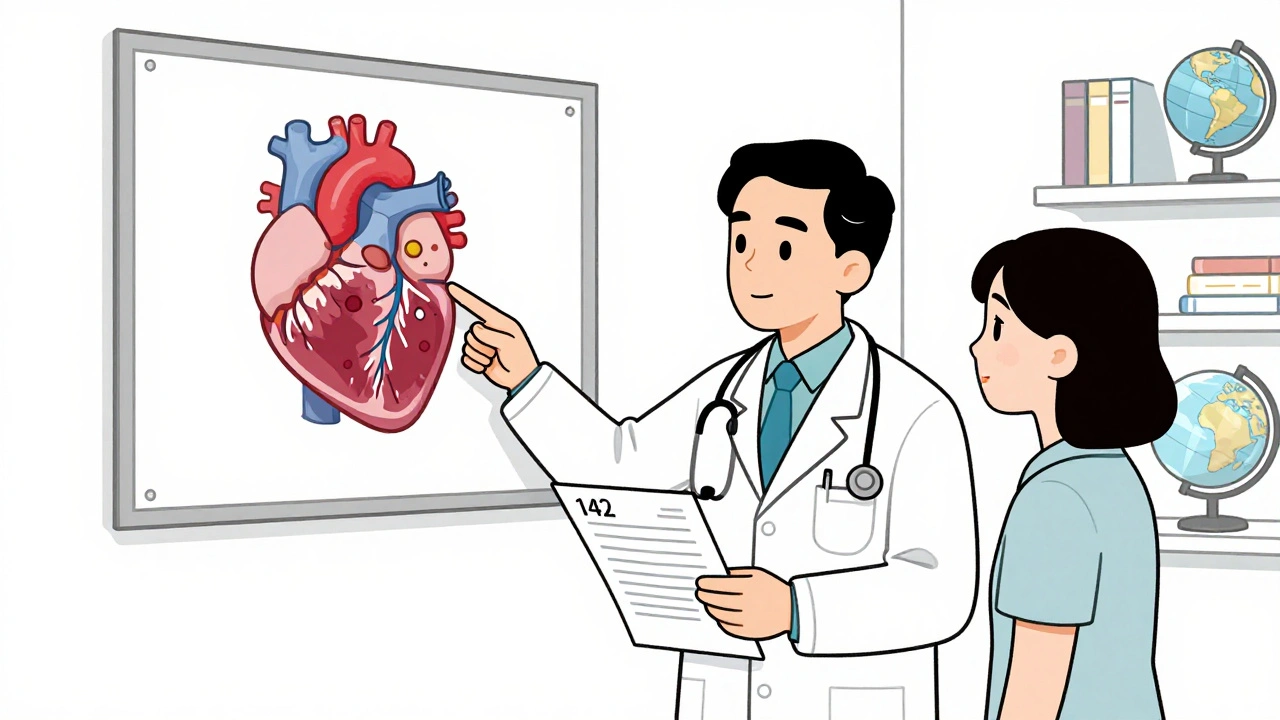
One man in his 50s from Melbourne had a score of 142. His doctor had recommended a statin for years. He ignored it. After seeing his score, he quit smoking, started walking daily, and began taking a statin. He told his doctor: “I didn’t believe I was at risk until I saw the numbers.”
Cost, Coverage, and Access
The scan typically costs between $100 and $300 out-of-pocket. Insurance coverage is spotty. Medicare doesn’t cover it. Some private insurers do - especially if your doctor documents your intermediate risk. Others won’t touch it.
That’s the biggest barrier. Despite strong evidence, only 15% of eligible patients get tested. Many doctors don’t bring it up. Many patients don’t know to ask.
But the trend is changing. In 2022, over 2 million coronary calcium scans were done in the U.S. - up 17% from the year before. AI is now helping reduce radiation doses by 40%, making it safer. More guidelines are expanding who qualifies.
Is It Worth It?
If you’re in your 40s to 70s and have risk factors - even mild ones - this test gives you information no blood test or physical can. It turns abstract risk into a concrete number. And for many, that number is the wake-up call they need.
It’s not about fear. It’s about control. Knowing your calcium score lets you act - before a heart attack forces you to.
Can a coronary calcium score detect heart blockages?
No. A coronary calcium score only detects calcified plaque, not the actual narrowing or blockage of arteries. For that, a coronary CT angiography (CCTA) is needed - which uses contrast dye and gives a clearer picture of blood flow. But calcium scoring is better for early detection of disease before blockages form.
Is the radiation from the scan dangerous?
The radiation dose is low - about 1 to 3 millisieverts, similar to a mammogram or a round-trip flight from Melbourne to Sydney. That’s far less than a standard chest CT (which can be 7-10 mSv). The benefit of catching heart disease early far outweighs the tiny risk from this level of radiation.
Do I need to fast before the test?
You don’t need to fast, but you should avoid caffeine and smoking for at least four hours before the scan. Both can raise your heart rate and make the images blurry. Otherwise, eat and drink normally.
If my score is high, do I need a stent or surgery?
Not necessarily. A high calcium score means you have advanced plaque buildup, but it doesn’t mean your arteries are blocked. Most people with high scores are treated with medication (like statins) and lifestyle changes - not surgery. Stents or bypass are only considered if you have symptoms or a blockage confirmed by another test.
Can I lower my calcium score?
You can’t make existing calcium disappear - once it’s there, it stays. But you can stop it from getting worse. Statins, healthy eating, exercise, and quitting smoking slow or even halt plaque progression. Some studies show aggressive treatment can reduce the *rate* of calcium growth by up to 50% over five years.
What Comes Next?
If you’re considering a coronary calcium scan, talk to your doctor. Ask if your risk profile makes you a candidate. If they say no, ask why. If they’re unsure, ask for a referral to a preventive cardiology clinic.
Don’t wait for chest pain. Don’t wait for a heart attack. The best time to find out about plaque in your arteries is before you feel anything. This test doesn’t promise a longer life - but it gives you the power to make choices that might get you there.




December 10, 2025 AT 20:22
I got mine done last year after my doc pushed it. Score was 89. Didn't think I was at risk since I'm not fat and don't smoke. Turns out my dad had a stent at 52. Scared the hell out of me. Started walking 5 miles a day and switched to olive oil. No statin yet but I'm watching my numbers like a hawk.
Best $150 I ever spent.