When your kidneys fail, life doesn’t stop-but it changes. End-stage renal disease (ESRD) means your kidneys have lost about 90% of their ability to clean your blood. Without treatment, toxins build up, fluids swell your body, and your heart struggles. The choices are clear: dialysis, transplant, or death. But between those options, there’s a world of difference in how you live, not just how long you live.
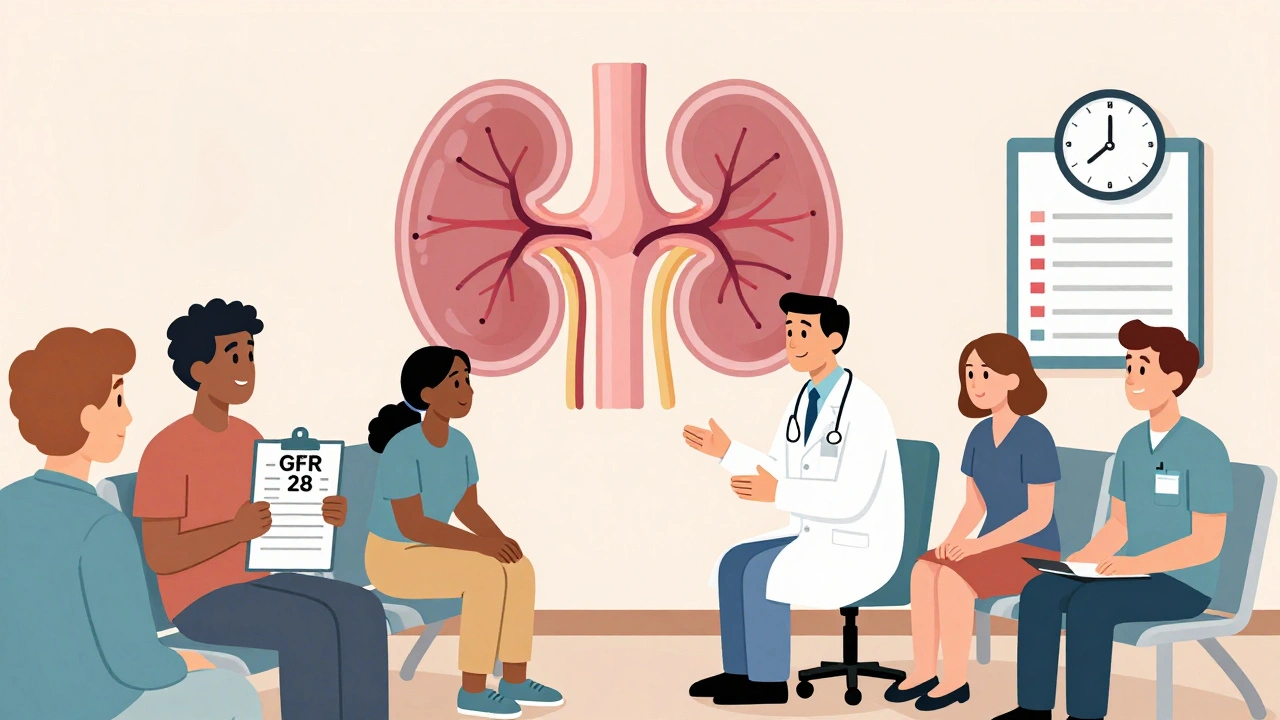
What Exactly Is End-Stage Renal Disease?
ESRD isn’t just "bad kidney function." It’s the point where your kidneys can’t keep up with the basics anymore. Doctors measure this with something called the glomerular filtration rate, or GFR. When it drops below 15 mL/min/1.73 m², you’re in ESRD. That’s not a slow decline-it’s a complete breakdown. Your body can’t remove waste, balance salts, or control blood pressure on its own anymore.The main culprits? Diabetes and high blood pressure. Together, they cause over 70% of ESRD cases in the U.S. Other causes include polycystic kidney disease, lupus, and long-term drug or toxin exposure. It’s not rare. About 786,000 Americans have ESRD. Most are on dialysis. Fewer than a third have a working transplant. And every month, 3,000 more people join the transplant waiting list.
Dialysis: Keeping You Alive, But at What Cost?
Dialysis is life support for your kidneys. There are two main types: hemodialysis and peritoneal dialysis.Hemodialysis means your blood is pumped out of your body, cleaned through a machine, and returned. You do this three times a week, for about four hours each session. That’s 12 to 16 hours a week just sitting in a chair, hooked up to tubes. Add travel time, prep, and recovery, and you’re looking at 20+ hours. Many patients feel exhausted afterward. Some can’t work full-time. Others skip sessions because they’re too tired.
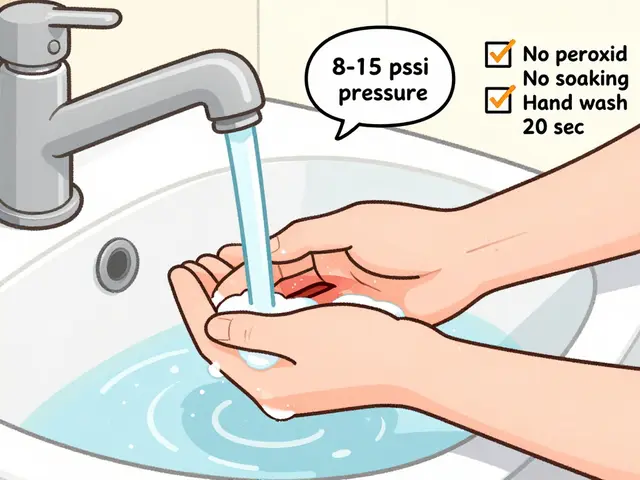
Peritoneal dialysis happens at home. A fluid is swapped in and out of your belly through a catheter. You do it daily-either four times manually or overnight with a machine. It’s more flexible, but you need space, cleanliness, and discipline. Infections are a real risk. One bad episode can land you in the hospital.
And then there are the numbers you can’t ignore. Blood tests are constant. Phosphate must stay between 3.5 and 5.5 mg/dL. Calcium below 9.5 mg/dL. Parathyroid hormone? Under 2 to 9 times the normal range. You’ll take pills with every meal-phosphate binders, vitamin D, iron, blood pressure meds. Diet is strict: no bananas, no potatoes, no processed food, no soda. Fluids? Limited. Salt? Forbidden. It’s a life of constant calculation.
And the cost? Medicare spends $35.4 billion a year on ESRD care. That’s 7.2% of its entire budget-for just 1% of its patients. You’re not just managing a disease. You’re managing a system.
Kidney Transplant: The Better Option, If You Can Get It
If dialysis keeps you alive, a kidney transplant helps you live.Studies show transplant recipients have a 68% lower risk of dying than those on dialysis. Five-year survival? 83% for transplant patients. For dialysis patients? Just 35%. That’s not a small difference-it’s life versus survival.
Transplant patients don’t need to spend hours hooked to machines. They can travel. Work. Eat more freely. Sleep through the night. One 2021 study found transplant patients scored 28.7 points higher on quality-of-life surveys than dialysis patients. That’s like going from feeling broken to feeling normal.
There are two kinds of transplants: from a living donor or a deceased donor. Living donor transplants have better outcomes. One-year graft survival? 95.5%. Five-year? 86%. Deceased donor? 93.7% and 78.5% respectively. The difference isn’t just numbers-it’s time. A transplant from a living donor can happen before dialysis even starts. That’s called a preemptive transplant. Only 5% of people who start dialysis ever get one. Why? Because the system doesn’t push for it.
But here’s the catch: you need to be healthy enough to get one. If you’re over 75 with heart disease, active cancer, dementia, or uncontrolled addiction, you’re not a candidate. Even if you’re eligible, the wait is long. The national waiting list has over 90,000 people. Only 27,000 transplants happen each year. That’s a three- to four-year wait, on average.
And then there’s the cost of staying alive after the transplant: immunosuppressants. These drugs stop your body from rejecting the new kidney. But they’re expensive-$1,500 to $2,500 a month. You take them for life. And they come with trade-offs: higher risk of infections, skin cancer, and other illnesses. You’ll need regular blood tests, doctor visits, and vigilance.

Why So Few People Get Transplants-And What’s Being Done
You’d think everyone who could get a transplant would get one. But that’s not the case.Black patients are less likely to be referred for transplant evaluation-even when their medical needs are the same. A study called RaDIANT found that after training doctors and educating patients, transplant referrals among Black patients jumped 40%. That’s progress. But it took a targeted program to fix a broken system.
Medicare doesn’t cover transplant evaluation until you’ve been on dialysis for three months. That delays everything. The Kidney Care Choices Model, launched in 2022, is trying to change that. It pays providers to refer patients earlier-to when GFR drops below 30 mL/min/1.73 m². That’s not ESRD yet. That’s stage 4 kidney disease. But it’s the sweet spot to start the transplant process.
There’s also a push to use more expanded criteria donors-older donors, donors with high blood pressure, donors who’ve had a stroke. Since 2017, this has increased the donor pool by 15%. It’s not perfect, but it saves lives.
And yet, the gap remains. The waiting list grows by 3,000 people every month. The supply hasn’t kept up. That’s why living donation is so critical. A single living donor can save two lives-the recipient, and the person who would have waited next in line.
Quality of Life: It’s Not Just About Living Longer
People talk about survival rates. But what matters more is how you feel day to day.Dialysis patients often describe their lives as being on hold. They plan everything around appointments. They can’t eat what they want. They can’t drink what they want. They’re tired. They’re anxious. They’re isolated. Many say they feel like a burden.
Transplant patients don’t have those same restrictions. They can eat a banana. Drink a glass of water. Go on a spontaneous trip. Sleep without alarms. They still have to take pills. Still have to go to appointments. Still worry about rejection. But they’re not chained to a machine.
And here’s something most people don’t realize: transplant patients have 50% fewer hospitalizations than dialysis patients. Fewer infections. Fewer ER visits. Fewer days lost to illness. That’s not just better quality of life-it’s less stress on families, less cost to the system, more time with loved ones.
One woman in Melbourne, who got a kidney from her brother in 2023, told me she finally felt like herself again. She started walking her dog every morning. She went back to painting. She didn’t realize how much she’d missed those things until she could do them again.
What You Can Do If You or Someone You Love Has ESRD
If you’re diagnosed with advanced kidney disease, don’t wait. Start thinking about transplant now.- Ask your nephrologist to refer you to a transplant center when your GFR drops below 30.
- Ask if you’re eligible for a preemptive transplant.
- Encourage family and friends to get tested as potential living donors. It’s safe. It’s simple. It saves lives.
- Learn about home dialysis options. They’re more flexible than in-center treatments.
- Join a patient support group. You’re not alone.
If you’re on dialysis, don’t give up on the idea of a transplant. Many people get transplants after years on dialysis. The key is to stay healthy enough to qualify. Eat well. Control your blood pressure. Don’t smoke. Take your meds. Keep moving.
And if you’re healthy, consider becoming a living donor. One kidney can give someone back their life. And you? You’ll live just fine with one.
What’s Next for ESRD Care?
The NIH is investing $157 million through 2026 to study personalized kidney treatments. That could mean better drugs, fewer side effects, and longer-lasting transplants. There’s also growing interest in bioengineered kidneys and artificial devices that mimic kidney function. But those are years away.Right now, the best thing we have is a working kidney from a living donor. It’s not perfect. It’s not easy. But it’s the closest thing to a cure we’ve got.
ESRD doesn’t have to mean the end of a good life. It can be the start of a new one-if you know the options, act early, and don’t let fear or bureaucracy stop you.
Can you live a normal life on dialysis?
You can live, but not always normally. Dialysis requires strict scheduling, dietary limits, and fluid control. Many patients feel fatigued, isolated, or restricted. While some continue working and socializing, the physical and emotional toll is high. Quality of life scores for dialysis patients are significantly lower than for transplant recipients.
How long is the wait for a kidney transplant?
The average wait is four years, but it varies widely. It depends on blood type, tissue match, location, and how sick you are. Some wait less than a year; others wait over a decade. Living donor transplants can happen immediately if a match is found, bypassing the waiting list entirely.
Can anyone get a kidney transplant?
No. Candidates must be healthy enough to survive surgery and lifelong immunosuppression. Contraindications include advanced age with severe heart disease, active cancer within the past 2-5 years, dementia, uncontrolled mental illness, or ongoing substance abuse. Each case is evaluated individually by a transplant team.
What are the risks of a kidney transplant?
The biggest risk is rejection-your immune system attacking the new kidney. That’s why you take immunosuppressant drugs for life. These drugs increase your risk of infections, certain cancers, high blood pressure, and diabetes. Other risks include surgical complications, blood clots, and side effects from medications. But for most, the benefits far outweigh the risks.
Is it safe to be a living kidney donor?
Yes, for healthy individuals. Living donation is a safe, well-studied procedure. Donors live just as long as people with two kidneys. The risk of kidney failure after donation is less than 1%. Most donors return to normal activities within 4-6 weeks. Long-term studies show no significant increase in health problems for donors.
Does Medicare cover kidney transplants and dialysis?
Yes. Medicare covers dialysis starting in the fourth month of treatment. It also covers transplant surgery, immunosuppressant drugs for 36 months after transplant, and related care. After 36 months, you may need other insurance or pay out-of-pocket for anti-rejection drugs unless you qualify for Medicaid or other programs.






December 4, 2025 AT 23:14
Man, the GFR cutoff at 15 is such a brutal line in the sand. It’s not like you slowly fade out-you hit a wall and suddenly your body’s just a leaky faucet the machines have to patch. And the phosphate binders? I swear, those little pills are the unsung villains of ESRD. You eat a banana, boom, you’re in the red zone. It’s not just medical-it’s psychological warfare.