When you’re scheduled for surgery, the last thing you want is for a drug you took years ago to cause a life-threatening reaction in the operating room. Yet every year, preventable drug reactions during surgery happen - not because doctors are careless, but because the information never made it from patient to provider. If you’ve ever had a bad reaction to a medication, whether it was a rash, nausea, trouble breathing, or worse, communicating this clearly before surgery isn’t just advice - it’s a safety requirement.
Why This Matters More Than You Think
About 1 in every 10,000 to 20,000 anesthesia cases results in a severe allergic reaction. That sounds rare, but when it happens, it can be fatal. And here’s the real problem: most of these reactions are avoidable. A 2022 NIH study found that drug-related complications account for 4.5% of all surgical errors, and allergic reactions make up 1.1% of anesthesia-related deaths. These aren’t accidents. They’re communication failures. The good news? Hospitals that use standardized protocols reduce these errors by up to 37%. That means if you take the right steps before your surgery, you’re not just helping yourself - you’re helping the whole system work better.What Counts as a Drug Reaction?
Not every bad side effect is an allergy. Many people say they’re “allergic” to a drug when they actually had a side effect - like nausea from codeine, dizziness from blood pressure meds, or stomach upset from ibuprofen. True allergies involve your immune system. Signs include:- Hives, swelling (especially lips or throat)
- Difficulty breathing or wheezing
- Rapid drop in blood pressure
- Loss of consciousness
- Anaphylaxis (a full-body reaction that can kill in minutes)
What to Document Before Your Surgery
Don’t just say “I’m allergic to penicillin.” That’s not enough. You need details. Here’s what you should write down before your pre-op appointment:- Drug name: Generic or brand? (e.g., “morphine” or “MS Contin”)
- Reaction: What happened? (e.g., “swollen tongue, couldn’t breathe”)
- Timing: How soon after taking it? (e.g., “within 5 minutes”)
- Treatment: Did you need epinephrine, steroids, or hospital care?
- Alternative drugs: Did your doctor ever say what you could safely take instead?
Don’t Forget the Extras
People often forget about non-prescription stuff. But here’s what else can trigger reactions:- Over-the-counter painkillers (NSAIDs like ibuprofen, naproxen)
- Herbal supplements (st. john’s wort, ginkgo, garlic)
- Vitamins and minerals (especially high-dose vitamin E or K)
- Latex (yes, it’s a drug reaction too - many anesthetics come in latex-containing packaging)
- Food or drinks taken close to surgery (some meds interact with grapefruit juice, alcohol, or even large meals)
Who Should You Tell - And When?
This isn’t just a question for your surgeon. You need to tell everyone involved:- Your primary doctor: Tell them as soon as you schedule surgery.
- The pre-op nurse: They’ll ask you to fill out a form. Don’t rush this. Read every question.
- The anesthesiologist: You’ll meet them the day of surgery. If they don’t ask about your history, bring it up yourself.
- The pharmacist: Many hospitals now have pharmacists review your meds 24 hours before surgery. If you don’t see them, ask if they’ve checked your file.
What If You Can’t Remember the Exact Drug?
It’s common. People forget names, especially if it happened years ago. Here’s what to do:- Think about the reason you took it. Was it for a toothache? A back injury? An infection?
- Recall the form. Was it a pill, shot, IV, or patch?
- Remember the setting. Was it in a hospital? ER? Dentist’s office?
- Check old medical records. Most hospitals let you request your history online.
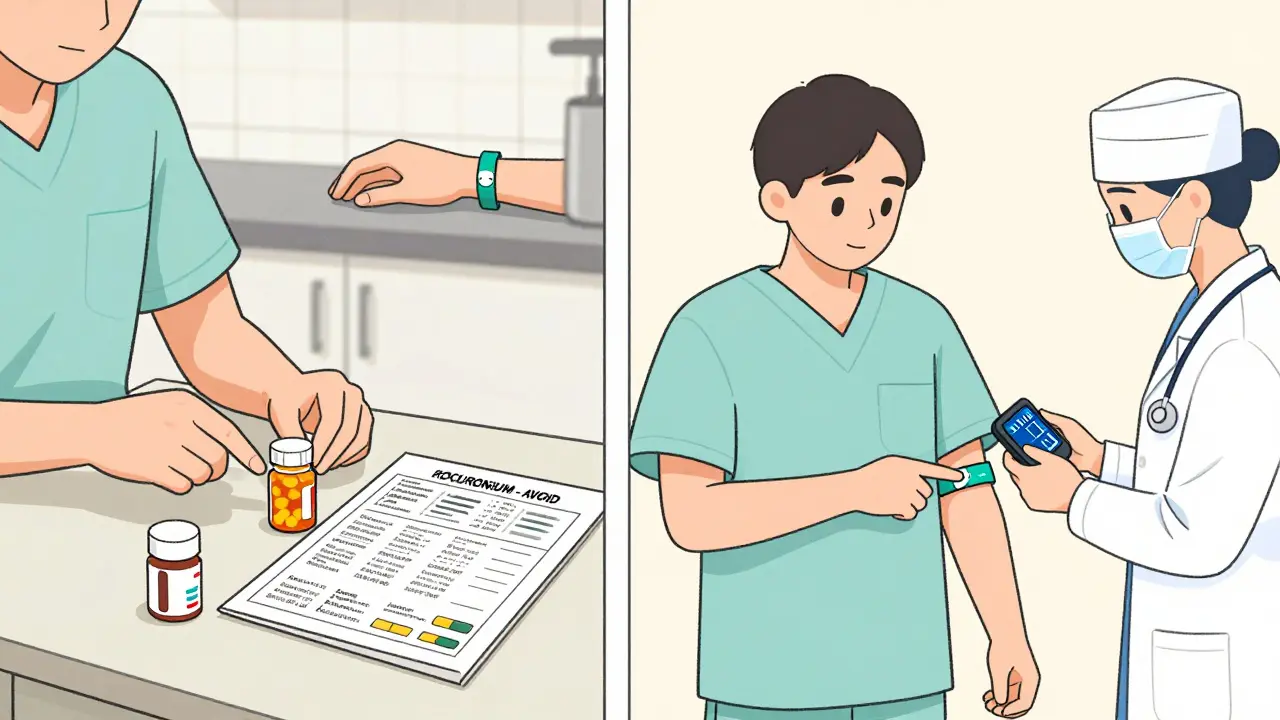
What Happens After You Tell Them?
Once you report a reaction, the hospital should:- Put a clear alert in your electronic medical record
- Flag your file so no one gives you that drug again
- Consult an allergist if the reaction was severe
- Offer you an allergy card or wristband (many hospitals provide these)
Red Flags to Watch For
Even with good protocols, things go wrong. Here’s what to watch for:- They don’t ask about your meds - or rush you through the form.
- They say, “We’ll just avoid penicillin,” but don’t ask about other drugs.
- You’re given a drug you’ve reacted to before - even if it’s called something different.
- No one reviews your file the day before surgery.
Real Stories - What Went Right and Wrong
One patient, a 58-year-old woman in Melbourne, had a severe reaction to succinylcholine during a 2017 surgery. She didn’t remember the name, but she remembered her body went rigid and she couldn’t breathe. When she scheduled a knee replacement in 2025, she brought a handwritten note: “Reaction to muscle relaxant - 2017. Breathing stopped. IV epinephrine. Never again.” The anesthesiologist immediately checked her file, confirmed the history, and switched to a safer muscle relaxant. She had a smooth surgery. Another patient, a 42-year-old man, told his surgeon he was allergic to codeine. He said he got nauseous. The team assumed it was just a side effect. They gave him hydrocodone - a close cousin - during his hernia repair. He vomited violently for hours after. It wasn’t an allergy, but it was still preventable. The team didn’t dig deep enough. The difference? One patient gave specifics. The other gave a vague answer. Details save lives.What You Can Do Today
You don’t need to wait for your surgery date to act. Here’s your checklist:- Write down every drug you’ve ever had a bad reaction to - even if you think it’s not important.
- For each, note the symptoms, timing, and treatment.
- Collect pill bottles or pharmacy records if you can.
- Call your doctor’s office and ask if they have a pre-op medication form - fill it out now.
- Ask for an allergy wristband or card - many hospitals give them for free.
- Bring your list to every pre-op appointment. Don’t assume they’ve seen it before.
What If You’re Having Emergency Surgery?
In emergencies, there’s no time for paperwork. That’s why it’s so important to wear a medical alert bracelet or carry a card in your wallet. If you’ve had a serious drug reaction, get one. You can order them online for under $10. Some hospitals give them out for free if you’ve had a reaction on their watch. If you’re unconscious and brought in for emergency surgery, your best chance is having that info visible. Paramedics and ER staff are trained to look for it.Final Thought: You’re Not Just a Patient - You’re a Partner
Doctors and nurses want to keep you safe. But they can’t read your mind. If you’ve had a bad drug reaction, you hold the key to avoiding another one. Don’t downplay it. Don’t assume they’ll find it in your file. Don’t wait until the last minute. The best time to talk about your drug history? Now. Before you even schedule the surgery. Because when it comes to your safety, silence isn’t golden - it’s dangerous.What if I think I’m allergic to a drug but I’m not sure?
It’s better to report it than to leave it out. Many people confuse side effects with allergies. If you had nausea, dizziness, or a rash after a drug, tell your care team. They can determine if it was a true allergy or a side effect. Even if it’s not an allergy, they may still avoid that drug to keep you comfortable.
Can I be tested for drug allergies before surgery?
Yes - but only for certain drugs and only if the reaction was severe. Skin tests or blood tests are available for antibiotics like penicillin, muscle relaxants, and some anesthetics. However, testing takes time and isn’t always accurate. Most hospitals recommend avoiding the drug entirely unless testing is done and confirmed safe. If you’ve had a life-threatening reaction, you’ll likely be referred to an allergist within 4-8 weeks after the event.
Do I need to tell my dentist if I’ve had a reaction to anesthesia?
Absolutely. Dental procedures often use local anesthetics, sedatives, or antibiotics that can trigger reactions. A reaction to lidocaine or epinephrine during a dental visit is just as serious as one during major surgery. Always inform any healthcare provider who gives you medication - not just surgeons.
What if I’m on long-term medications like blood thinners?
Blood thinners like warfarin, aspirin, or clopidogrel require special management before surgery. Stopping them too early can cause clots; stopping too late can cause bleeding. Your surgeon and pharmacist will work together to time the stoppage correctly. For example, ticagrelor (Brilinta) must be stopped 3-5 days before surgery, while prasugrel needs 7 days. Never stop these on your own - always follow your doctor’s plan.
Can I bring someone with me to pre-op to help remember things?
Yes, and you should. Memory can be unreliable, especially under stress. Having a family member or friend with you helps ensure nothing gets missed. They can also ask questions you might forget, like “Did you check if he’s allergic to latex?” or “What did we say about the herbal tea he takes daily?”





January 7, 2026 AT 14:03
my cousin had a rash from amoxicillin and forgot to tell the doc-ended up in ICU. don’t downplay rashes. just say it.