The U.S. Food and Drug Administration doesn’t just approve drugs and medical devices - it keeps watching them after they’re on the market. That’s where MedWatch comes in. It’s not a fancy lab or a high-tech machine. It’s a simple, powerful system that lets doctors, patients, and manufacturers report problems with medicines, devices, and even cosmetics. And those reports? They’re what trigger recalls, label changes, and sometimes life-saving warnings.
What Exactly Is MedWatch?
MedWatch, officially called the FDA Safety Information and Adverse Event Reporting Program, started in 1993. It’s the FDA’s main tool for tracking safety issues after a product is sold to the public. Think of it like a national early warning system. If a new painkiller causes unexpected heart rhythms in a few patients, or a pacemaker wire breaks during routine use, someone needs to tell the FDA. That’s MedWatch’s job.
It doesn’t just collect reports - it also sends out alerts. When a serious risk is found, the FDA uses MedWatch to email doctors, post updates online, and notify the public. It’s a two-way street: you report problems, and the FDA tells you what they’re doing about them.
Who Can Report and How?
Anyone can file a MedWatch report - patients, caregivers, nurses, pharmacists, or doctors. You don’t need to be a medical expert. The online form at www.fda.gov/medwatch walks you through it step by step. You’ll need basic info: the patient’s age and sex, what product was involved (brand name, lot number if possible), when the problem happened, what symptoms occurred, and whether the person got better or worse.
For healthcare providers, the form is called FDA 3500. For manufacturers and hospitals, it’s FDA 3500B - a legal requirement. Companies must report deaths or serious injuries linked to their products within 30 days. For life-threatening events, they have just five workdays.
Still, most reports come from people outside the industry. In 2022, 42% of reports came from patients and family members. That’s huge. It means everyday users are helping catch problems that even clinical trials missed.
What Gets Reported?
MedWatch doesn’t just track side effects. It covers:
- Unexpected reactions to prescription or over-the-counter drugs
- Device failures - like a glucose monitor giving wrong readings
- Contaminated products
- Incorrect labeling or packaging
- Use errors - like a patient taking two doses by accident because the instructions were unclear
- Problems with biologics, vaccines, or even hemp-based products
You don’t have to prove the product caused the issue. If you suspect it might have, report it. The FDA’s analysts will sort out the connection later.
What Happens After You Submit?
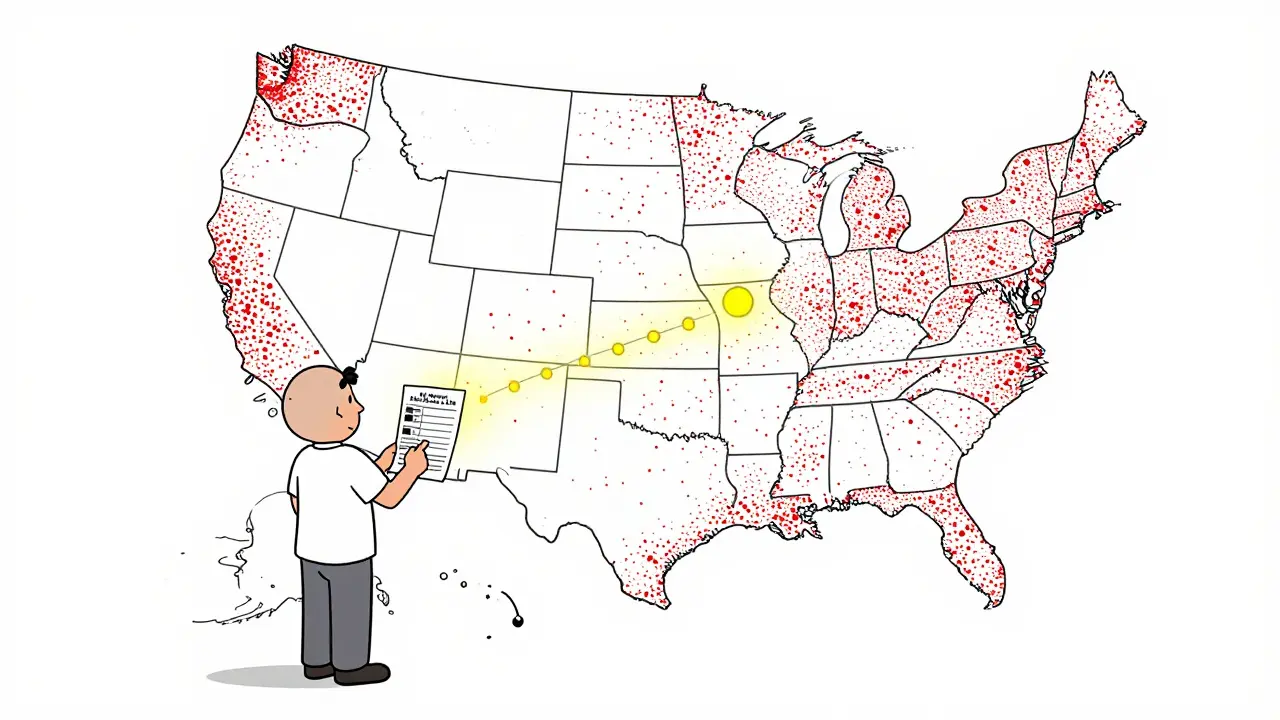
Every report goes into the FDA Adverse Event Reporting System (FAERS), a database with over 28 million entries. That’s not just a pile of paperwork - it’s a treasure trove of real-world data.
Software tools scan for patterns. If 50 people report the same rare liver injury after taking a new diabetes drug, the system flags it. Statisticians use methods like the Proportional Reporting Ratio (PRR) and Bayesian algorithms to spot signals hiding in the noise. About 5,000 potential safety signals are analyzed each year.
When a real risk is confirmed, the FDA can:
- Update the drug’s label with new warnings
- Send a safety communication to all doctors
- Require a Risk Evaluation and Mitigation Strategy (REMS)
- Order a recall
Take the 2021 recall of Allergan’s textured breast implants. MedWatch reports showing a link to a rare cancer called BIA-ALCL helped the FDA act within 45 days. That’s fast - and it saved lives.
Why Underreporting Is the Biggest Problem
Here’s the catch: most problems never get reported. Experts estimate only 1% to 10% of adverse events make it into MedWatch. Why?
- Doctors are busy. Filling out a report can take 15 to 20 minutes - time most don’t have.
- Patients don’t know how. A 2022 survey found 68% of consumers gave up because the form felt too technical.
- Some think, “It’s probably just a coincidence.” But that’s exactly when you should report it.
One oncologist at MD Anderson reported unusual immune reactions to Keytruda in 2019. Her report led to a formal FDA warning within 90 days. But how many similar cases went unreported because no one took the time?
The Government Accountability Office called underreporting a “major limitation.” Without enough data, the FDA can’t see the full picture. A drug might seem safe - until thousands more reports come in years later.
How Technology Is Changing MedWatch
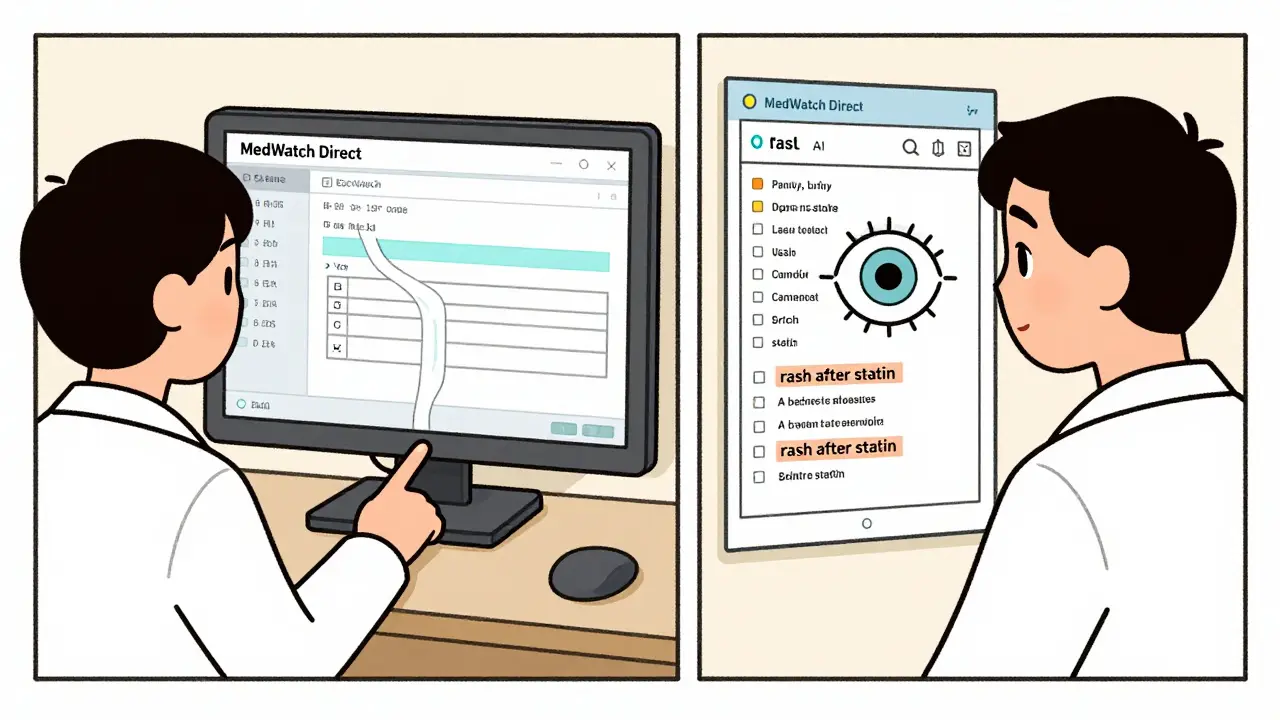
The FDA knows the system needs upgrading. In 2023, they launched MedWatch Direct - a new API that connects directly to electronic health records. Instead of manually typing a report, a doctor can click a button in Epic or Cerner when a patient has a reaction. The system auto-fills the form with lab results, medication history, and diagnosis codes.
By 2024, the FDA plans to use AI to scan clinical notes for hidden safety signals. If a doctor writes, “Patient developed severe rash after starting new statin,” the AI will pull that out and turn it into a structured report. Early tests show this could boost reporting by 25%.
Blockchain is coming too - to verify that reports aren’t fake. And by 2025, the FDA hopes to cut analysis time from weeks to hours using smarter algorithms.
But tech alone won’t fix the core problem: people still need to speak up.
What Makes MedWatch Different?
Other countries have similar systems - like EudraVigilance in Europe or Canada Vigilance. But MedWatch stands out because it’s open to the public. Anyone with a phone or computer can file a report. That’s rare. In most places, only doctors or companies can report.
It also combines reporting and communication. You don’t just send data - you get updates. The FDA sends out email alerts, posts safety notices, and even updates its website daily. That transparency builds trust.
Real Impact: When Reports Changed Everything
Here are three real cases where MedWatch made a difference:
- Avandia (rosiglitazone) - Reports of heart attacks led to label changes and usage restrictions in 2010.
- Thimerosal in vaccines - Public concern triggered by MedWatch reports led to its removal from most childhood vaccines by 2001.
- Elaprase (idursulfase) - Reports of severe allergic reactions prompted the FDA to require pre-treatment with antihistamines.
These weren’t discovered in clinical trials. They were found because someone - a nurse, a patient, a pharmacist - took the time to report.
How to File a Good Report
Not all reports are useful. The FDA says a strong report includes:
- Exact product name and manufacturer
- Product lot number or expiration date (if available)
- Patient’s age and sex
- When the reaction started (e.g., “2 days after first dose”)
- Exact symptoms (don’t say “felt bad” - say “chest pain, shortness of breath, dizziness”)
- What happened after - did the person go to the ER? Did symptoms improve after stopping the drug?
- Other medications or conditions the patient had
Use the FDA’s free online decision tree tool. It helps you decide if your issue is reportable. It cut wrong submissions by 38% in 2023.
What If You Don’t Report?
If you ignore a bad reaction, you’re not just protecting yourself - you’re protecting others. A single report might seem small. But if 10 people have the same issue and none report it, the FDA never sees the pattern. That drug stays on shelves. More people get hurt.
And when a recall finally happens? It’s often because one person spoke up - and their report was the first in a chain that led to action.
Final Thoughts
MedWatch isn’t perfect. It’s slow in some ways. It’s underfunded. Too many reports are incomplete. But it’s the best tool we have to catch hidden dangers after a product is out in the wild.
It’s not about blaming companies or doctors. It’s about collective responsibility. If you take a new medicine and feel something off - don’t assume it’s just you. Don’t wait for someone else to report it. Take five minutes. Fill out the form. Your report could be the one that saves someone else’s life.
The system only works if we use it. And right now, most of us aren’t.
Is MedWatch only for prescription drugs?
No. MedWatch accepts reports for prescription drugs, over-the-counter medicines, vaccines, medical devices (like pacemakers or glucose monitors), biologics, cosmetics, and even hemp-derived products. If it’s regulated by the FDA and something went wrong, you can report it.
Do I need to prove the product caused the problem to report it?
No. You don’t need to be certain. The FDA’s job is to investigate causality. If you suspect a product might be involved - even if you’re not sure - report it. Many safety signals start with just one or two vague reports.
How long does it take for the FDA to act on a report?
It varies. For serious, life-threatening events, the FDA can issue a warning in days. For slower-developing patterns, it can take months or even years to confirm a trend. A single report rarely triggers immediate action - it’s the volume and consistency of similar reports that matter.
Can I report a problem anonymously?
Yes. You can file a report without giving your name or contact info. However, if you leave your details, the FDA may follow up for more information, which can help them better understand the issue.
Are reports from patients taken seriously?
Absolutely. In fact, patient reports are often the first to catch rare or delayed side effects that clinical trials miss. About 42% of all reports in 2022 came from patients and caregivers. The FDA trains analysts to treat every report seriously, regardless of who submitted it.
What if I report something and nothing happens?
That doesn’t mean your report didn’t matter. The FDA reviews every report, even if no public action follows. Your report adds to the database. It might help in the future when another case shows up. Safety signals often emerge only after dozens or hundreds of similar reports pile up.
If you’ve ever taken a medication and wondered, “Is this normal?” - don’t wonder alone. Report it. The system is simple. The impact? Potentially huge.




December 28, 2025 AT 23:08
MedWatch is a joke. I've reported three adverse reactions over the years. Zero follow-up. Zero acknowledgment. Just a confirmation email that disappears into the void. The FDA doesn't care. They're too busy approving drugs with 3-month trials and calling it 'emergency use'.