Opioid Safety Risk Calculator
This tool estimates your risk of opioid-induced sleep apnea based on your daily dose. According to the article, patients taking 100 MME or more per day are 4 times more likely to develop severe central sleep apnea.
When you take an opioid for pain, you’re not just blocking pain signals-you’re also slowing down your breathing, especially when you’re asleep. This isn’t just a side effect. It’s a life-threatening interaction that millions of people don’t even know they’re at risk for. If you or someone you care about is on long-term opioid therapy, understanding how these drugs affect sleep and breathing could literally save a life.
How Opioids Quiet Your Breathing While You Sleep
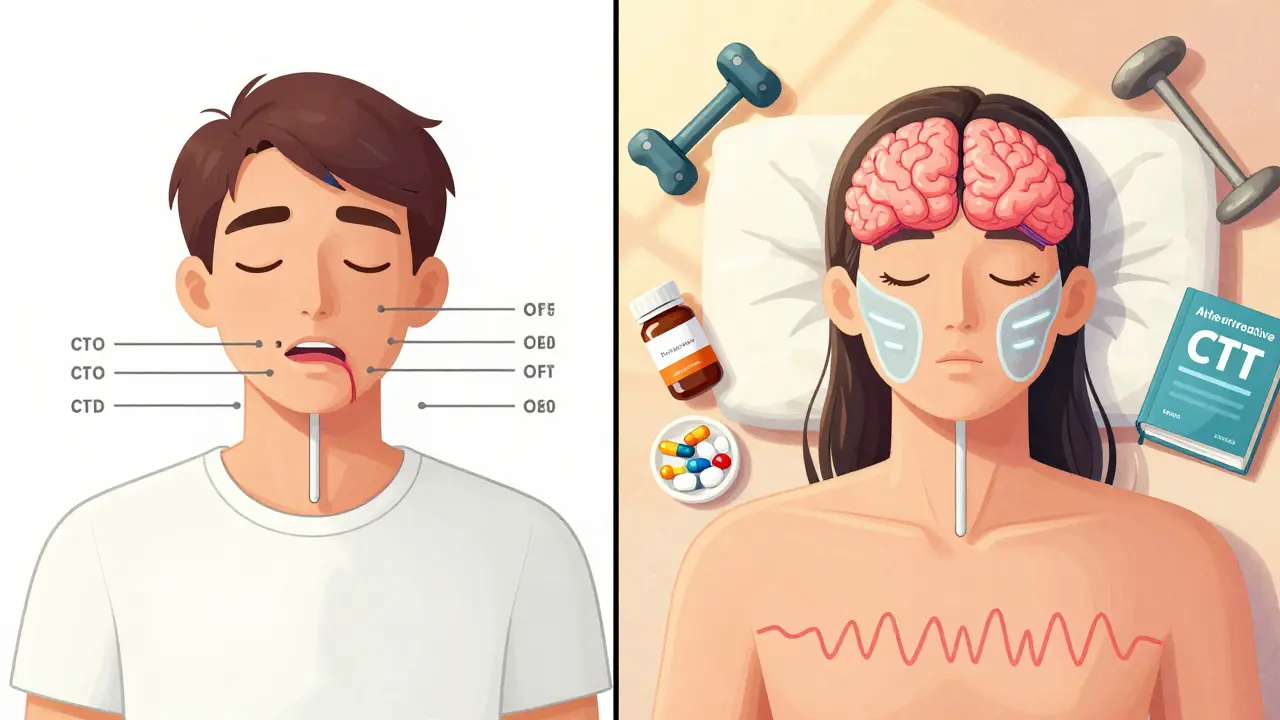
Opioids like oxycodone, hydrocodone, fentanyl, and morphine work by binding to μ-opioid receptors in the brain. These receptors are found in areas that control pain, reward, and-critically-breathing. The brainstem, specifically the parabrachial complex and the pre-Bötzinger complex, is where breathing rhythm is generated. When opioids activate receptors in these regions, they disrupt the natural cycle of inhale and exhale.
Instead of smooth, steady breaths, breathing becomes irregular. Exhalation stretches out, sometimes for seconds longer than normal. In severe cases, breathing stops entirely-what’s called apnea. Research shows that opioids can increase expiration time by up to 200%, leading to prolonged pauses between breaths. At high doses, this can result in 30 or more breathing pauses per hour during sleep, which is the clinical definition of severe central sleep apnea.
It’s not just the brainstem. Opioids also reduce activity in the hypoglossal nerve, which controls the tongue and upper airway muscles. When these muscles relax too much, the airway collapses-like a straw pinching shut. This is why many people on opioids experience both central sleep apnea (the brain stops signaling to breathe) and obstructive sleep apnea (the airway physically closes). The combination is deadly.
Why Sleep Makes It Worse
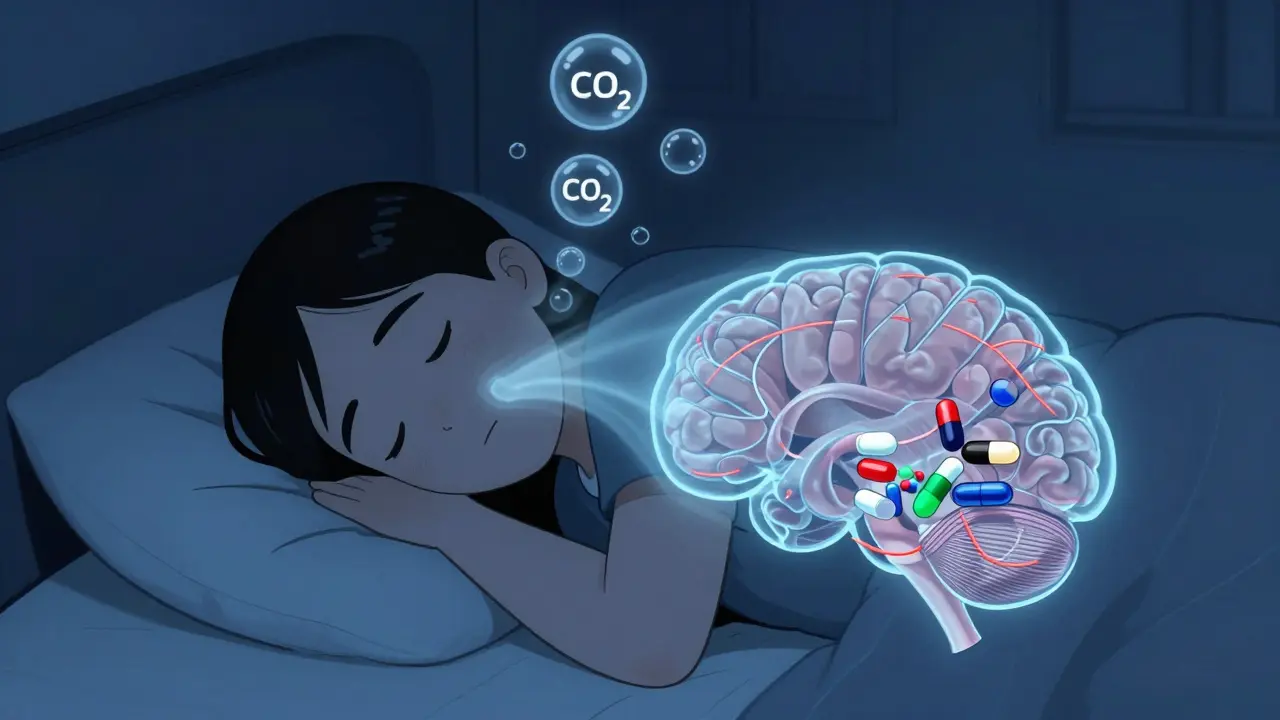
During wakefulness, your brain has backup systems to keep you breathing. You’re alert. Your body is actively monitoring oxygen and carbon dioxide levels. But when you fall asleep, those backup systems turn off. That’s normal. The problem is, opioids remove the very last line of defense: the brain’s ability to detect low oxygen and trigger a gasp.
Studies show that opioid users often have reduced sensitivity to rising carbon dioxide levels-a condition called blunted chemoreflex. Normally, when CO2 builds up, your body wakes you up to breathe. But with opioids, that alarm system is muted. You might go minutes without breathing and never stir. This is why most opioid-related deaths happen at night, often alone in bed.
Adding to the danger, opioids also mess with sleep architecture. They reduce deep, restorative slow-wave sleep by 20-30% and increase the lightest stage of sleep (Stage 1) by 15-25%. This means you’re not just breathing poorly-you’re not sleeping well either. The result? Constant fatigue, morning headaches, and a vicious cycle where people take more opioids to cope with daytime exhaustion, worsening the problem.
Who’s Most at Risk?
Not everyone on opioids develops sleep apnea. But certain factors raise the risk dramatically:
- Using high doses: People taking 100 morphine milligram equivalents (MME) or more per day are 4 times more likely to develop severe central sleep apnea.
- Already having sleep apnea: If you’ve been diagnosed with obstructive sleep apnea before starting opioids, your risk of dangerous breathing events increases by 50-70%.
- Using other sedatives: Mixing opioids with benzodiazepines (like Xanax or Valium), alcohol, or sleep aids multiplies the risk of fatal respiratory depression by 300-500%.
- Age over 65: Older adults have naturally reduced respiratory drive and slower drug metabolism.
- Obesity: Extra weight around the neck increases airway collapse risk, and opioids worsen it.
- Genetic factors: Some people have variations in the OPRM1 gene that make them more sensitive to opioid-induced respiratory depression.
One study found that 30-40% of chronic opioid users develop clinically significant sleep-disordered breathing. Many report waking up gasping, choking, or feeling like they’ve stopped breathing. In online patient forums, over 60% of users on long-term opioids describe similar experiences. Yet, fewer than 20% of primary care doctors routinely screen for it.

The Silent Danger: Why Pulse Oximeters Can Lie
Many people assume that if their oxygen level looks normal on a pulse oximeter, they’re fine. That’s a dangerous assumption. Oxygen saturation can stay in the 90s or even low 90s for minutes while breathing is dangerously slow or paused. By the time oxygen drops below 90%, brain damage or cardiac arrest can already be underway.
What you can’t see is carbon dioxide buildup. As breathing slows, CO2 accumulates in the blood. This is called hypercapnia. It causes confusion, headaches, drowsiness, and eventually, loss of consciousness. But pulse oximeters don’t measure CO2. Only capnography-the monitoring of exhaled CO2-can catch this early. That’s why hospitals use it for high-risk patients. But outside the hospital? Almost no one does.
What Doctors Should Be Doing
Guidelines from the American Society of Anesthesiologists and the CDC clearly recommend baseline sleep studies for patients starting long-term opioid therapy, especially those with risk factors. Yet, only 15-20% of primary care providers follow this advice.
A simple home sleep apnea test can detect breathing pauses during sleep. It’s non-invasive, affordable, and often covered by insurance. If apnea is found, treatment with CPAP (continuous positive airway pressure) can reduce events by 60-80%. But CPAP alone isn’t enough if the root cause is opioid-induced central apnea.
The real solution? Reducing or eliminating opioids when possible. For chronic pain, alternatives like physical therapy, cognitive behavioral therapy, or non-opioid medications (like gabapentin or duloxetine) should be explored first. If opioids are necessary, the lowest effective dose for the shortest time is the rule.
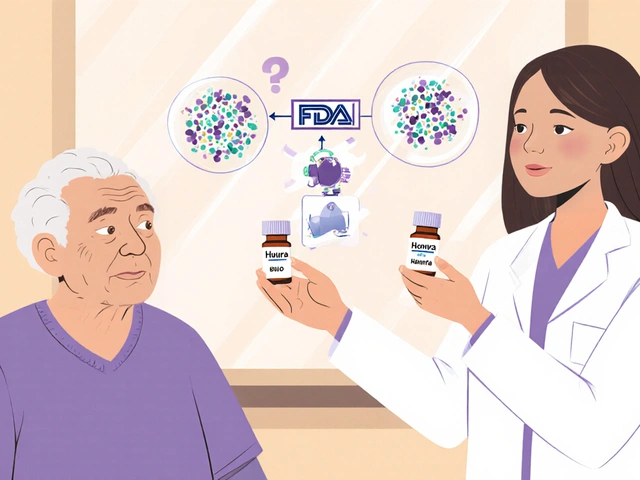
Reversing the Crisis: Naloxone and New Hope
Naloxone (Narcan) is the only FDA-approved drug that can reverse opioid overdose. It works by kicking opioids off the μ-receptors in the brainstem, restoring breathing within minutes. It’s lifesaving-but it’s not perfect. Too much naloxone can trigger severe withdrawal, causing vomiting, seizures, or cardiac stress. Too little, and it doesn’t work.
For people on long-term opioids, having naloxone at home is critical. The CDC recommends it for anyone prescribed 50 MME or more per day, or anyone using opioids with benzodiazepines. Family members should know how to use it. Training is free and available through pharmacies and public health programs.
Beyond naloxone, researchers are developing new drugs that separate pain relief from respiratory depression. One promising approach targets only the pain-related opioid receptors while leaving the breathing-related ones untouched. Early animal studies show these “biased agonists” can deliver 70-80% of the pain relief with only 20-30% of the breathing suppression. Human trials are underway.
Another path involves drugs that stimulate breathing without touching opioid receptors. Ampakines and 5-HT4 agonists have boosted respiratory rate by 40-60% in lab models without reducing pain control. These could one day be added as safety pills alongside opioids.
What You Can Do Today
If you’re on opioids:
- Ask your doctor if you should have a sleep study-even if you don’t snore.
- Never mix opioids with alcohol, benzodiazepines, or sleep meds.
- Keep naloxone at home and teach someone how to use it.
- Watch for signs: waking up gasping, morning headaches, daytime exhaustion, or mood changes.
- Don’t assume your oxygen level is safe just because your pulse oximeter looks normal.
- Explore non-opioid pain management options with your provider.
If you’re caring for someone on opioids:
- Learn the signs of overdose: slow or stopped breathing, blue lips, unresponsiveness.
- Keep naloxone accessible and check its expiration date.
- Encourage them to sleep on their side, not their back.
- Don’t wait for symptoms to get worse-act early.
It’s Not Just About Pain
Opioids are powerful tools for pain. But they come with a hidden cost: they rob you of the most basic, automatic function your body performs every night-breathing. Sleep apnea isn’t just a nuisance for opioid users. It’s a silent killer that’s often ignored because it happens in the dark, when no one’s watching.
There’s no shame in needing pain relief. But there’s danger in assuming it’s safe. The science is clear: opioids and sleep don’t mix without risk. The good news? We know how to spot it. We know how to treat it. And we’re getting closer to safer alternatives.
Ask the questions. Get the test. Keep naloxone handy. Your breath-and maybe someone else’s life-depends on it.
Can opioids cause sleep apnea even if I’ve never had it before?
Yes. Opioids can trigger central sleep apnea in people with no prior history. This happens because opioids suppress the brain’s breathing center, leading to pauses in breathing during sleep. Studies show that 30-40% of long-term opioid users develop clinically significant sleep-disordered breathing, even if they didn’t snore or have apnea before starting the medication.
Is it safe to use a CPAP machine while on opioids?
Yes, but CPAP alone may not be enough. CPAP helps with obstructive sleep apnea by keeping the airway open, but it doesn’t fix central sleep apnea caused by opioids suppressing the brain’s breathing signal. Many patients need both CPAP and a reduction in opioid dose. In some cases, adding a breathing stimulant like acetazolamide or an ampakine (under medical supervision) may help.
Why do I wake up gasping for air after taking my opioid pain pill at night?
Taking opioids close to bedtime increases the risk of central apnea. As the drug peaks in your bloodstream during sleep, it depresses your brain’s breathing drive. Your body may stop breathing for 10-30 seconds, causing carbon dioxide to build up. When your brain finally detects the high CO2 level, it triggers a sudden gasp to restart breathing. This is a classic sign of opioid-induced central sleep apnea.
Can naloxone prevent overdose during sleep?
Naloxone can reverse an opioid overdose, even during sleep, if administered in time. But it won’t prevent the overdose from happening. It’s a rescue tool, not a shield. For people on high-dose opioids, having naloxone available and ensuring someone nearby knows how to use it is the best protection. Some experts now recommend prescribing naloxone to anyone taking more than 50 morphine milligram equivalents per day.
Are there safer pain medications than opioids for people with sleep apnea?
Yes. Non-opioid options like physical therapy, cognitive behavioral therapy for pain, NSAIDs (if safe for you), gabapentin, pregabalin, or antidepressants like duloxetine can be effective for chronic pain without suppressing breathing. For nerve pain, topical lidocaine or capsaicin patches may help. Always work with your doctor to find alternatives tailored to your condition and risk profile.
How do I know if my opioid dose is too high for my breathing?
Signs include waking up with headaches, feeling exhausted despite sleeping 8 hours, frequent nighttime awakenings, or being told you stop breathing while sleeping. A dose of 90 morphine milligram equivalents (MME) per day or higher is considered high-risk. The CDC recommends reducing doses below 50 MME when possible. If you’re unsure, ask for a sleep study and a medication review with your doctor.



January 26, 2026 AT 14:17
so like... are we sure this isn't just the government trying to make us all dependent on CPAP machines so they can sell us more gadgets? i mean, i took oxycodone for 3 years and never woke up gasping... unless you count when my ex left me. also, pulse oximeters are clearly rigged. i saw a guy on youtube say his read 98% while he was dead. 🤔