Acute Bronchitis: Causes, Treatments, and What Really Works
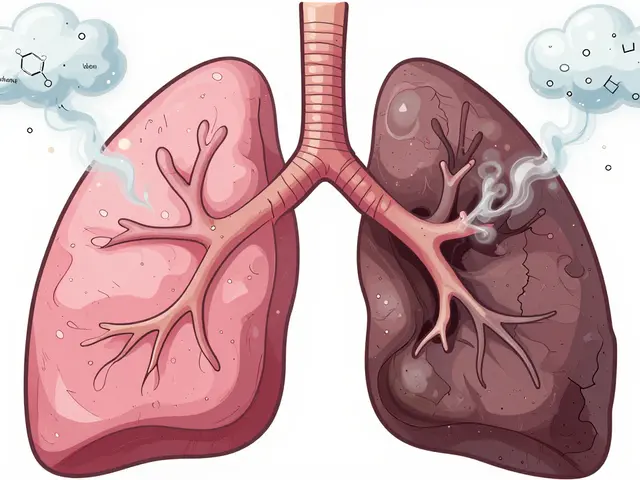
When you have a persistent cough, chest tightness, and mucus that won’t quit, you’re likely dealing with acute bronchitis, a short-term inflammation of the bronchial tubes that usually follows a cold or flu. Also known as viral bronchitis, it’s one of the most common reasons people visit the doctor — and one of the most often mismanaged. Unlike chronic bronchitis, which lasts months or years and is tied to smoking or pollution, acute bronchitis comes on fast, lasts a few weeks, and almost always starts with a virus — not bacteria.
Here’s the thing most people don’t know: antibiotics, medications designed to kill bacteria don’t work for most cases of acute bronchitis. The CDC says over 90% of cases are caused by viruses like rhinovirus or influenza. Taking antibiotics when they’re not needed doesn’t speed up recovery — it just increases your risk of side effects and contributes to drug-resistant infections. Yet, many patients still walk out with a prescription because they expect something strong. What actually helps? Rest, fluids, honey for cough relief, and sometimes a simple expectorant to loosen mucus. If you’re wheezing or short of breath, an inhaler might be more useful than pills.
Some people confuse acute bronchitis with pneumonia. The difference? Pneumonia hits the lung tissue itself and often comes with fever, chills, and sharp chest pain. Acute bronchitis stays in the airways — your cough is the main symptom, and it can hang around for 3 to 8 weeks, even after the virus is gone. That’s normal. Your airways are healing. Don’t panic if you’re still coughing after two weeks. But if you’re coughing up blood, have a fever over 100.4°F for more than a few days, or feel like you can’t catch your breath, that’s when you need to get checked.
There’s also a lot of noise around OTC cough syrups. Dextromethorphan? Often ineffective. Guaifenesin? Might help thin mucus, but don’t expect miracles. And yes, some of the posts below dive into how diphenhydramine, an antihistamine used in sleep aids and cold medicines shows up in cough formulas — but it’s not for bronchitis. It dries you out, which can make mucus thicker and cough worse. Same goes for many decongestants. They might help a stuffy nose, but they don’t fix the root problem.
What you’ll find below are real, practical guides from people who’ve been there. Posts that break down what works — like steam inhalation, staying hydrated, and when to skip the pharmacy altogether. Others explain why certain antibiotics like moxifloxacin, a broad-spectrum antibiotic sometimes misused for respiratory infections are rarely needed and carry risks. You’ll also see how sleep aids and antihistamines get tangled up in self-treatment, and why that’s a trap. This isn’t about quick fixes. It’s about understanding your body’s natural healing process — and not letting marketing or pressure push you into treatments that don’t belong.
Acute bronchitis is usually viral and doesn't need antibiotics. Learn how to manage the cough safely with rest, fluids, honey, and proven remedies-without unnecessary drugs.