Alzheimer’s disease: What you need to know
When talking about Alzheimer’s disease, a progressive neurodegenerative disorder that primarily affects memory and thinking skills. Also known as AD, it is the most common cause of dementia, a broader syndrome marked by a decline in cognitive function beyond normal aging. Understanding how this condition develops helps you spot early signs, evaluate treatment options, and plan for long‑term care.
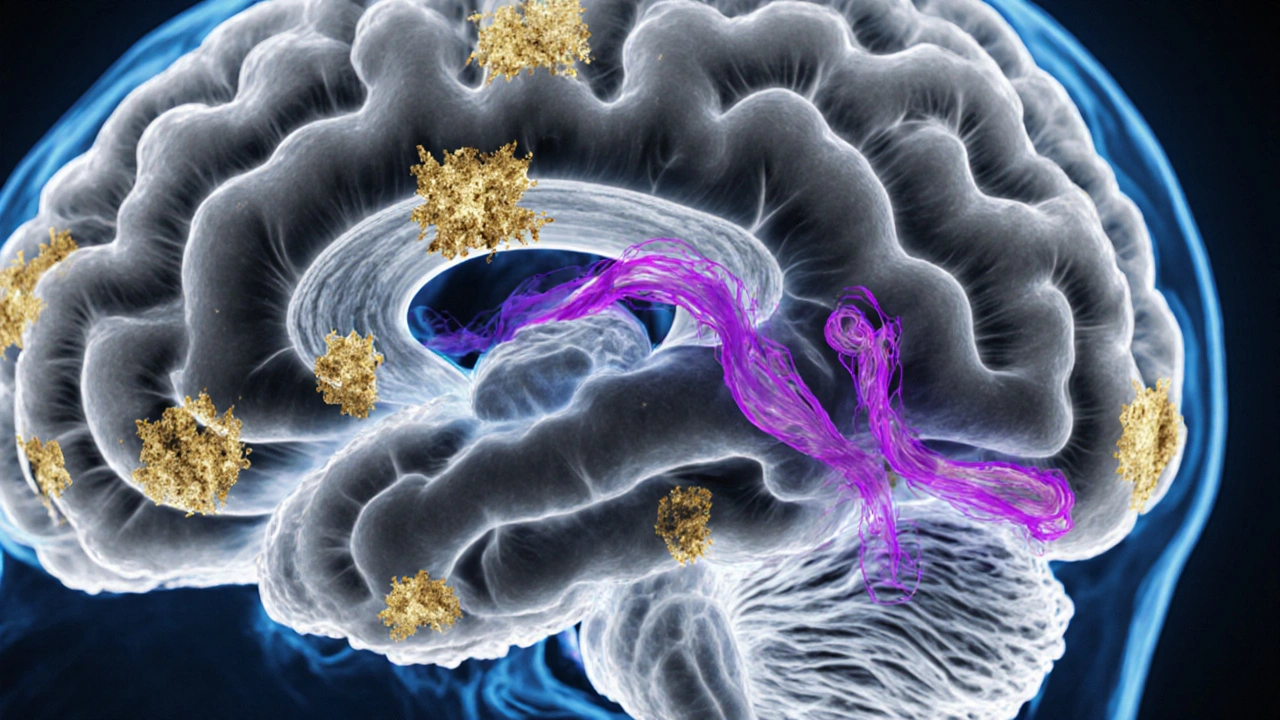
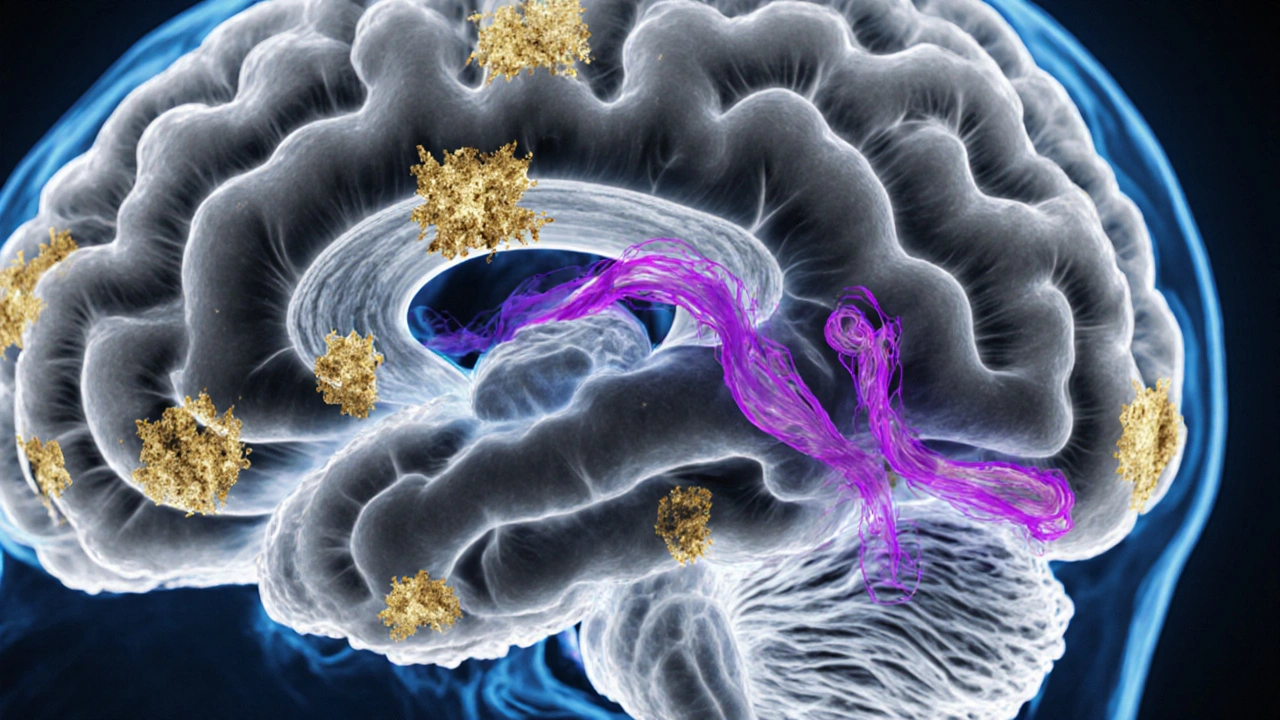
At the heart of the disease are two proteins that misbehave. Beta‑amyloid, tiny fragments that clump together to form sticky plaques outside neurons disrupt cell communication, while tau protein, normally a stabilizer inside neurons, twists into neurofibrillary tangles that break down the cell’s transport system. These processes trigger neurodegeneration, leading to the hallmark memory loss, language problems, and impaired judgment that define Alzheimer’s disease.
Risk factors and early detection
Age remains the strongest predictor—most diagnoses appear after 65. Genetics also play a role; the APOE‑ε4 allele raises risk, while rare mutations can cause early‑onset forms. Lifestyle choices matter too. Regular exercise, a Mediterranean‑style diet, and mental stimulation have been linked to slower progression. Monitoring subtle changes, like misplacing items in familiar places or difficulty finding words, can prompt a medical review before symptoms become severe.
Doctors use a combination of cognitive tests, brain imaging, and biomarker analysis to confirm the diagnosis. PET scans can visualize beta‑amyloid buildup, while cerebrospinal fluid tests measure its levels alongside tau. These tools help separate Alzheimer’s from other types of dementia and guide treatment decisions.
Currently approved medications fall into two main groups. Cholinesterase inhibitors, drugs that boost the neurotransmitter acetylcholine to improve memory and attention are used in mild to moderate stages. In later stages, NMDA‑type receptor antagonists such as memantine help regulate glutamate activity, reducing excitotoxic damage. While these drugs don’t cure the disease, they can modestly slow cognitive decline and improve daily function.
Beyond pharmaceuticals, non‑drug strategies are essential. Cognitive training, physical activity, and social engagement have shown measurable benefits. Caregiver support programs teach practical skills—managing medication, handling behavioral changes, and planning for future care—which can reduce stress and improve outcomes for both patients and families.
Research is racing ahead. Emerging therapies target the root causes: antibodies that clear beta‑amyloid plaques, tau‑directed vaccines, and gene‑editing approaches aimed at correcting genetic risk. Clinical trials are expanding, offering hope that disease‑modifying treatments will become available within the next decade.
Living with Alzheimer’s disease is a journey that touches every aspect of life. Early detection, a balanced mix of medication and lifestyle changes, and robust caregiver support create the best chance to maintain quality of life. Below you’ll find a collection of articles that dive deeper into each of these topics, from the science of beta‑amyloid to practical tips for daily caregiving. Keep reading to expand your understanding and find actionable insights you can use right away.
Learn the practical differences between Alzheimer's disease and Dementia of the Alzheimer's type, including definitions, diagnosis, treatment options, and common misconceptions.