Drug interactions: what to watch for
They can change how your medicines work or cause side effects. Knowing the common types and simple steps to reduce risk keeps you safer.
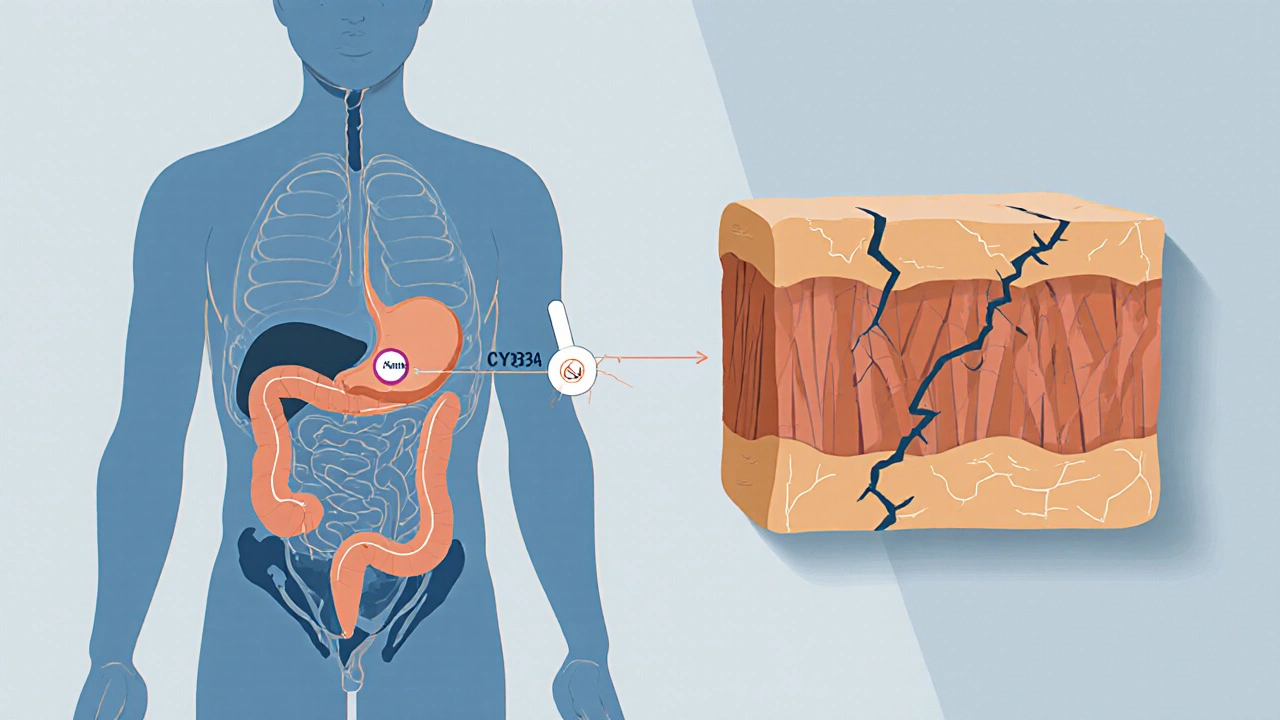
There are two main kinds of interactions. Pharmacokinetic interactions change how your body absorbs, distributes, breaks down, or removes a drug. For example, some antibiotics or antifungals block enzymes in the liver and let other drugs build up to dangerous levels. Pharmacodynamic interactions happen when two drugs affect the same body system in opposite or additive ways — like blood thinners plus anti-inflammatory drugs increasing bleeding risk.
Certain combinations are well known for trouble. Warfarin combines poorly with many antibiotics, antifungals, and herbal supplements such as St. John's wort. Statins and strong antibiotics or antifungals can raise the chance of muscle damage. Taking multiple sedatives — benzodiazepines, opioids, or sleep meds — can dangerously slow breathing. Mixing MAO inhibitors with certain antidepressants or foods high in tyramine can trigger severe blood pressure spikes.
How can you spot risky interactions quickly? Start by listing all medicines, including over-the-counter pain relievers, vitamins, herbal products, and eye drops. Use an online interaction checker from a medical site or ask your pharmacist to run the list. Watch for new symptoms after starting or changing a medicine: unusual bruising, severe dizziness, breathing changes, sudden muscle pain, or fainting are all red flags. If you notice these, get medical advice fast.
Simple steps reduce problems. Always tell every clinician and pharmacist about every drug and supplement you take. Use a single pharmacy when possible — pharmacists can catch dangerous pairs. Read medicine leaflets and check for warnings about other drugs, food, or alcohol. Avoid stopping a prescribed drug suddenly without advice; some medicines cause withdrawal or rebound effects.
Timing can matter. Some meds compete for absorption, so spacing doses a few hours apart helps. With certain blood pressure or diabetes drugs, stable timing and regular monitoring make interactions easier to catch. For antibiotics or antifungals that affect liver enzymes, your doctor may lower the dose of the other drug or choose a safer alternative.
Supplements and herbal remedies are not harmless. Many interact with prescription drugs. St. John's wort speeds the removal of many medicines, reducing their effect. Grapefruit juice blocks enzymes and raises blood levels of certain drugs. Tell your clinician about any supplement or juice you use regularly.
If you take high-risk drugs such as warfarin, lithium, digoxin, immunosuppressants, or some cancer drugs, expect more frequent blood tests and checks. Ask your provider what symptoms to watch for and when to call.
Drug interactions are common but manageable. With a solid medicine list, good communication with your pharmacist and prescriber, and basic attention to symptoms and timing, you can cut most risks and use medicines safely. Use a medication app to store doses and reminders, and carry a printed medicine list in your wallet for emergencies. If you feel worse after a med change, stop risky activities like driving and contact care immediately now.

Grapefruit juice can dangerously increase drug levels in your blood by blocking a key enzyme. Over 85 medications, including statins and blood pressure drugs, interact with it. Even small amounts can cause serious harm. Avoid it completely if you're on affected meds.
Pharmacodynamic drug interactions occur when drugs alter each other's effects at the target site, not by changing levels in the body. These can be deadly-like SSRIs with MAOIs-or lifesaving, like antibiotic combos. Know the risks.

Theophylline has a narrow therapeutic range and is easily affected by common medications like cimetidine, fluvoxamine, and allopurinol. Even small changes in metabolism can lead to life-threatening toxicity. Learn which drugs reduce clearance and how to prevent dangerous interactions.
Learn the difference between pharmacokinetic and pharmacodynamic drug interactions-how they work, why they matter, and how to avoid dangerous combinations. Real-world examples and expert insights.

As a patient or healthcare provider, it's crucial to be aware of Lamivudine drug interactions. Lamivudine is an antiviral medication commonly used to treat HIV and hepatitis B, but it can interact with other medications, potentially reducing its effectiveness or causing adverse side effects. To ensure safe and effective treatment, patients should inform their healthcare providers about all medications they are taking, including prescriptions, over-the-counter drugs, and supplements. Healthcare providers, in turn, should closely monitor patients on Lamivudine and adjust treatment plans accordingly. By staying informed and communicating openly, we can better manage our health and ensure the best outcomes possible.